Research Article - Journal of Neurology and Neurorehabilitation Research (2017) Volume 2, Issue 1
Current treatment status of adult brain tumors in the Philippine general hospital.
Ranhel C de Roxas1*, Karlo M Pedro1, Jonathan P Rivera2, Julette Marie F Batara1
1Department of Neurosciences, Philippine General Hospital, Philippine
2Department of Pathology, Philippine General Hospital, Philippine
- *Corresponding Author:
- Ranhel C de Roxas
Department of Neurosciences
Philippine General Hospital
Philippines
Tel: +639228010319
E-mail: rhainderoxas@yahoo.com
Accepted date: January 02, 2017
Citation: de Roxas RC, Pedro KM, Rivera JP, et al. Current treatment status of adult brain tumors in the Philippine general hospital. J Neurol Neurorehabil Res. 2016;1(2):22-28.
DOI: 10.35841/neurology-neurorehabilitation.2.1.1-7
Visit for more related articles at Journal of Neurology and Neurorehabilitation ResearchAbstract
Background: Brain tumors, although affecting only a small percentage of the population, poses a large impact worldwide with its high incidence of morbidity and mortality. In the turn of the century, we have witnessed major breakthroughs in the diagnosis and management of patients with brain tumors that is largely becoming molecular-based and personalized. In developing countries like the Philippines, major efforts are yet to be made in order to deliver the ideal treatment modalities to patients with brain tumor, yet certain socio-cultural factors and the lack of standardized protocol limit and even hinder this goal. Hence, it is important to be able to describe our patient population and to determine if they were able to receive adequate treatment in order to pave the way to further identification of ways to clinical improvement in the future. Objectives: This study aims to describe the clinical characteristics of patients diagnosed with brain tumors and to identify the different treatment modalities utilized to treat them in the Philippine General Hospital from January 2010 to December 2015. Methodology: Between 2010 and 2015, a total of 262 medical records of adult patients with brain tumors were successfully retrieved. The demographic data, clinical presentation, performance status, histopathologic diagnosis and treatment of all patients were recorded. The descriptive statistics using the STATA 13.0 software was used to summarize the data obtained. Results: Majority of the patients were females (59.2%) with a mean age of 41.7 years and a mean duration of symptoms of 13.2 months. The majority of the patients (66.8%) had a KPS of 80- 100. Headache, focal deficits, seizures and visual disturbances were the most common symptoms reported. Meningioma, Astrocytoma and glioblastoma were the most common histopathologic diagnosis. More than half of the patients received surgery alone (56.5%) but this is still lower than the expected number of patients who were advised to have surgery (60.7%). The use of combination therapy was found to be increasingly utilized within the duration of the study but a lower proportion of patients completed the planned treatment (13.1%). Around 10.5% of the patients only had regular follow-up to see if any progression in the tumor takes place. No intervention was done in 17.6% of patients who were noted to be either with poor prognosis, those who were lost to follow-up or those who had no consent to any intervention. Conclusion: In summary, there are multiple treatment modalities available to improve the outcome of patients with brain tumors. Although surgery alone remains to be the treatment of choice in majority of the patients, combination therapy was shown to have an increasing popularity. A lower proportion of patients received these treatment modalities than what was expected. Giving minimal or no intervention to the patient was already of decreasing trend in the institution. Further studies to determine the outcome after these treatment modalities on the patients diagnosed with brain tumors are deemed necessary in the future.
Keywords
Adult, Brain Tumors, Treatment modalities, Surgery, Chemotherapy, Radiotherapy
Background and Significance of the Study
Brain tumors is a large group of benign and malignant neoplasms arising from the brain parenchyma and its adjacent structures [1]. Though considered to be uncommon, with less incidence compared to neoplastic processes of the prostate, lungs, breast and colon, it is among the significant causes of cancer-related deaths [2,3]. It is associated with a high level of physical, neurological, cognitive and psychosocial changes [4]. The worldwide incidence of brain tumors is 3.4 to 18.6 per 100,000 and is reported to have an increasing trend in the last decades with higher incidence in developing countries. This geographic variation is attributed to the wide differences in socioeconomic and environmental factors but not fully elucidated due to limited registries [5].
