Research Article - Biomedical Research (2017) Volume 28, Issue 9
Curative effect of emergency care for patients with cerebral haemorrhage in Emergency Department
Ying Li1*, Yuqin Zhao1, Junling Zhang2, Yuming Zheng11Emergency Department, Binzhou People’s Hospital, Shandong, China
2Pediatrics Department (III), Binzhou People’s Hospital, Shandong, China
Accepted date: January 30, 2017
Abstract
Objective: To discuss the nursing effect of patents with cerebral haemorrhage in emergency department.
Methods: One hundred and twenty patients with cerebral haemorrhage were selected from July 2014 to July 2015 and randomly divided into a control group and an observation group according to case number. Patients in the control group were given conventional nursing, while patients in the observation group were treated by predictive nursing intervention measures besides conventional nursing. The clinical effect, incidence of complications, nursing satisfaction and prognosis were compared between the two groups.
Results: Compared to that of the control group, the incidence of complications of the observation group was much lower, and the difference had statistical significance (P<0.05); the nursing satisfaction degree of the observation group was higher than that of the control group, and the difference had statistical significance (P<0.05). Fugl-Meyer Assessment scale (FMA) score, Barthel Index (BI) and National Institutes of Health Stroke Scale (NIHSS) score of patients in the observation group were superior to those of patients in the control group, and the differences were statistically significant (P<0.05); the prognosis of the observation group was also better than that of the control group, and the difference was remarkably significant (P<0.05).
Conclusions: In the process of emergency treatment for patients with cerebral haemorrhage, the application of predictive nursing intervention is of great significance in lowering the incidence of complications, improving prognosis and enhancing living quality.
Keywords
Cerebral haemorrhage, Emergency department, Nursing effect.
Introduction
Cerebral haemorrhage induced by angiorrhexis in brain parenchyma and featured by sudden onset and high death rate has an incidence of 30% among stroke patients; cerebrovascular accident is its main cause [1,2]. It is manifested as nervous system impairments such as paralytic limbs, aphasia and disturbance of consciousness. It is usually seen among middle aged and elderly people with high blood pressure, intracranial vascular malformation and cerebral arteriosclerosis. With the aging of Chinese population, the incidence of cerebral haemorrhage has been higher and higher year by year [3,4]. Therefore, rapid, accurate and effective rescue for patients with cerebral haemorrhage and processing various symptoms are of great significance in the treatment of cerebral haemorrhage.
Predictive nursing, a new nursing concept proposed to adapt to modern nursing in recent years, refers to transforming passive rescue to active rescue by predicting the possible problems in disease course before and during nursing, confirming nursing key points and adopting effective prevention and treatment measures as soon as possible to reduce the pain of patients to the largest extent as well as complications [5-7]. This study selected 120 cerebral haemorrhage patients who received rescue, aiming to discuss the nursing effect on patients with cerebral haemorrhage in emergency department.
Materials and Methods
Research objects
One hundred and twenty patients who suffered from cerebral haemorrhage and received treatment in the Binzhou People’s hospital, Shandong, China, from July 2014 to July 2015, were selected as research subjects. All patients were confirmed having cerebral haemorrhage by brain Computed Tomography (CR), Magnetic Resonance Imaging (MRI), Digital Subtraction Angiography (DSA) and cerebrospinal fluid detection and they signed informed consent before study. They were randomly and evenly divided into two groups according to the case number.
