Research Article - Journal of Public Health Policy and Planning (2019) Volume 3, Issue 1
Cost of family planning service in desie city administration, amhara regional state, Ethiopia
Biniyam Kassa*
Pathfinder International, Addis Ababa, Ethiopia
- Corresponding Author:
- Biniyam Mulat Kassa
Pathfinder International
Addis Ababa, Ethiopia
E-mail: kbin16@gmail.com
Accepted date: December 27, 2018
Citation: Kassa. Cost of family planning service in dessie city administration, amhara regional state, Ethiopia. J Public Health Policy Plann. 2018;3(1):1-9.
Abstract
The cost of providing family planning service and its potential burden on the economy is not clearly considered by most policy makers and government officials. The objective of this study is, to measure cost of Family Planning service provision in Dessie City Administration, Amhara regional state, Ethiopia. To carry out this research, facility-based cross-sectional study design which combines quantitative and qualitative techniques was employed. A stratified random sampling technique was used to select a total of 10 health facilities (4 governmental, 4 private and 2 NGO). Purposive sampling technique was used to select key informants and participants of focus group discussion. Analysis of Variance (ANOVA) was also used to explain comparison of mean cost across health facilities. The mean total cost of providing one unit of Family Planning service in all health facilities varies from ETB 10.44 ($0.45) for condom to ETB 227.53 ($9.76) for Jadell. On the other hand, cost per Couple Years of Protection (CYP) varies from ETB 9.66 ($0.41) for IUCD to ETB 130.38 ($5.6) for DMPA. Results of one-way ANOVA revealed that, there is a statistically significant difference between Governmental, Non-governmental and Private health facilities in the total cost of providing family planning service. Long-term FP services are the most efficient contraceptive methods as their cost per Couple Years of Protection is found to be lower in all health facilities.
Keywords
Cost of family planning service, unit cost of family planning, cost per CYP
Background
In Ethiopia, modern Family planning service was pioneered by the Family Guidance Association of Ethiopia (FGAE) and has been provided for more than a century with the generous support of humanitarian and development organizations from abroad [1,2]. Investing in family planning improves maternal and child health and also has benefits for Ethiopia across several sectors [3]. For example, fulfilling unmet need for family planning would generate significant cost savings in meeting five of the Millennium Development Goals (MDG), achieve universal primary education, reduce child mortality, improve maternal health, ensure environmental sustainability and combat HIV/AIDS, malaria, and other diseases [3]. Even though the Sustainable Development Goals (SDGs) make specific references to family planning in Goal [4] (Ensure healthy lives and promote well-being for all at all ages) and Goal [5] (Achieve gender equality and empower all women and girls), most of the SDGs will be benefited greatly from increased access to family planning service [5,6].
According to United Nation Population Division, globally donor assistance dedicated to family planning has decreased substantially in absolute dollar amounts in recent years, from $653 million in 1997 to $394 million in 2006. It is unclear how much additional funding was allocated to family planning through general budget support [7].
There have been some family planning cost studies and estimates of program costs, many of these are either old or rely on old data. There are inconsistencies in methodologies used making comparisons difficult [8]. Massive involvement and huge financial support of non-governmental organizations in the provision of family planning service hinders most government officials and health practitioners not to consider its cost and the potential burden that may arise on the overall economic activities. The cost of providing family planning service and potential burden of providing family planning service on the economy is not clearly considered by most policy makers and government officials. In additions, cost effectiveness and efficiency of different health facilities providing FP service in the study area is not known clearly.
In spite of searching effort in the study area, researches on cost of family planning service are limited or non-existent. Hence, this study estimates cost of family planning service in Dessie City Administration, South Wollo Zone, Amhara regional state Ethiopia.
Objectives
The general objective was to measure costs of Family Planning service provision in Dessie City Administration, Amhara regional state, Ethiopia.
The specific objectives are:
• To calculate unit cost of providing family planning service in different service providing health facilities found in Dessie City Administration.
• To calculate the cost per CYP for modern contraceptive methods in different service providing health facilities of Dessie city Administration.
Method and Materials
Study area
The study was conducted in Dessie city administration, Amhara regional state, Northeastern Ethiopia. The administrative center of this district is Dessie city, which is located 401 km to North of Addis Ababa, capital of Ethiopia.
Study period: This study was conducted from September 10 to October 10, 2017.
Study design: A facility-based cross-sectional study design which combines Quantitative and Qualitative data collection techniques was employed to carry out this research.
Source population: The source population for this study was all health facilities, health workers and administrative bodies of health facilities found in Dessie city administration.
Study population:
• Government owned, private owned and NGO owned health facilities found in Dessie city administration providing FP service.
• Health professionals providing family planning service in selected health facilities of Dessie city administration.
• Key informants working on Dessie city administration health office and health facilities. They include Dessie city administration health office head, finance department experts, Dessie city administration health office SRH/FP focal person, head of selected private and NGO owned clinics and finance department heads of NGO owned health facility.
