Case Report - Biomedical Research (2017) Volume 28, Issue 11
Defection of phalanx: a complication of Bunnell's pulley reconstruction
Chao Lu1* and Guanglei Tian21Department of Orthopedics, the First Affiliated Hospital of Chongqing Medical University, Chongqing, PR China
2Department of Hand Surgery, Jishuitan Hospital, Beijing, PR China
- *Corresponding Author:
- Chao Lu
Department of Orthopedics
The first Affiliated Hospital of Chongqing Medical University, PR China
Accepted on April 10, 2017
Abstract
Objective: To report defection of phalanx under the reconstructed pulleys with Bunnell’s technique.
Methods: We followed up 26 reconstructed annular pulleys in 23 digits of 18 cases for 20 months and analysed the X-ray results of those phalanges. The function of pulley reconstruction was observed. The joint flexion and extension movement of the finger joint was recorded.
Results: All the reconstructed pulleys were healed. The efficacy was good. No bowstringing sign was found. The defections of phalanx were found in the areas of reconstructed pulleys in all cases. Narrowing of medullary cavities, osteophyte formation and thinning of cortex of phalanges were found in some cases with X-ray examination. The joint flexion and extension movement of the finger joint has improved.
Conclusion: Defection of phalanges will be found after Bunnell’s pulley reconstruction. It could be caused by pulley’s pressure which is converted from the traction load of the flexor tendon. Prognostic Studies, Level IV.
Keywords
Complication, Pulley reconstruction, Defection of phalanx.
Introduction
Compressive bone defects, also known as pressure erosion, are the defection that presented as bone surface pressed and absorbed. Peripheral soft tissue tumor compression or longterm collision of adjacent bones mostly causes it. Pulley reconstruction is an important surgery to prevent bowstring of flexor tendon and loss of Interphalangeal (IP) joint function [1]. Among all the techniques of pulley reconstruction, Bunnell’s procedure is the most common one. Several cases declare that there may be bone defection after pulley reconstruction [2-5]. To define the possibility of this complication, we followed up 18 cases and found that there will always be bone defection after Bunnell’s pulley reconstruction.
Materials and Methods
Study population
35 patients underwent Bunnell’s pulley reconstruction between 2001 to 2012 in our hospital. Only 18 of them (12 males and 6 females) were contacted. The data of those patients were collected. Age at surgery was 5 to 60 years old. The median following time is 20 months (4 to 114 months).
Surgical technique and rehabilitation
As Bunnell described [6], we used a free tendon graft obtained from the superficialis tendon of adjacent finger or the palmar plate to restore the pulleys [7]. The length of them were more than 5 mm. After the suture, we put the suture nodes on the lateral side of the finger. Drainage was extracted 48 h after the surgery. Flexion and extension exercise was encouraged in the first 4 weeks under the protection of an elliptic open aluminium ring preventing the pulley from over-loading. After that, the ring was moved and patients can use their fingers as normal.
Methods
Statement: This study was approved by the Institutional Review Board (IRB) and informed consent was obtained from each patient.
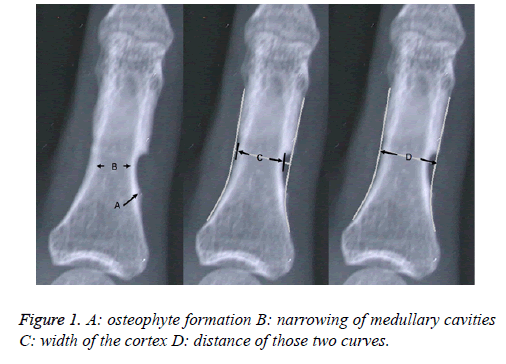
We got in touch with 18 patients, of who, 26 annular pulleys in 23 digits were reconstructed, and collected their X-ray films. On those X-ray films there were osteophyte formation, narrowing of medullary cavities, and thinning of cortex. First, we drew two curves to simulate the normal shape of the phalanges. Secondly, we measured the width of the cortex at the narrowest site and marked it as “C”. Then we measured the distance of those two curves at the same direction and marked it as “D”. After that we recorded the ratio of “C” and “D” (Figure 1).
Results
All the reconstructed pulleys were healed. No bowstringing sign was found. We can find all the phalanges had defections in the areas of reconstructed pulleys (Table 1). Narrowing of medullary cavities, osteophyte formation and thinning of cortex of phalanges were found in some cases (Figure 1). The joint flexion and extension movement of the finger joint has improved.
| Case number | Gender | Reconstructed pulley | Age | Following time (months) | C/D |
|---|---|---|---|---|---|
| 1 | Female | A1 (thumb) | 6 | 28 | 0.89 |
| 2 | Male | A2 (index finger) | 46 | 10 | 0.89 |
| 3 | Male | A2 (ring finger) A4 (ring finger) | 30 | 13 | 0.80/0.82 |
| 4 | Male | A2 (index finger) A2 (ring finger) | 21 | 26 | 0.84/0.65 |
| 5 | Male | A2 (ring finger) | 38 | 80 | 0.97 |
| 6 | Male | A2 (middle finger) | 29 | 7 | 0.79 |
| 7 | Female | A2 (ring finger) A4 (little finger) | 53 | 6 | 0.88/0.92 |
| 8 | Female | A2 (middle finger) | 37 | 4 | 0.9 |
| 9 | Female | A2 A4 (ring finger) A4 (little finger) | 41 | 7 | 0.80/0.90/0.81 |
| 10 | Male | A2 (little finger) | 60 | 14 | 0.9 |
| 11 | Male | A4 (little finger) | 12 | 13 | 0.83 |
| 12 | Male | A2 (index finger) A4 (ring finger) | 23 | 20 | 0.72/0.81 |
| 13 | Male | A2 (index finger) A2 (ring finger) | 23 | 114 | 0.87/0.78 |
| 14 | Male | A2 (index finger) | 15 | 55 | 0.94 |
| 15 | Female | A2 (ring finger) A4 (ring finger) | 10 | 24 | 0.85/0.92 |
| 16 | Female | A2 (middle finger) | 42 | 14 | 0.81 |
| 17 | Female | A2 (ring finger) | 25 | 39 | 0.86 |
| 18 | Male | A2 (little finger) | 23 | 53 | 0.93 |
Table 1. Post-operative record of pulley reconstruction.