Methods
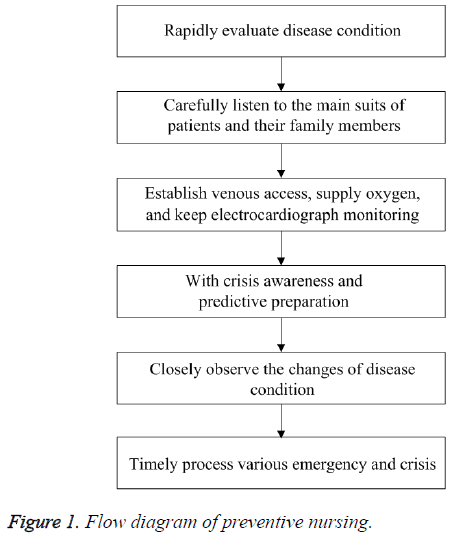
Patients in the control group were treated by conventional emergency nursing. After being admitted to the emergency room, the patients were given conventional emergency nursing measures such as oxygen inhalation, the observation of vital signs, transfusion, haemostasis and intracranial pressure reduction. Besides conventional emergency nursing, the observation group also received comprehensive and targeted predictive nursing intervention. The specific nursing measures were as follows. The first step was the monitoring of intracranial pressure. The temperature of brain was decreased using ice mat or ice cap. The sober patients took a lateral position and the bed was lifted for 15°~30°. The unconscious patients took a lateral position as well; the shock patients took a horizontal position to reduce the pressure bore by brain. Patients were infused with fluid or dripped with 20% mannitol. The dripping speed was controlled at 250 ml/30 min to prevent tissue necrosis induced by the crystallization or exosmosis of mannitol. Water-salt balance and acid-base balance were detected regularly. The next step was the monitoring of epilepsy. When there was a sign of epilepsy, the limbs of patients should be pressed in a proper strength. Towel or tongue depressor needed to be prepared to avoid bite wound. The next step was nursing for preventing upper gastrointestinal haemorrhage. The property and color of gastric juice were observed after surgery; gastrointestinal tract was given nutritional support and the injection of proton pump blocker to inhibit the secretion of gastric acid and protect gastric mucosa if there was no abnormality in the property and color of gastric juice. Next, nursing for preventing lung infection was performed. Firstly, nurses should make an accurate evaluation on the physical condition of patients, especially disturbance of consciousness and the property, quantity and color of sputum. For high-risk patients, basic nursing should be strengthened; besides, patients were assisted to take a lateral position or head turned to one side; nursing measures such as turning over, sputum suction and back slapping were given timely. The airway was processed by humidification nursing. The increase of body temperature and sputum might indicate the occurrence of lung infection; at that moment, sputum culture needed to be made timely and antibiotic drugs were selected for antiinfection treatment. The fifth step was nursing for preventing urinary system infection. 0.1% benzalkonium bromide solution was used to wash perineum, twice each day. For patients with retention catheterization, the bladder was washed by normal saline, once each day. Besides, the urine routine indexes of patients were reexamined regularly to prevent the occurrence of urinary system infection. The sixth step was nursing for preventing pressure sores. Patients with cerebral hemorrhage usually have physical disabilities; to prevent the incidence of pressure sores, the patients were assisted to turn over and guided to use air bed, the pressed part and bone bulge site were massaged or padded with soft pillows, and nutritional intake was strengthened. The last step was nursing for preventing intracranial rebleeding. The changes of consciousness and pupils were closely observed after surgery. If there was headache, emesis or the presence of fresh blood in drainage tube, the incidence of intracranial rebleeding should be paid attention to; at that moment, nurses should positively assist doctors to rescue patients. The detailed flow diagram is shown in Figure 1.
Evaluation indexes
Clinical effect was evaluated by Glasgow Outcome Scale (GOS) after treatment. GOS has five levels: good recovery, i.e., though with mild defect, patients could live normally; mild disability, i.e., though with disability, patients could work and live independently under assistance; severe disability, i.e., though disable and unable to live independently, patients had clear consciousness; vegetable state, i.e., few reactions; death.
Upper limbs reflex activity, coordinated and separation movement of flexor and extensor muscles, wrist function, hand function, coordination movement and speed movement were evaluated using simple Fugl-Meyer assessment scale (FMA): 0 point for complete non-function, 1 point for partial improvement, and 2 points for reflex or improvement. There were 33 events for upper limbs, totally 66 points. Better functions would gain higher scores.
Activities of daily living were evaluated using Barthel Index (BI). It was scored for 15, 10, 5 or 0 points according to the need of help and the degree of help. The total score was 100 points. A score lower than 20 points indicated the need of help in all aspects, a score between 20 and 40 points indicated the need of help in some aspects, and a score higher than 60 points indicated basically independent living.
Neurologic impairment was evaluated by National Institutes of Health Stroke Scale (NIHSS).
Statistical analysis
SPSS ver. 20.0 was used for data processing. Measurement data were expressed as mean ± Standard Deviation (SD) and processed by t-test; categorical data were expressed as percentage and processed by Chi-square test. Difference was considered statistically significant if P<0.05.
Results
In the control group (60 cases), they aged from 34 to 82 years old, bleeding volume ranged from 27 to 130 ml, and Glasgow Coma Score (GCS) ranged from 3 to 7 points. In the observation group (60 cases), they aged from 36 to 85 years old, bleeding volume ranged from 27 to 132 ml, and Glasgow Coma Score (GCS) ranged from 3 to 8 points. The differences of general data between the two groups had no statistical significance (P>0.05); hence the results were comparable (Table 1).
| Group | N | Male/female | Age (years) | Amount of bleeding (ml) | GCS (point) |
|---|---|---|---|---|---|
| Observation group | 60 | 36/24 | 62.48 ± 7.23 | 67.93 ± 24.51 | 5.33 ± 0.76 |
| Control group | 60 | 34/26 | 63.74 ± 6.63 | 67.93 ± 24.51 | 5.32 ± 0.71 |
Table 1: Comparison of general data between the two groups.