Sampling size determination
According to Health Management Information System (HMIS) report of Dessie city Zonal Health Office, Dessie city administration has 12 government health facilities, 12 private health facilities and 6 NGO health facilities providing FP service. Health facilities were selected to ensure adequate representation of all variables under consideration in the study. For this study purpose, 30% of health facilities providing FP service found in Dessie City Administration were selected. Stratified random sampling technique was employed in order to address the complexity with private, government owned and NGO owned health facilities.
To this end, 4 health facilities from government owned, 4 health facilities from privately owned and 2 health facility from NGO owned were randomly selected among health facilities found in Dessie city Administration. Health facilities are used as a unit of analysis in this study. Within each sampled clinic, all health service providers working in sampled health facilities who provide family planning service found in the time of date collection were interviewed.
Three Focus Group Discussions (FGD) were conducted participating purposively selected health service providers from Go, NGO & Private health facilities separately. Each FGD had involved 6-7 purposively selected participants who involved in the provision of FP service in selected health facilities.
Key informant interviews were conducted with purposively selected 8 individuals. This include Dessie city administration health office head, finance department experts, Dessie city administration health office SRH/FP focal person, head of selected private and NGO owned clinics and finance department heads of NGO owned health facility.
Major records and documents in all selected health facilities such as client cards, laboratory log sheets, financial records/ payrolls, that are relevant in estimating cost of providing FP service, were reviewed. This document review was conducted retrospectively including 3 months’ data from June 1st 2017 to August 31, 2017.
Types of inputs coasted
Direct Costs include:
• Staff time for providing FP services; counseling and clinic visits.
• FP commodities cost; modern contraceptive method.
• Medical consumables and medical supplies cost.
• Laboratory testing cost.
• Physical infrastructures for FP service provision.
Indirect costs include:
• Administrative staff time.
• Supervision from regional or central level.
• Physical infrastructure for administering the program/ service.
• Other Miscellaneous costs (Public utilities, electricity, water, office supplies and consumables etc.).
The analysis was undertaken from the perspective of health facilities (i.e., health facilities) only. This implies that out-ofpocket costs incurred by FP clients (e.g. travel costs, opportunity cost of travel time, user fees for services or drugs, and other social costs) were not included in this study.
Costing approach
The study was focused on service provider side costs associated with FP service provision. The focus was unit cost analysis, defined as the cost of providing FP service for one client for one specific time. Cost per CYP, which is the cost of protecting couples for one year, was also calculated in this study. An ingredients approach which will focus on specific modern contraceptive methods was used to the costing analysis whereby quantities of each input was identified and prices were then attached to estimate their contribution to the overall cost.
Data processing and analysis
The quantitative data was first entered in to an excel sheet to make it ready for further processing and then it was analyzed using Statistical Package for Social Science (SPSS) version 20 software. The data was analyzed to identify the key cost drivers of each FP service delivery method. The analysis of the unit cost was based on the unit cost of inputs and client waiting time for specific contraceptive service. The data are presented as average costs and direct and indirect costs attributable to specific FP services. Costs were calculated in Ethiopian Birr (ETB) and converted to USD (United States Dollar) with an exchange rate of 1 USD=ETB 23.32 which was average exchange rate during the study period.
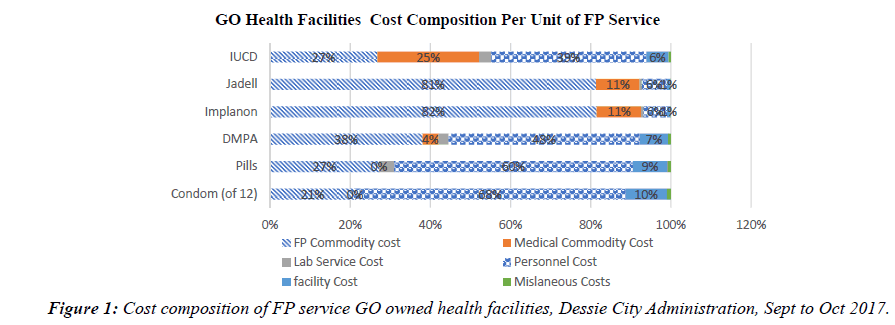
Overall mean cost of providing family planning service, mean costs of each contraceptive method was used to categorize findings. ANOVA analysis was also used to explain comparison of mean cost across groups (private, government & NGO owned health facilities). The Descriptive statistics was used to describe the data using frequency tables and figures (Figure 1).
The qualitative data collected using FGD and Key informant interview was used to support and triangulate findings of the quantitative study.