In the literature, metastatic tumors remain to be the most common adult brain tumor followed by glioblastoma, astrocytoma and oligodendroglioma [6]. This is in contrast to the pediatric population where primary brain tumors such as astrocytoma, medulloblastoma and ependymoma remain to be more prevalent in the local setting [7]. The demographic characteristics of adult intracranial tumors in the Philippines is yet to be determined, hence, its full impact in our healthcare system cannot be completely described at present.
Treatment options for adult brain tumors are evolving and tends to be multidisciplinary. Since there is no standardized protocol in the treatment of the different adult brain tumors, the management of patients are based on different guidelines and studies and on the physician’s discretion. Surgery is usually the initial treatment and is generally attempted in most types of brain tumors. Its goals are to establish histologic diagnosis, to reduce intracranial pressures and sometimes to relieve seizures which are oftentimes intractable to anticonvulsants. The surgery may vary from a simple biopsy or insertion of a shunt or a complete or partial resection of the brain tumor [8]. Currently, radiation therapy, chemotherapy and targeted biological agents may also be treatment options depending on the histologic diagnosis and anatomical site of the brain tumor. Radiation therapy, which may be given in different forms such as conventional external beam radiation, brachytherapy or stereotactic radiosurgery, aims to shrink neoplastic cells sensitive to it while preserving the nearby normal brain cells. It is usually the first line of treatment in metastastic brain tumors and serves as an adjunct to surgery in primary brain tumors. On the other hand, chemotherapy is becoming an option as an initial treatment in chemosensitive tumors such as lymphoma, oligodendroglioma, anaplastic astrocytoma, glioblastoma, ependymoma and germ-cell tumors and as an adjunct therapy in large, unresectable tumors [9]. Targeted biological agents are also becoming a promising treatment option in brain tumors specifically in glioblastomas and high-grade gliomas by either interrupting the cell repair process fueling tumor growth or inhibiting the growth of new blood vessels or replacing faulty genes of the tumor cells [10]. Combination therapy of the aforementioned treatment strategies is usually utilized, however, active surveillance or regular monitoring of tumor progression is also offered in some patients with brain tumors who do not want to undergo the aforementioned treatment [11]
In our institution, approximately about a hundred patients with both primary and metastatic brain tumors are admitted for further management annually. However, there is no available local data on how these patients are being managed or if the various treatment options available are being utilized. Being able to describe the current treatment trends in managing brain tumors can give us an overview of the current clinical practice in the institution and can serve as a guide in how to improve treatment decisions in the future. This may also impact on the policies imposed in the hospital in order to be of further benefit in patients with brain tumors.
Objectives
General objective
This study aims to identify the different treatment strategies used to treat adult patients with brain tumors seen in the Philippine General Hospital from January 2010 to December 2015.
Specific objectives
1) To describe the clinical characteristics of patients diagnosed with brain tumors in a government tertiary hospital.
2) To describe the characteristics of the confirmed and unconfirmed cases of adult brain tumors.
3) To describe the utilization of different treatment options for adult brain tumors in a government tertiary hospital from 2010 to 2015.
Methodology
Study design and study population
This is a cross-sectional retrospective study from January 2010-December 2015. A review of the medical records of brain tumor patients admitted in the Philippine General Hospital was done. A total of 262 patients was included in the study as computed based from the total population and accuracy of 5%.
Sampling and randomization
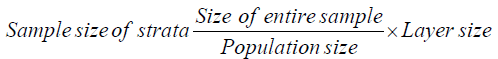
The sample size for each year was obtained using the stratified random sampling method. Proportionate stratification was used to ensure the representativeness of the samples for each year, wherein the number of samples for each year was proportionate to the population size of each stratum. The randomization for the selection of patients included in the study for each year was generated using a computer-generated random numbers.
The following stratified sampling formula was used: (Table 1)
| Strata (Year) | Size of entire sample | Population size | Layer size | Sample size for each stratum |
|---|---|---|---|---|
| 2010 | 262 | 758 | 119 | 41 |
| 2011 | 262 | 758 | 97 | 34 |
| 2012 | 262 | 758 | 108 | 37 |
| 2013 | 262 | 758 | 144 | 50 |
| 2014 | 262 | 758 | 134 | 46 |
| 2015 | 262 | 758 | 156 | 54 |
Table 1: The following stratified sampling formula was used.