Comparison of FMA score, BI and NHISS score between the two groups after intervention
FMA score, BI and NHISS score of the observation group were much higher than those of the control group, and the differences had statistical significance (P<0.05). Specific data are shown in (Table 2).
| Group | FMA score | BI | NHISS score |
|---|---|---|---|
| Observation group | 52.60 ± 5.13 | 59.09 ± 6.98 | 16.93 ± 7.13 |
| Control group | 40.12 ± 4.31 | 48.45 ± 5.10 | 24.21 ± 7.52 |
| t | 7.96 | 5.4 | 3.97 |
| P | <0.05 | <0.05 | <0.05 |
Table 2: Comparison of FMA score, BI and NHISS score between two groups after intervention.
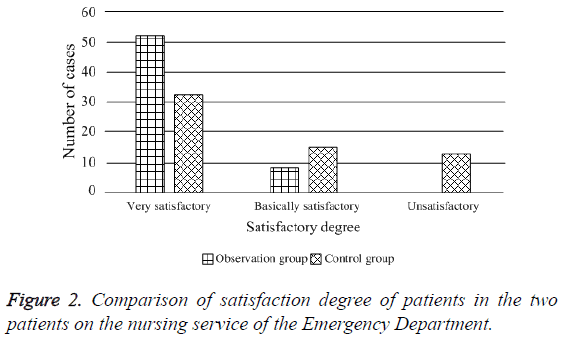
Nursing satisfaction of patients in the two groups
The investigation of the satisfaction of patients in the two groups on nursing in the emergency department suggested that, the satisfaction degree of the observation group was 100%; among them, 52 patients felt very satisfactory and 8 patients felt basically satisfactory; the satisfaction degree of the control group was 78.3%; among them, 32 patients felt very satisfactory, 15 patients felt basically satisfactory, and 13 patients felt unsatisfactory. The nursing satisfaction degree of patients in the observation group was much higher than that of the control group, and the difference had statistical significance (X2=11.06, P<0.05), as shown in Figure 2.
The comparison of incidence of complications between the two groups
The incidence of complications of the observation group was 16.7%; there were 4 cases of lung infection, 3 cases of hyperpyrexia and 3 cases of pressure sores. The incidence of complication of the control group was 66.7%; there were 14 cases of lung infection, 14 cases of hyperpyrexia and 12 cases of pressure sores. The difference between the two groups was statistically significant (X2=6.33, P<0.05).
The comparison of prognosis between the two groups
The prognosis effect of the observation group was superior to that of the control group, and the difference was statistically significant (P<0.05), as shown in Table 3.
| Group | Good recovery | Mild disability | Severe disability | Vegetable survival | Death |
|---|---|---|---|---|---|
| Observation group (N=60) | 41 (68.3) | 15 (25.0) | 1 (1.7) | 1 (1.7) | 2 (3.3) |
| Control group (N=60) | 23 (38.3) | 23 (38.3) | 3 (5.0) | 4 (6.7) | 7 (11.7) |
| X2 | 8.16 | 5.74 | 4.22 | 5.24 | 6.16 |
| P | <0.05 | <0.05 | <0.05 | <0.05 | <0.05 |
Table 3: Comparison of prognosis between two groups (N (%)).
Discussion
Cerebral haemorrhage, a kind of cerebral apoplexy, is a cerebral disease with high risks which is commonly seen among middle-aged and elder patients with high blood pressure. Cerebral haemorrhage refers to haemorrhage induced by angiorrhexis in brain parenchyma, and its causes include high blood pressure, intracranial vascular malformation and cerebral arteriosclerosis. It is usually induced by excitement or excessive use of strength. Therefore, cerebral haemorrhage generally occurs suddenly, is highly dangerous, and has a very high death rate. It is one of the fatal diseases for middle-aged and elder patients currently and ranks the first among the death causes for elder people [8,9]. Therefore, patients with cerebral haemorrhage need proper treatment and careful clinical nursing [10]. The role of nursing coordination has become more and more important in modern times. The modern nursing tends to be more professional and comprehensive. Conventional nursing has not been able to keep up with the pace of times due to multiple shortcomings. For example, conventional nursing is not targeted enough to assist patients with hypertensive cerebral haemorrhage; conventional nursing is usually carried out according to doctor's advice, which is difficult to satisfy the demand of patients and may affect patients’ satisfaction; due to the lack of initiative, it may not able to effectively prevent possible complications. Thus, more effective clinical nursing is needed to solve the above problems.