Results
Cost of family planning service
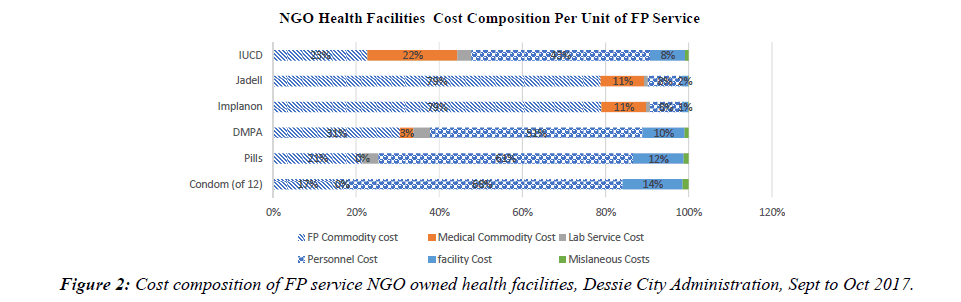
This study covered Ten Health facilities found in Dessie city Administration (4 government health facilities, 2 NGO owned health facilities, 4 Private health facilities). The primary focus of this study was estimating unit cost of providing FP service which is the sum total of specific costs (both direct and indirect costs) incurred to provide one unit of FP service for one client at a time. In this study, six elements of costs were considered as a contributor to the unit cos of FP service. Table 1 below explains specific mean costs attached to providing one unit of FP service in GO, NGO and Private Health facilities (Figure 2).
| Types of FP Costs | Health Facilities | Mean Cost of FP by Contraceptive Methods (ETB) | |||||
|---|---|---|---|---|---|---|---|
| Condom | Pills | DMPA | Implanon | Jadell | IUCD | ||
| Personnel cost | GO | 6.93 | 12.13 | 14.44 | 12.99 | 14.15 | 19.63 |
| NGO | 8.76 | 15.64 | 19.08 | 17.4 | 18.86 | 25.43 | |
| Private | 5.55 | 9.87 | 11.72 | 10.64 | 11.57 | 16.04 | |
| Laboratory service Related costs | GO | 0.00 | 0.75 | 0.75 | 1.29 | 1.48 | 1.58 |
| NGO | 0.00 | 0.88 | 1.13 | 1.56 | 1.56 | 1.75 | |
| Private | 0.00 | 2.73 | 5.18 | 5.03 | 6.27 | 5.43 | |
| Physical infrastructure costs | GO | 1.12 | 1.86 | 2.24 | 1.96 | 2.14 | 2.98 |
| NGO | 1.87 | 3.13 | 3.75 | 3.28 | 3.59 | 5 | |
| Private | 1.43 | 2.37 | 2.85 | 2.49 | 2.74 | 3.80 | |
| Miscellaneous costs | GO | 0.11 | 0.19 | 0.23 | 0.19 | 0.22 | 0.3 |
| NGO | 0.19 | 0.31 | 0.38 | 0.33 | 0.36 | 0.5 | |
| Private | 0.14 | 0.24 | 0.29 | 0.25 | 0.27 | 0.38 | |
| FP commodity Cost | All Facilities | 2.16 | 5.49 | 11.39 | 178.00 | 182.70 | 13.45 |
| Medical Supply cost | All Facilities | 0.00 | 0.00 | 1.20 | 24.37 | 24.37 | 12.80 |
| Total Cost of FP | GO | 10.32 | 20.42 | 30.23 | 218.81 | 224.96 | 50.73 |
| NGO | 12.98 | 25.56 | 37.28 | 225.37 | 231.88 | 59.17 | |
| Private | 9.29 | 20.73 | 32.62 | 220.78 | 227.92 | 52.65 | |
Table 1: Mean Costs of providing one unit of FP service (ETB) in GO, NGO & private health facilities, Dessie City Administration, Sept to Oct 2017.
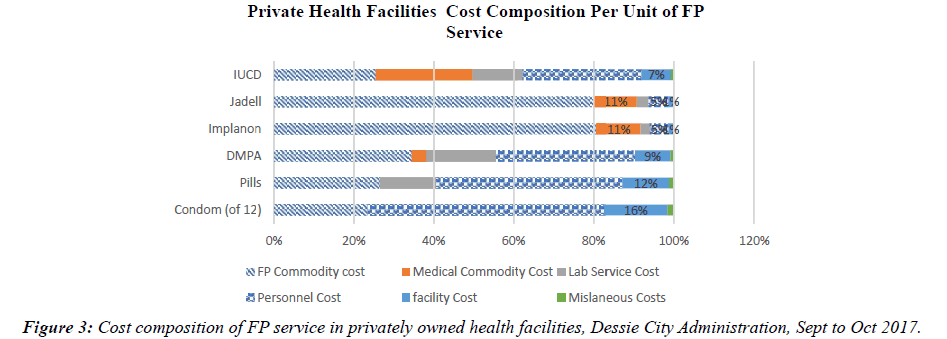
The mean total cost of FP service in GO health facilities Varies from ETB 10.31 ($0.44) for condom to ETB 224.95 ($9.65) for Jadell. On the other hand, the mean total cost of FP service in Private & NGO owned health facilities vary from ETB 9.28 ($0.4) and ETB 12.98 ($0.56) for condom to ETB 227.92 ($9.77) and ETB 231.88 ($9.94) for Jadell respectively (Figure 3).