Discussion
Even not well-known as re-rupture, stiffness, synovitis, and infection [8], bone defection may be the most common complication of Bunnell’s pulley reconstruction. In our research every phalange got defection under the reconstructed pulley in spite of age, gender, finger number and range of motion.
Sanger reported a case of bone defection in which a 55 years old female suffered from multiple pulley reconstruction [2]. The bone defection and fracture were observed under the pulley. They inferred that both the defection and the fracture were caused by multiple procedures on the blood supply and abnormal pressure of pulley. In our research bone defection was observed with none pulleys involved of multiple procedures or blood supply damage. That indicates the defection has nothing to do with times of surgery or blood supply of bone.
Conolly reported another case of bone defection in which a 7 years old boy got a fracture of phalange after the pulley reconstruction [3]. They stated that this complication was the result of the inability of the tendon graft to grow and the tightness of the tendon loop. In our research, bone defection happened in adult cases in spite of children.
Lin reported a case of a 35 years old male who got hourglassshaped bone resorption around the proximal phalanx under the reconstructed pulley [4]. They stated that the length of reconstructed pulley was not the same with the normal one which caused stress concentrated at a small area. They thought that was the reason of bone resorption and called it pressure erosion of the bone. We agree with the pressure erosion theory for the defection of the bone was also located underneath the pulleys with glass-hour like shape in our research. Diaphyseal narrowing remained the same in follow-up X-rays years later in both their research and ours. We also found osteophyte formation in our cases means the repairing ability of the bone is stable.
Ferran and Dias reported a case of a 27 year old female who got bone resorption only 7 months later after the pulley reconstructed [5]. In our research the same complication occurred from 4 to 114 months after surgery.
Palmer [9], and Leung [10] mentioned that tunnel of tendon graft in scaphoid and lunate may grow bigger or even fractured after years. Now we believed that it was the result of pressure erosion, just like what happened in our research.
Doyle and Blythe [11] suggested that we reconstruct the pulley through tunnel drilled in the base of phalanx in order to avoid increasing thickness of finger. That was rejected by Schneider [12] and Le [13] who believed that it would cause a fracture of phalanx. It seems that the latter opinion is right for it is easier to get fracture of drilling tunnel than Bunnell’s pulley reconstruction.
In this study we observed bone defection under reconstructed pulleys and it has nothing to do with gender, age, finger number or range of motion. It may happen before 4 months since the surgery was performed. We believe that it was caused by pressure erosion. But it needs more experiments to prove it. So does the mechanism and further influence.
References
- Peterson WW, Manske PR, Bollinger BA, Lesker PA, McCarthy JA. Effect of pulley excision on flexor tendon biomechanics. J Orthop Res 1986; 4: 96-101.
- Sanger JR, Buebendorf ND, Matloub HS, Yousif NJ. Proximal phalangeal fracture after tendon pulley reconstruction. J Hand Surg Am 1990; 15: 976-979.
- Conolly WB, Leicester AW. Fracture of the proximal phalanx. An unusual complication of pulley reconstruction in a child. J Hand Surg Br 1992; 17: 420-421.
- Lin GT. Bone resorption of the proximal phalanx after tendon pulley reconstruction. J Hand Surg Am 1999; 24: 1323-1326.
- Ferran NA, Dias JJ. Bone resorption of the proximal phalanx secondary to pulley reconstruction. J Hand Surg Eur Vol 2014; 39: 315-316.
- Bunnell S. Repair of tendons in the fingers and description of two new instruments. Surg Gynecol Obstet 1918; 26: 103-110.
- Alexander D. Flexor tendon pulley reconstruction. Oper Tech Orthop 1998; 8: 116-119.
- Wehbe MA, Mawr B, Hunter JM, Schneider LH, Goodwyn BL. Two-stage flexor-tendon reconstruction. Ten-year experience. J Bone Joint Surg Am 1986; 68: 752-763.
- Palmer AK, Dobyns JH, Linscheid RL. Management of post-traumatic instability of the wrist secondary to ligament rupture. J Hand Surg Am 1978; 3: 507-532.
- Leung PC, Hung LK. An effective method of reconstructing posttraumatic dorsal dislocated distal radioulnar joints. J Hand Surg Am 1990; 15: 925-928.
- Doyle BW. The finger flexor tendon sheath and pulleys: Anatomy and reconstruction. American Academy of Orthopaedic Surgeons. Symposium on tendon surgery in the hand. St Louis: CV Mosby 1975; 81-87.
- Schneider LH. Flexor tendons late reconstruction. Greens operative hand surgery. New York: Churchill Livingstone (4th edn.) 1999; 1922-1924, 1930-1937.
- Le VD, Samson P. Repair of finger flexor pulley-2. Current practice in hand surgery. London: Martin Dunitz 1997; 25-27.