Data collection
All patients at least 18 years of age admitted with a consideration or a definite diagnosis of brain tumor was obtained from the Adult Neurology census, Neurosurgery census, Tumor Clinic Census and the Surgical Pathology Unit of the Philippine General Hospital. The medical records of the patients included in the study were retrieved. Patients with missing charts were excluded from the study. The demographic data, clinical presentation, performance status, histopathologic diagnosis and received treatment of all patients were recorded (Appendix A).
Study analysis
Descriptive statistics was used to summarize the demographic and clinical profile of the patients included in the study. Frequency and proportion were used for categorical variables, while mean and standard deviation for interval/ratio variables. Missing data were neither replaced nor included in the analysis. All data analysis was performed using the STATA 13.0 software.
Ethical considerations
The study protocol was submitted to the University of the Philippines Research Ethics Board Panel for ethics review and approval. The study was conducted upon the approval of the reviewer panel. The anonymity of subjects, as well as the confidentiality of the data obtained, were assured by the researcher. All data were recorded only in writing. The results and patient information were kept strictly confidential by the primary investigator. A unique alphanumeric code was issued to each patient and their names did not appear on any of the data collection tools. Only the primary investigator had the full access to the patients’ names and other pertinent information, to ensure patient confidentiality at all times.
Results
A total of 262 patient records were reviewed from the Medical Records Section of the Philippine General Hospital. The age of the patients included in the study ranges from 18-80 years with a mean age of 41.7 years (median 41.5 years). Majority of patients were females (59.2%) and belonging to the 18-29 years age group (27.1%). More than half of the patients had no comorbidities (68.5%). The mean duration of symptoms was 13.2 months and more than a third of patients presented with headache followed by focal deficits, seizures, visual disturbances, hearing loss, memory problems, sensory deficits, behavioral changes, loss of consciousness, dysarthria and gait instability. Using the Karnofsky Performance Status (KPS) Scale, majority of patients still had good functional capacity with no special care needed (66.8%). Table 2 shows the clinical profile of all the brain tumor patients included in the study.
| Baseline Characteristics | Number (%) |
|---|---|
| Age | Mean: 41.7 ± 15.5 |
| 18-29 | 71 (27.1%) |
| 30-39 | 50 (19.1%) |
| 40-49 | 44 (16.8%) |
| 50-59 | 59 (22.5%) |
| >60 | 38 (14.5%) |
| Sex | |
| Male | 107 (40.8) |
| Female | 155 (59.2) |
| Marital Status | |
| Married | 137 (52.3) |
| Single | 113 (43.1) |
| Widow | 10 (3.8) |
| Others | 2 (0.8) |
| Educational attainment | |
| Elementary | 62 (23.7) |
| High school | 145 (55.3) |
| College | 54 (20.6) |
| Vocational | 1 (0.4) |
| Employment status | |
| Employed | 63 (24.0) |
| Self-employed | 24 (9.2) |
| Retired | 5 (1.9) |
| Unemployed | 170 (64.9) |
| Comorbidities | |
| None | 185 (68.5) |
| Hypertension | 40 (14.8) |
| Diabetes Mellitus | 12 (4.4) |
| Carcinoma | 12 (4.4) |
| Cerebrovascular Disease | 3 (1.2) |
| Others | 18 (6.7) |
| Clinical Presentation | |
| Headache | 142 (39.1) |
| Dysarthria | 1 (0.3) |
| Focal deficits | 80 (22.0) |
| Loss of consciousness | 2 (0.5) |
| Seizures | 63 (17.4) |
| Visual disturbances | 43 (11.8) |
| Memory problems | 9 (2.5) |
| Behavioral changes | 6 (1.7) |
| Sensory deficits | 7 (1.9) |
| Gait instability | 1 (0.3) |
| Hearing loss | 9 (2.5) |
| Duration of symptoms | Mean: 13.2 ± 24.6 |
| KPS score | |
| 0-40 | 8 (3.1) |
| 50-70 | 79 (30.1) |
| 80-100 | 175 (66.8) |
Table 2: Demographic characteristics and clinical profile of adult patients diagnosed with brain tumors.