Based on the findings of FGD and key informant interview, there was no significant variation among health facilities in the amount and type of medical supplies utilized for the provision of respective contraceptive methods included in this study. In this regard, the above listed costs were taken as an estimate of medical supplies cost attached to the provision of one unit of FP service for a client. There were no significant medical supplies utilized for the provision of Condom and Pills, whereas, provision of Implanon and Jadel takes the highest share of the cost ETB 24.37 ($1.04).
The main source of FP commodities for most Health facilities found in the study area is PFSA. To this end, the cost FP commodities (price of each FP commodities) was collected from this organization and uniformly taken as an estimate of FP commodity cost for all health facilities. Cost of FP commodities vary from ETB 2 ($0.09) for condom (for 12 pieces) to ETB 182.50 ($7.83) for Jadell.
The data revealed that, in all health facilities personnel cost takes the highest share for short term FP services followed by FP commodity cost. On the other hand, FP commodities cost takes the major share for long term FP services especially Implanon and Jadell (Figure 4).
Analysis of variance by total cost for one unit of FP service
So as to measure weather there is a significant variation in the total cost of providing family planning service by Government owned health facilities, NGO owned health facilities and privately owned health facilities, a one-way ANOVA was conducted. Result of ANOVA analysis for total cost of different contraceptive methods was depicted in Table 2 below.
| Sum of Squares | df | Mean Square | F | Sig. | ||
|---|---|---|---|---|---|---|
| ANOVA | ||||||
| Total Cost of Condom | Between Groups | 18.396 | 2 | 9.198 | 28.91 | 0 |
| Within Groups | 2.227 | 7 | 0.318 | |||
| Total | 20.623 | 9 | ||||
| Total Cost of Pills | Between Groups | 40.265 | 2 | 20.133 | 19.873 | 0.001 |
| Within Groups | 7.092 | 7 | 1.013 | |||
| Total | 47.357 | 9 | ||||
| Total Cost of DMPA | Between Groups | 66.228 | 2 | 33.114 | 16.08 | 0.002 |
| Within Groups | 14.416 | 7 | 2.059 | |||
| Total | 80.643 | 9 | ||||
| Total Cost of Implanon | Between Groups | 57.659 | 2 | 28.83 | 24.82 | 0.001 |
| Within Groups | 8.131 | 7 | 1.162 | |||
| Total | 65.79 | 9 | ||||
| Total Cost of Jadell | Between Groups | 64.924 | 2 | 32.462 | 9.688 | 0.01 |
| Within Groups | 23.456 | 7 | 3.351 | |||
| Total | 88.38 | 9 | ||||
| Total Cost of IUCD | Between Groups | 97.122 | 2 | 48.561 | 9.17 | 0.011 |
| Within Groups | 37.071 | 7 | 5.296 | |||
| Total | 134.193 | 9 | ||||
Table 2: ANOVA total cost of FP service (ETB) for GO, NGO & private health facilities, Dessie City Administration, Sept to Oct 2017.
There was a statistically significant difference between health facilities in the total cost of Condom as determined by one-way ANOVA (F=28.91, p<0.001). A Tukey post hoc test revealed that, total cost of providing one unit of condom was statistically significantly lower in Private Health facilities (9.28 ± 0.5 ETB, p=0.001) compared to NGO health facilities (12.98 ± 0.39 ETB, p=0.02). however, there was no statistically significant difference between private and Government health facilities (p=0.08) in the total cost of providing one unit of condom.
There was a statistically significant difference between health facilities in the total cost of Pills as determined by one-way ANOVA (F=19.87, p=0.001). A Tukey post hoc test revealed that the total cost of providing one unit of Pills was statistically significantly lower in Government Health facilities (20.41 ± 0.92 ETB, p=0.001) as compared to NGO health facilities (25.56 ± 0.9 ETB, p=0.001) but there was no statistically significant difference between private and Government health facilities (p=0.91).
There was a statistically significant difference between health facilities in the total cost of DMPA as determined by one-way ANOVA (F=16.08, p=0.002). A Tukey post hoc test revealed that the total cost of providing one unit of DMPA was statistically significantly lower in Government Health facilities (30.22 ± 0.78 ETB, p=0.001) as compared to NGO health facilities (37.27 ± 1.13 ETB, p=0.002). However, there was no statistically significant difference between private and Government health facilities (p=0.112) in the total cost of providing DMPA for clients (Figure 5).
There was a statistically significant difference between health facilities in the total cost of Implanon as determined by one-way ANOVA (F=24.82, p=0.001). A Tukey post hoc test revealed that the total cost of providing one unit of Implanon was statistically significantly lower in Government Health facilities (218.80 ± 0.96 ETB, p=0.001) as compared to NGO health facilities (225.37 ± 1.03 ETB, p=0.001). However, there was no statistically significant difference between private and Government health facilities (p=0.08) in the total cost of providing Implanon for clients (Figure 6).