Predictive nursing refers to formulating nursing schemes based on the accurate evaluation on the physical and mental situations of patients; prevention before treatment is its principle [11]. Compare to conventional nursing, predictive nursing can turn nursing operation from passive to active, which provides guidance for the application of reasonable nursing measures and effectively reduces the incidence of postoperative complications. A study [12] demonstrates that, actively preventing the disease progress of patients with predictive nursing can significantly reduce risk factors and ensure the safety of patients.
Improving motor function and neurological function, enhancing living quality and reducing disability rate are the major objectives for the treatment of cerebral haemorrhage [13-16]. The research results suggested that, the scores of motor function, living quality and neurological function in the observation group were much higher than those of the control group, suggesting predictive nursing was positive to the prognosis of patients with high blood pressure and cerebral haemorrhage. Besides, it was also found that, the incidence of complications such as lung infection, hyperpyrexia and pressure sores were lower than that of the control group, suggesting predictive nursing could effectively reduce the incidence of complications and had great significance to the improvement of curative effect and nursing quality. As to the satisfaction degree, the satisfaction degree of the observation group reached 100%, and only two patients died in the observation group (3.3%), which was better than that of the control group (11.7%).
Conclusion
To sum up, nursing works is of great significance in the rescue of patients with cerebral haemorrhage. Timely application of predictive nursing can ensure the accuracy of disease condition determination, lower the incidence of complications, improve satisfaction degree, improve prognosis, and reduce death rate. Hence it is worth promoting.
Declaration of Interest
All authors declared there was no conflict interests involved.
References
- Qureshi AI, Ezzeddine MA, Nasar A, Suri MF, Kirmani JF, Hussein HM, Divani AA, Reddi AS. Prevalence of elevated blood pressure in 563, 704 adult patients with stroke presenting to the ED in the United States. Am J Emerg Med 2007; 25: 32-38.
- Hwang SK, Kim JS, Kim JH, Hong CK, Yang KH. Antihypertensive treatment of acute intracerebral hemorrhage by intravenous nicardipine hydrochloride:prospective multi center study. J Korean Med Sci 2012; 27: 1085.
- Sumer MM, Acikgoz B, Akpinar G. External ventricular drainage for acute obstructive hydrocephalus developing following spontaneous intracerbral haemorrhage. Neurol Sci 2002; 23: 29-33.
- Monies JM, Wong JH, Fayad PB, Awad IA. Stereotactic computed tomographic-guided aspiration and thrombolysjs of intracerebral hematoma: protocol and preliminary experience. Stroke 2000; 31: 834-840.
- Chen J. Experience of emergency nursing of 138 cases of cerebral haemorrhage. Chin Pract Med 2011; 6: 216.
- Wen XY, Jiao HY. Clinical application of predictive nursing in patients with acute cerebral hemorrhage. J Emerg Trad Chin Med 2006; 15: 104.
- Gao HW, Gao X. Impact of emergency nursing intervention on nerve function and life quality of survived patients with cerebral haemorrhage. J Clin Med Pract 2014; 12: 14-16.
- Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 2014; 383: 245-254.
- Wang WZ, Jiang B, Liu HM, Li D, Lu CZ, Zhao YD, Sander JW. Minimally invasive craniopuncture therapy vs. conservative treatment for spontaneous intracerebral haemorrhage: results from a randomized clinical trial in China. Int J Stroke 2009; 4: 11-16.
- Ding YH. Observation of effect of normalized emergency nursing intervention on acute cerebral haemorrhage. Mod Med Health 2014; 16: 2683-2684.
- Zhang HJ. Management of emergency nursing process of 87 cases of cerebral hemorrhage. Fertil Health 2014; 1: 60-61.
- Zhang MX, Shi YH. Effects of improved emergency nursing process on rescue effect of patients undergoing cerebral haemorrhage surgery. Mod Nurs 2013; 19: 3105-3107.
- Takahata H, Tsutsumi K, Baba H, Nagata I, Yonekura M. Early intervention to promote oral feeding in patients with intracerebral haemorrhage: a retrospective cohort study. BMC Neurol 2011; 11: 6.
- Geusgens CA, van Heugten CM, Cooijmans JP, Jolles J, van den Heuvel WJ. Transfer effects of a cognitive strategy training for stroke patients with apraxia. J Clin Exp Neuropsychol 2007; 29: 831-841.
- Wang LT, Jiang YM, Xu H, Li L, Ma SB, Zhang SR, Yang M, Wang X. Effects of rehabilitation training on limbs function recovery of patients with hypertensive cerebral haemorrhage after mini-invasive evacuation of hematoma. Chin J Phys Med Rehabil 2013; 35: 378-382.
- Poon MT, Fonville AF, Al-Shahi Salman R. Long-term prognosis after intracerebral haemorrhage: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2014; 85: 660-667.