The three most common sites of brain tumor in this study are the frontal lobe (33.6%), parietal lobe (14.5%) and the sellar area (11.1%). The diagnosis of the patients were histopathologically confirmed in 71% of the cases. Among these confirmed cases, meningioma is the most common tumor (45.1%) followed by astrocytoma (9.7%) and glioblastoma multiforme (7.5%). Among the unconfirmed cases by histopathology, metastasis is the most common consideration (43.4%, n=33). Table 3 shows the characteristics of the brain tumors included in the study.
| Number (%) | |
|---|---|
| Primary Site (Location) | |
| Brainstem | 6 (2.3) |
| Cerebellum | 22 (8.4) |
| Frontal | 88 (33.6) |
| Occipital | 4 (1.5) |
| Olfactory | 1 (0.4) |
| Parietal | 38 (14.5) |
| Pineal gland | 1 (0.4) |
| Pituitary and Craniopharyngeal duct | 29 (11.1) |
| Temporal | 19 (7.3) |
| Ventricle | 5 (1.9) |
| Skull Base | 18 (6.9) |
| Thalamus | 3 (1.1) |
| Multifocal | 26 (9.9) |
| Orbital | 2 (0.8) |
| Biopsy | |
| With biopsy | 186 (71.0) |
| Malignant | 37 (19.9) |
| Non-Malignant | 149 (80.1) |
| Without biopsy | 76 (29.0) |
| CNS Tumors by Histology | |
| Astrocytoma | 18 (9.7) |
| Choroid plexus tumors | 2 (1.1) |
| Craniopharyngioma | 9 (4.8) |
| Ependymoma | 7 (3.8) |
| Germinoma | 4 (2.2) |
| Glioblastoma | 14 (7.5) |
| Hemangioblastoma | 4 (2.2) |
| Hemangiopericytoma | 1 (0.5) |
| Lymphoma | 3 (1.6) |
| Medulloblastoma | 3 (1.6) |
| Meningioma | 84 (45.1) |
| Metastasis | 6 (3.2) |
| Oligoastrocytoma | 5 (2.7) |
| Oligodendroglioma | 7 (3.8) |
| Pituitary Adenoma | 7 (3.8) |
| Schwanomma | 12 (6.4) |
Table 3: Characteristics of adult brain tumors in the philippine general hospital.
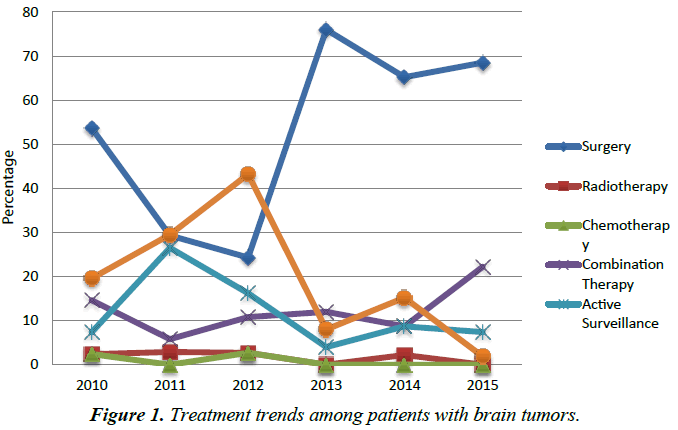
In terms of the treatment received by the patients, Table 4 shows a comparison between the planned treatment and the received treatment among patients diagnosed with brain tumors. More than half of the patients received surgery alone (56.5%) but this is still lower than the expected number of patients who were advised to have surgery (60.7%). Seventeen patients (6.5%), mostly with the consideration of brain metastases, were advised to have radiotherapy but only four patients received the actual treatment. A total of 59 patients (22.5%) were advised combination therapy (41=surgery + radiotherapy; 4=surgery + chemotherapy; 14=surgery + radiotherapy + chemotherapy) but only 34 patients completed the planned treatment. Around 10.5% of the patients only had regular follow-up to see if any progression in the tumor takes place. No intervention was done in 17.6% of patients who were noted to be either with poor prognosis, those who were lost to follow-up or those who had no consent to any intervention. Within the duration of the study, there was an increasing trend in the utilization of surgery alone among patients with brain tumor. Although the use of radiotherapy alone or chemotherapy alone was not shown to be commonly utilized in patients with brain tumor, the use of combination of surgery and/or radiotherapy and/ or chemotherapy was also shown to be of increasing value, although still lower than the expected percentage of patients who should receive the said treatment. There was also a notable decline in the use of active surveillance in patients with brain tumor. The trend of not doing any intervention was also shown to have decreasing trend (Figure 1, Appendix B).
| Planned Treatment | Received Treatment | |
|---|---|---|
| Surgery | 159 (60.7) | 148 (56.5) |
| Radiotherapy | 17 (6.5) | 4 (1.5) |
| Chemotherapy | 2 (0.8) | 2 (0.8) |
| Combination Therapy | 59 (22.5) | 34 (13.1) |
| Active Surveillance | 16 (6.1) | 28 (10.5) |
| None | 9 (3.4) | 46 (17.6) |
Table 4: Comparison between the planned versus received treatment among patients with brain tumors.