There was a statistically significant difference between health facilities in the total cost of Jadell as determined by oneway ANOVA (F=9.68, p=0.01). A Tukey post hoc test revealed that the total cost of providing one unit of Jadell was statistically significantly lower in Government Health facilities (219.8 ± 1.02 ETB, p=.006) as compared to NGO health facilities (231.88 ± 1.13 ETB, p=0.008). However, there was no statistically significant difference between private and Government health facilities (p=0.123) in the total cost of providing Jadell for clients.
There was a statistically significant difference between health facilities in the total cost of IUCD as determined by oneway ANOVA (F=9.17, p=0.011). A Tukey post hoc test revealed that the total cost of providing one unit of IUCD was statistically significantly lower in Government Health facilities (50.72 ± 1.16 ETB, p=0.009) as compared to NGO health facilities (59.17 ± 1.52 ETB, p=0.009). But, there was no statistically significant difference between private and Government health facilities (p=0.5) in the total cost of providing IUCD for clients.
Cost per couple years of protection (CYP)
This section uses the information on total cost of providing FP service presented in previous sections to determine the costs per CYP for different methods provided by different delivery systems. To estimate cost of FP service per CYP, the conversion factors of each contraceptive method to produce one unit of CYP was used as depicted in Ethiopian Federal Ministry of Health FP guideline. Quantity required to produce a unit of CYP was attached to the total cost of FP service and cost per CYP of each contraceptive method was produced. The cost per CYP of each FP service is explained in Table 3 below.
| List of Contraceptives | GO | NGO | Private | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std. Dev | Mean | Std. Dev | Mean | Std. Dev | Mean | Std. Dev | |
| Condom | 103.1725 | 3.93651 | 129.8100 | 5.16188 | 92.7650 | 7.06598 | 104.3370 | 15.13544 |
| Pills | 91.8725 | 2.95457 | 115.0400 | 4.18607 | 93.1650 | 5.77107 | 97.0230 | 10.31988 |
| DMPA | 120.9125 | 3.14898 | 149.1200 | 4.55377 | 130.4750 | 7.75000 | 130.3790 | 11.97970 |
| Implanon | 109.4000 | .47979 | 112.6900 | .52326 | 110.3900 | .59950 | 110.4540 | 1.35409 |
| Jadell | 64.2725 | .29182 | 66.2500 | .32527 | 65.1225 | .71756 | 65.0080 | 0.89488 |
| IUCD | 9.2225 | .21313 | 10.7550 | .27577 | 9.5700 | .58344 | 9.6680 | 0.70150 |
Table 3: Cost Per CYP of FP service (ETB) for GO, NGO & private health facilities, Dessie City Administration, Sept to Oct 2017.
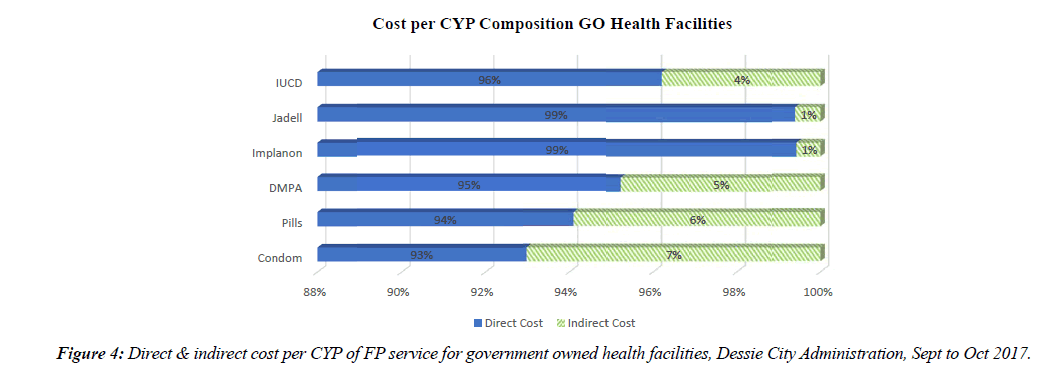
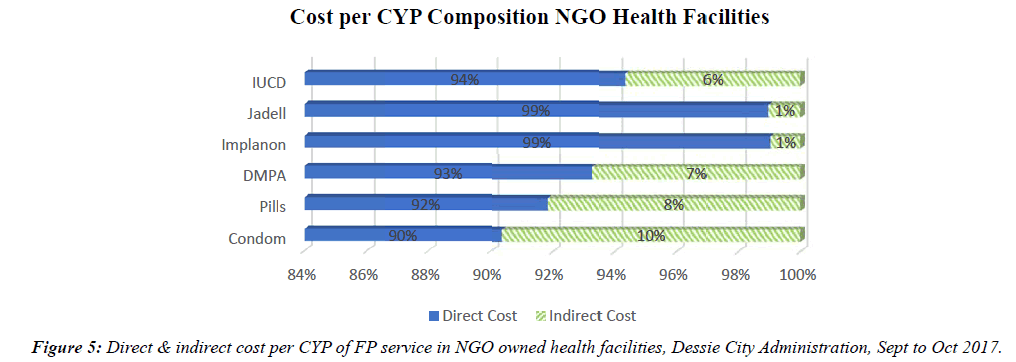
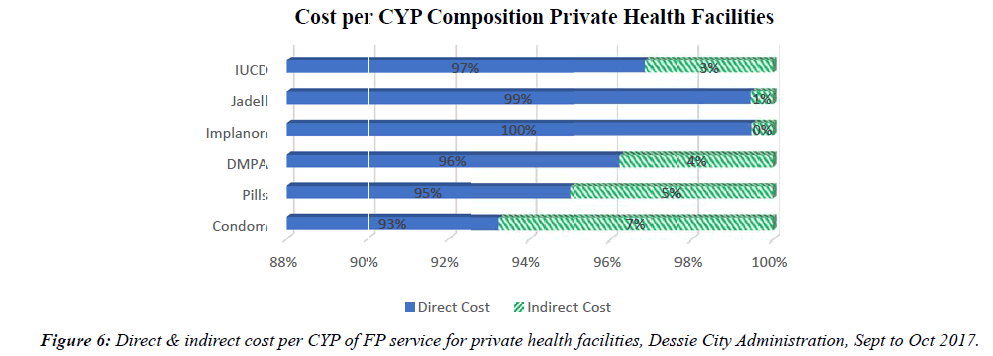
The study revealed that short term FP methods such as Condom, Pills and DMPA had the highest indirect costs in GO, NGO and private health facilities accounting 4% to 10% of the total cost of producing a unit of CYP. The reason for this is the frequency with which a client can or will have to visit the health facilities so as to generate one unit of CYP using those short term FP methods. The FP service with the lowest percentage of indirect cost was Implanon, Jadell and IUCD which generates more than one unit of CYP from a single service as a result their proportion of indirect cost was lower than those of short term FP methods.