Meningioma, Astrocytoma and Glioblastoma were found to be the most common histopathologically confirmed brain tumors in this study. Patients with astrocytoma were found to be younger with a median age of 29.5 years compared to meningioma and glioblastoma with a median age of 43.5 and 51.5 years respectively. Meningioma was found to be more common in females than males while astrocytoma and glioblastoma does not seem to have sex predilection. Surgery alone was found to be the mainstay treatment in these tumors although there was also a large proportion of patients with astrocytoma and glioblastoma who received combination therapy (Tables 5-7). On the other hand, metastasis is the most common consideration among patients with no histopathologic confirmation. It was found in a wide age range of patients with a median age of 53 years. In this study, most of these patients were found to have undergone no intervention (Table 8).
| Number (%) | |
|---|---|
| Age | Mean: 43.9 (Range: 18-80 years old) |
| Sex | |
| Male | 21 (25.0) |
| Female | 63 (75.0) |
| Treatments received | |
| Surgery | 75 (89.2) |
| Radiotherapy | 0 |
| Chemotherapy | 0 |
| Surgery + Radiotherapy | 4 (4.8) |
| Active Surveillance | 5 (6.0) |
Table 5: Clinical profile of patients diagnosed with meningioma (n=84).
| Number (%) | |
|---|---|
| Age | Mean: 33.5 (Range: 18-65 years old) |
| Sex | |
| Male | 9 (50.0) |
| Female | 9 (50.0) |
| Treatments received | |
| Surgery | 10 (55.5) |
| Radiotherapy | 0 |
| Chemotherapy | 0 |
| Surgery + Radiotherapy | 5 (27.8) |
| Surgery + Radiotherapy + Chemotherapy | 3 (16.7) |
| Active Surveillance | 0 |
Table 6: Clinical profile of patients diagnosed with Astrocytoma (n=18).
| Number (%) | |
|---|---|
| Age | Mean: 49.3 (Range: 18-68 years old) |
| Sex | |
| Male | 8 (57.1) |
| Female | 6 (42.9) |
| Treatments received | |
| Surgery | 7 (50.0) |
| Radiotherapy | 0 |
| Chemotherapy | 0 |
| Surgery + Radiotherapy | 5 (35.7) |
| Surgery + Radiotherapy + Chemotherapy | 1 (7.1) |
| Active Surveillance | 0 |
| None | 1 (7.1) |
Table 7: Clinical Profile of Patients diagnosed with Glioblastoma (n=14).
| Number (%) | |
|---|---|
| Age | Mean: 49.0 (Range: 18-66 years old) |
| Sex | |
| Male | 18 (46.2) |
| Female | 21 (53.8) |
| Treatments received | |
| Surgery | 6 (15.4) |
| Radiotherapy | 3 (7.7) |
| Chemotherapy | 1 (2.6) |
| Radiotherapy + Chemotherapy | 2 (5.1) |
| Active Surveillance | 7 (17.9) |
| None | 20 (51.3) |
Table 8: Clinical Profile of Patients with metastatic brain tumors (n=39).
Discussion
First, this study described the clinical profile of patients diagnosed with brain tumors. The median age at diagnosis of brain tumor was found to be at 41.5 years of age, which is about two decades earlier than that recorded in other countries like the United States showing a median age of 59 years. It was also found to be less common in males with a male to female ratio of 0.69; this finding is at par with other countries with brain tumor registries such as the United States, South Korea and France [12]. Headache was found to be the most common manifestation of brain tumor occurring in 39.1% of patients in this study. In the study by Kirby et al. the headache in brain tumors tends to be intermittent, moderate to severe in intensity with variable character described as dull, aching, throbbing or shooting and usually more severe in the morning. It also tends to occur more frequently in midline and infratentorial tumors [13]. Other common symptoms are seizures and focal deficits which may occur in up to 30% of patients and are usually referable to the particular anatomic area of the brain affected [14]. The Karnofsy Performance Status scale is a widely used assessment tool to determine the functional status and to prognosticate patients with brain tumors. It is an 11-point scale with three states: A (100% to 80%) which corresponds to ability to work and proceed with normal activity, B (70% to 50%) which corresponds to inability to work with varying degree of assistance and C (40% to 0%) which corresponds to inability to care for one self with a requirement for hospitalization or institutional care. Despite the subjective nature of the tool, it serves as a salient factor in the decision-making on the treatment for the patient [15]. In this study, majority of the patients (66.8%) was found to have good functional status based on the KPS scale.
Secondly, this study determined the trend in the utilization of the different treatment options in brain tumors and if these treatments are being given to the patients. Surgery alone was found to be the preferred treatment in majority of the patients (56.5%). In the literature, it is the treatment of choice in many types of brain tumors such as meningioma, low-grade astrocytoma, craniopharyngioma, pituitary adenoma, hemangioblastoma and ependymoma [16]. Meningioma, being the most common brain tumor, is primarily managed with surgery alone. Being a slowgrowing tumor and sometimes, only presenting with minimal symptoms, active surveillance is also a reasonable option for some patients. However, higher grade meningioma such as anaplastic meningioma, which was seen in this study, may not be controlled with surgical resection alone. In a study by Sun et al. the debatable combination of surgery with adjuvant radiotherapy is already recommended and is associated with long-term tumor control [17].
As shown in this study, combination therapy is increasingly being utilized in brain tumors, although the rates shown are still lower than what is expected. In high-grade tumors such as hemangiopericytoma, anaplastic astrocytoma and glioblastoma, the addition of radiotherapy increases survival to six-fold compared to surgery alone [18]. Further addition of chemotherapy was found to increase the two-year survival by at least 6% and the relative risk reduction of death by 15% [19]. In lymphoma, various chemotherapeutic agents were shown to benefit patients although the addition of radiotherapy was shown to prolong overall survival and increase remission rates [20]. In choroid plexus tumors, the addition of radiotherapy with or without chemotherapy after subtotal surgical resection offers significant survival advantage [21]. In deep-seated tumors such as germinoma which are usually located in the pineal region, the use of radiotherapy alone, chemotherapy alone or the combination of both were found to have more than 85% cure rate [22].
Active surveillance or the watchful waiting approach is commonly chosen in other institutions especially in low-grade tumors such as oligodendroglioma, low-grade astocytoma and oligoastrocytoma. In this approach, patients were followedup with a repeat imaging and would only be offered tumor resection if there are already signs of tumor growth or malignant transformation. However, recent studies have shown that this approach offers lower median and overall survival compared to early tumor resection [23,24]. This could probably explain the reason of the decreasing trend of this approach in this study.
Limitations and Recommendations
There were several limitations to this study. The patients included in the study were only those admitted in the wards of the Philippine General Hospital, who were either referred to the Neurology and/or Neurosurgery services. This means that only those patients who were deemed admissible or were admitted for a procedure were included. Those patients who were never admitted or were just on regular follow-up in the outpatient clinics may be less represented in the study. Also, the extraction of the patient information was based on chart review, hence, some information which were not written in the chart were not be included.
This study is the first study to describe the patients with brain tumors, as well as the status of treatment utilization in our institution. This will pave the way to further studies in the future. The researchers would recommend to include the histopathologic staging in every diagnosis in the future series. Also, a more focused and detailed study on the outcomes of the most common tumors may also be helpful. A brain tumor registry is also deemed warranted because of the difficulty faced by the researchers in the manual extraction of the data from the medical records section of the hospital. Since the treatment of brain tumors is continuously evolving, it would be helpful to monitor the improvement in the utilization in the treatment options as this may serve as a guide for further hospital policy changes and easier multidisciplinary team communication.
Conclusions
In summary, there were already multiple treatment modalities offered to improve the outcome of patients with brain tumors. Although surgery alone remains to be the treatment of choice in majority of the patients, combination therapy was shown to have an increasing popularity. A lower proportion of patients received these treatment modalities than what was expected. Giving minimal or no intervention to the patient was already of decreasing trend in this institution. Further studies to determine the long-term outcome after these treatment modalities on the patients diagnosed with brain tumors are deemed necessary in the future.