Analysis of variance by cost per CYP: In order to measure weather there is a significant variation in the cost per CYP of providing family planning service by Government owned health facilities, NGO owned health facilities and privately owned health facilities, a one-way ANOVA was conducted. Result of ANOVA analysis for Cost per CYP of different contraceptive methods was depicted in Table 4 below.
| ANOVA | ||||||
|---|---|---|---|---|---|---|
| Sum of Squares | df | Mean Square | F | Sig. | ||
| Cost Per CYP of Condom | Between Groups | 1838.816 | 2 | 919.408 | 28.871 | .000 |
| Within Groups | 222.918 | 7 | 31.845 | |||
| Total | 2061.734 | 9 | ||||
| Cost Per CYP of Pills | Between Groups | 814.872 | 2 | 407.436 | 19.857 | .001 |
| Within Groups | 143.627 | 7 | 20.518 | |||
| Total | 958.499 | 9 | ||||
| Cost Per CYP of DMPA | Between Groups | 1060.946 | 2 | 530.473 | 16.098 | .002 |
| Within Groups | 230.672 | 7 | 32.953 | |||
| Total | 1291.618 | 9 | ||||
| Cost Per CYP of Implanon | Between Groups | 14.459 | 2 | 7.230 | 24.776 | .001 |
| Within Groups | 2.043 | 7 | .292 | |||
| Total | 16.502 | 9 | ||||
| Cost Per CYP of Jadell | Between Groups | 5.301 | 2 | 2.651 | 9.735 | .010 |
| Within Groups | 1.906 | 7 | .272 | |||
| Total | 7.207 | 9 | ||||
| Cost Per CYP of IUCD | Between Groups | 3.195 | 2 | 1.598 | 9.067 | .011 |
| Within Groups | 1.234 | 7 | .176 | |||
| Total | 4.429 | 9 | ||||
Table 4: ANOVA table cost per CYP of FP service (ETB) for GO, NGO & private health facilities, Dessie City Administration, Sept to Oct 2017.
As we can understand from the above tables, there was a statistically significant difference between health facilities in the cost of producing one unit of CYP from Condom as determined by one-way ANOVA (F=28.87, p<0.001). A Tukey post hoc test revealed that, total cost of producing one unit of CYP from condom (120 units of condom=1 CYP) was statistically significantly lower in private Health facilities (92.76 ± 4.88 ETB, p=0.000) compared to NGO health facilities (129.81 ± 4.88 ETB, p<0.01). There was no statistically significant difference between private and Government health facilities (p=0.079) in the cost per CYP of condom.
There was a statistically significant difference between health facilities in the cost of producing one unit of CYP from Pills as determined by one-way ANOVA (F=19.85, p=0.001). A Tukey post hoc test revealed that, the cost of producing one unit of CYP from Pills (13 Cycle=1 CYP) was statistically significantly lower in Government Health facilities (91.87 ± 2.9 ETB, p=0.001) as compared to NGO health facilities (115.04 ± 4.18 ETB, p=0.001). However, there is no significant variation between private and government health facilities (p=0.915) in the cost per CYP of pills.
There was a statistically significant difference between health facilities in the cost of producing one unit of CYP from DMPA as determined by one-way ANOVA (F=16.098, p=0.002). A Tukey post hoc test revealed that the cost of producing one unit of CYP from DMPA (4 doses (mL)=1 CYP) was statistically significantly lower in Government Health facilities (120.91 ± 3.14 ETB, p=0.002) as compared to NGO health facilities (149.12 ± 4.5 ETB, p=0.002). However, there is no significant variation between private and government health facilities (p=0.112) in the cost per CYP of DMPA.
There was a statistically significant difference between health facilities in the cost of producing one unit of CYP from Implanon as determined by one-way ANOVA (F=24.77, p=0.001). A Tukey post hoc test revealed that the cost of producing one unit of CYP from Implanon (2 CYP per Implanon) was statistically significantly lower in Government Health facilities (109.4.32 ± 0.479 ETB, p=0.001) as compared to NGO health facilities (112.69 ± 0.523 ETB, p=0.001). However, there is no significant variation between private and government health facilities (p=0.81) in the cost per CYP of Implanon.
There was a statistically significant difference between health facilities in the cost of producing one unit of CYP from Jadell as determined by one-way ANOVA (F=9.735, p=0.01). A Tukey post hoc test revealed that the cost of producing one unit of CYP from Jadell (3.5 CYP per Jadell) was statistically significantly lower in Government Health facilities (64.27 ± 0.29 ETB, p=0.008) as compared to NGO health facilities (65.122 ± 0.71 ETB, p=0.008). However, there is no significant variation between private and government health facilities (p=0.121) in the cost per CYP of Jadell.
There was a statistically significant difference between health facilities in the cost of producing one unit of CYP from IUCD as determined by one-way ANOVA (F=9.067, p=0.011). A Tukey post hoc test revealed that the cost of producing one unit of CYP from IUCD (5.5 CYP per IUCD) was statistically significantly lower in Government Health facilities (9.22 ± 0.213 ETB, p=0.01) as compared to NGO health facilities (10.75 ± 0.27 ETB, p=0.01) but, there is no statistically significant variation between Government health facilities and Private Health facilities (p=0.5).
Discussion
Unit cost of Providing Short term FP service in NGO health facilities exceeds the cost of providing same service in GO health facilities in average by 25% (26% for Condom, 25% for Pills & 23% for DMPA). However, for Long term FP service, unit cost of provision in NGO health facilities requires an average of 8% more cost (3% for Implants & Jadell and 18% for IUCD) than GO health facilities to get same service.
Unit cost of Providing Short term FP service in Private health facilities exceed the cost of providing same service in GO health facilities in average by 7% (10% for DMPA and 3% for Pills). However, for Long term FP service, unit cost of provision in Private health facilities requires an average of 8% more cost (3% for Implants, 3% Jadell and 17% for IUCD) than GO health facilities to get same service. This might be due to the difference in the personnel cost and physical infrastructure related costs of FP in different health facilities.
The cost of generating one unit of CYP from Short term FP service in NGO health facilities exceeds the cost of generating same CYP in GO health facilities in average by 25% (26% for Condom, 25% for Pills & 23% for DMPA). This result is slightly different from results of same study conducted in Kenya which revealed cost per CYP of Short term FP methods in NGO health facilities exceeds the cost per CYP in GO health facilities in average by 34% (21% for Condom, 31% for Pills & 49% for DMPA) [9].
On the other hand, this study depicts unit cost of producing one unit of CYP from Long term FP methods in NGO health facilities incurs an average of 8% more cost (3% for Implanon & Jadell and 17% for IUCD) than GO health facilities which is closer as compared to previous study conducted in Kenya which is, NGO health facilities incurs an average of 11% more cost (3% for Implants and 18% for IUCD) than GO health facilities [9].
Unit cost of generating one unit of CYP using Long term FP methods in Private health facilities incurs an average of 2% more cost (1% for Implants, 1% Jadell and 4% for IUCD) than GO health facilities. However, there is no significant difference in the cost of producing a unit of CYP from short term FP service both in Private and government health facilities. Similar study conducted in Ethiopia in 2010 indicated that, there is no significant difference in the cost per CYP for Long term FP services between private and GO health facilities but, there exists a 2% (3% for Condom, 3% for Pills & 1% for DMPA) reduction in Private health facilities in the cost of producing a unit of CYP using short term FP service [9].