References
- de Robles P, Fiest KM, Frolkis AD, et al. The worldwide incidence and prevalence of primary brain tumors: a systematic review and meta-analysis. Neuro Oncol. 2015;17:776-83.
- Wrensch M, Minn Y, Chew T, et al. Epidemiology of primary brain tumors: Current concepts and review of the literature. Neuro Oncol 2002;4(4):278-99.
- Siegel R, Ma J, Zou Z, et al. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9-29.
- Ford E, Catt S, Chalmers A, et al. Systematic review of supportive care needs in patients with primary malignant brain tumors. Neuro Oncol 2012;14(4):392-404.
- Tamimi AF, Tamimi I, Abdelaziz M, et al. Epidemiology of malignant and non-malignant brain tumors in Jordan. Neuroepidemiology 2015;45:100-108.
- Davis FG, Kupelian V, Freels S, et al. Prevalence estimates for primary brain tumors in the United States by behavior and major histology groups. Neuro Oncol 2001;3(3):152-158.
- Legaspi GD, Lagapa EP. Epidemiology of pediatric brain tumor in a tertiary hospital: A seven-year experience. Phil J Neurol 2006;10(2):65.
- Cloughesy T, Selch MT, Liau L. Brain. In: Haskell CM, editor. Cancer Treatment. 5th ed. Philadelphia, Pa: WB Saunders Co, 2001, pp. 1106-42.
- Soffietti R, Baumert BG, Bello L. European federation of neurological societies. Guidelines on management of low-grade gliomas: Report of an EFNS-EANO task force. Eur J Neurol 2010;17(9):1124-1133.
- Ewend MG, Elbabaa S, Carey LA. Current treatment paradigms for the management of patients with brain metastases. Neurosurgery 2005;57(5 Suppl):S66-77; discussion S1-4.
- Lallana EC, Abrey LE. Update on the therapeutic approaches to brain tumors. Expert Rev Anticancer Ther 2003;3(5):655-70.
- Ostrom QT, Gittleman H, Fulop J, et al. CBTRUS Statistical Report: Primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro Oncol 2015;17(s4):iv1-iv66.
- Kirby S, Purdy RA. Headaches, and brain tumors. Neurol Clin 2014;32(2):423Y432.
- Butowski NA. Epidemiology and diagnosis of brain tumors. Continuum (Minneap Minn). 2015;21(2 Neuro-oncology):301-13.
- Péus D, Newcomb N, Hofer S. Appraisal of the Karnofsky performance status and proposal of a simple algorithmic system for its evaluation. BMC Med Inform Decis Mak 2013;13:72.
- Maity A, Pruitt AA, Judy KD. Cancer of the central nervous system. In: Abeloff MD, Armitage JO, Niederhuber JE. Kastan MB, McKenna WG, editors. Abeloff’s Clinical Oncology. 4th ed. Philadelphia, Pa: Elsevier; 2008:1075-1136.
- Sun SQ, Hawasli AH, Huang J, et al. An evidence-based treatment algorithm for the management of WHO Grade II and III meningiomas. Neurosurg Focus 2015;38(3):E3.
- Rutkowski MJ, Jian BJ, Bloch O, et al. Intracranial hemangiopericytoma: Clinical experience and treatment considerations in a modern series of 40 adult patients. Cancer 2012;118(6):1628-36.
- Parisi S, Corsa P, Raguso A, et al. Temozolomide and radiotherapy versus radiotherapy alone in high grade gliomas: A very long term comparative study and literature review. Biomed Res Int. 2015;2015:620643.
- Roth P, Korfel A, Martus P, Weller M. Pathogenesis and management of primary CNS lymphoma. Expert Rev Anticancer Ther 2012;12(5):623-33.
- Bettegowda C, Adogwa O, Mehta V, et al. Treatment of choroid plexus tumors: A 20-year single institutional experience. J Neurosurg Pediatr 2012;10(5):398-405.
- Shibamoto Y. Management of central nervous system germinoma: Poposal for a modern strategy. Prog Neurol Surg 2009;23:119-29.
- Jakola AS, Myrmel KS, Kloster R, et al. Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA 2012;308(18):1881-8.
- Jakola AS, Unsgård G, Myrmel KS, et al. Surgical strategy in grade II astrocytoma: A population-based analysis of survival and morbidity with a strategy of early resection as compared to watchful waiting. Acta Neurochir (Wien) 2013;155(12):2227-35.