In all health facilities, unit cost of providing Short term FP service is higher than unit cost of providing Long-term FP services. To the contrary, cost of generating one unit of CYP from Short term FP service is higher than cost of generating one unit of CYP from Long term FP services. The average cost of generating one unit of CYP from Short term FP services is estimated as ETB 110.58 ($4.74), whereas, the average cost of generating one unit of CYP from Long term FP services is ETB 61.71 ($2.65) which is significantly lower than cost per CYP of Short term FP Services. In similar study conducted in Ethiopia in 2010, the average cost per CYP for short term FP services was estimated as $4.92 and the average cost per CYP for Long term FP services was $4.57 which is slightly greater than findings of this research [9]. In another study conducted in Mali, the cost per CYP for Short term FP services was estimated to be $7.17 and for Long term FP service it was estimated as $8.5111. The variation in estimating personnel cost of FP service and FP commodity cost during the study period contributed for this variation between the two studies.
Out of the total cost per CYP generated from Long term FP service, 17% was related to personnel costs and the remaining 83% was attached to FP commodity, medical supply and other costs. In a slight similar fashion, previous study conducted in Ethiopia revealed that, personnel cost attached to Cost Per CYP for Long term FP service was reported as 21% and FP commodity related costs accounts for 79% of the total cost per CYP for Long term FP services [9]. Where as in a study conducted in Kenya & Mali, personnel cost related to cost per CYP generated from Long Term FP service was found to be 47% & 48% respectively and commodity related costs accounts for 53% & 52% of the total cost per CYP for Long term FP services respectively for Kenya & Mali [9].
The study revealed that short term FP methods such as Condom, Pills and DMPA had the highest indirect costs in GO, NGO and private health facilities accounting 4% to 10% of the total cost of producing a unit of CYP. The reason for this is the frequency with which a client can or will have to visit the health facilities so as to generate one unit of CYP using those short term FP methods. The FP service with the lowest percentage of indirect cost was Implanon, Jadell and IUCD which generates more than one unit of CYP from a single service as a result their proportion of indirect cost was lower than those of short term FP methods.
Conclusion
The study reveals that, Unit cost of providing FP service is significantly higher in NGO owned health facilities followed by, private health facilities. GO health facilities encore a significantly cheaper cost to provide one unit of FP service as well as to generate CYP using both short term and long term FP methods. The cost of producing one unit of CYP from all types of FP Methods is significantly higher in NGO owned health facilities followed by private health facilities.
Long-term FP services such as IUCD and Jadell are the most efficient contraceptive methods as their cost per CYP is found to be lower in all health facilities, while short-term family planning methods like condoms, DMPA, and Pills are less efficient and expensive in the long-term. IUCD is the most efficient contraceptive method as its cos per CYP is the lowest of all followed by Jadell in all health facilities.
The major cost component of the total cost of FP services is the direct cost, which comprises FP commodities, medical Supplies, Personnel cost, cost of infrastructure and laboratory services. There is also slight cost difference among government, NGO and private health facilities mainly because of personnel cost and cost of physical infrastructure.
Declaration
Ethical clearance was obtained from Wollo University College of medicine and health sciences and Ethical Review Committee. Official letter was sent to Dessie city administration zonal health department and the data collection was started after permission was received from the office collect data from all health facilities on which the study was carried out.
Respondents were first asked for their willingness and voluntariness to participate in the study. Then, purpose of the study, procedure and duration, possible risks and benefits of the study were clearly explained for the participants using local language. The respondents were assured of confidentiality by excluding their name during the period of data collection. They were again informed well that they have full right to totally refuse to participate and/or with draw from the study at any time if they have any difficulty.
Acknowledgments
I would like to express my gratitude to Wollo University College of medicine and Health Science, department of Public Health for giving me a chance to study and conduct this thesis. I also like to express my gratefulness to my primary advisor Mr. Negalign Berhanu (PhD fellow) and Mr. Tesfaye Birhane (MPH) for their valuable comments from drafting the proposal to the completion of the study. My especial thank goes to the staffs of Dessie City Administration Zonal Health office, health facilities and their staff who cooperated with me in the process of data collection without whom this study wouldn’t be a reality. I am also grateful to the data collectors and Supervisor, who helped me a lot during the data collection process.
References
- Internation Planned Parenthood Federation. Family guidance association of Ethiopia. FGAE in Perspectives, Addis Ababa, 2016.
- National guideline for family planning service in Ethiopia. Federal Democratic Republic of Ethiopia Ministry of Health, 2011.
- USAID. The health policy project. Family Planning in Ethiopia, 2012.
- USAID. Health policy initiative, task order 1. Achieving the MDGs: The contribution of family planning, Ethiopia, 2009.
- International Planned Parenthood Federation. Sustainable development goals and family planning 2020. 4 Newhams Row, London SE1 3UZ, United Kingdom, 2016.
- Starbird EH. Family planning in the sustainable development goals, 2017.
- UN Population Division. World population prospects, 2009.
- Godbole R, Smith E. Crosswalk of family planning tools: A guide to costing, planning, and impact analysis tools. Washington, DC Futures Group, Health Policy Project, 2014.
- USAID Health Policy Initiative. The cost of family planning in Kenya. One Thomas Circle, NW, 2010.