- Biomedical Research (2005) Volume 16, Issue 2
Correlative study of bone related Biochemical parameters in normal postmenopausal women and hyperglycemic postmenopausal women
Meena Varma, Sangeeta Paneri*, Preetha BadiDepartment of Biochemistry, M.G.M. Medical College, Indore, India
- *Corresponding Author:
- Dr. Sangita Paneri
Department of Biochemistry,
MGM Medical College
Indore 452 001, India
E-mail: drsanlit ( at ) yahoo.com
Accepted date: July 01, 2005
Abstract
Described and treated since ancient times, diabetes is an incurable chronic disease that affects almost every organ and system of the body. The present study comprised a total of 78 postmenopausal women out of which 40 women had diabetes mellitus type 2 and all these women had attained menopause for average five years. The remaining 38 were normal, non-diabetic, and post-menopausal women. Data regarding bone related parameters like calcium, phosphorus, hydroxyproline, bone formation marker alkaline phosphatase, HbA1c and blood sugar levels were estimated. The results obtained showed that in postmenopausal diabetic women the serum alkaline phosphatase tends to be higher, while serum calcium and phosphorus levels are decreased, moreover an increase in level of urinary calcium and hydroxyproline is seen. Therefore, our findings suggest that hyperglycemia in postmenopausal women affect the bone related biochemical parameters.
Keywords
Hyperglycemia, postmenopausal women, bone-related biochemical parameters, alkaline phosphatase.
Introduction
Women have an early postmenopausal phase of rapid bone loss that lasts for 5-10 years after menopause. In women the rapid phase is mediated mainly by loss of the direct restraining effect of estrogen on bone cell function, whereas the slow phase is mediated mainly by the loss of estrogen action on extra skele-tal calcium homeostasis leading to net calcium wasting. Osteopenia has been ascribed to diabetes without residual insulin secretion and high insulin requirement. However, it is not known if this is partially due to disturbance in the Insulin – like growth factor system, which is a key regulator of bone cell function [1]. One study reports that women with diabetes had significantly higher bone mineral density levels than women with normal glucose tolerance [2]. Recent crosssectional studies revealed that the presence of hyperglycemia is associated with higher bone mass and lower fracture rates [3,4,5,6]. One of these stud-ies reports that metabolic improvement of poorly controlled hyperglycemia decreases bone turnover [3]. Other studies indicate that poor glycemic control impairs the responses of osteoblasts and osteoclasts in normo-insulinemic type 2 diabetic patients [7]. Still some studies find no evidence that hyperglycemia produces any change in bone metabolism or mass [8]. It seems worthwhile to investigate the pattern of bone loss in postmeno-pausal women with hyperglycemia.
The aim of this study is to evaluate the effect of hyperglycemia on the rate of bone turnover as well as the status of calcium, phosphorus and hydroxyproline metabolism in postmenopausal diabetic women so that they can be used as prognostic markers to delay or prevent the multifaceted complications before they can eventually manifest.
Material and Methods
The study was conducted in the Department of Biochemistry and Clinical Biochemistry of M.G.M. Medical College and OPD of M.Y. Hospital, Indore.
Clinical Material
Subjects: The clinical material for the present study comprised of a total of 78 post menopausal subjects. Two groups were formed, group 1 comprised of 40 mildly diabetic patients while group 2 comprised of 38 normal, non-diabetic women as a con-trol group. Data regarding history of diabetes, HbA1c values, random blood glucose (RBG) levels, bone-related parameters like calcium phosphorus, alkaline phosphatase (ALP) and hydroxyproline was obtained by structured questionnaires and by clinical and laboratory assessments.
1. Hyperglycemic postmenopausal women (Group 1)
This group comprised of 40 postmenopausal mildly diabetic women. Blood glucose was controlled by balanced diet and exercise. None of the patients had a disease or were treated with drugs that would interfere with calcium or phosphate metabolism and/or bone structure. The exclusion criteria also included hypertension and other factors affecting blood sugar level.
2. Normal Subjects (Group 2)
This group comprised of 38 normal, non-diabetic postmenopausal women, without any prior family history of diabetes and not on any other drug therapy. These individuals were screened for the presence of diabetes based on the diagnostic criteria of the ADA [9].
Collection of material
Blood and urine: From all the above Groups 5ml whole blood was collected along with 24 h urine sample. 0.5ml whole blood was mixed with EDTA reagent (anticoagulant) and kept for the estimation of HbA1c. The remaining whole blood is kept at room temperature for 1 hour after which the supernatant clear fluid is pipetted out into another tube and the sample is used for esti-mation of blood sugar, calcium, phosphorus and ALP. Urine sample is used for estimation of calcium and hydroxyproline.
Clinical Method: estimation of HbA1c, Blood sugar and bone related biochemical parameters
HbA1c, Calcium, Phosphorus, Alkaline phosphatase and Random blood sugar are estimated on fully automated auto-analyzer (Selectra E). Urine hydroxyproline estimation is done by Modified Neuman and Logan method.
Statistical analysis
The statistical analysis was done by student ‘t’ test. The values were expressed as Mean + S.D. (Standard Deviation).
Results
The biochemical findings of the study can be expressed in the form of the following results.
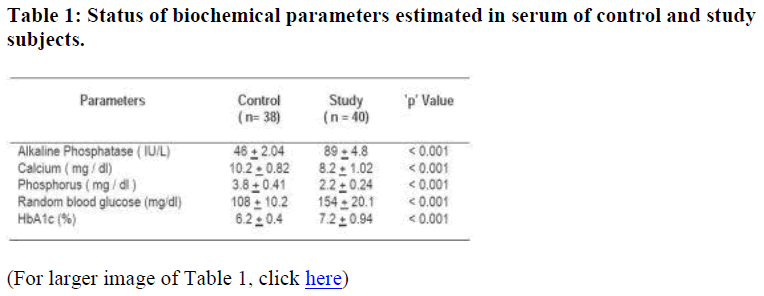
1. Significant increase (p < 0.001) in the alkaline phos phatase level is seen in the study group (Table 1).
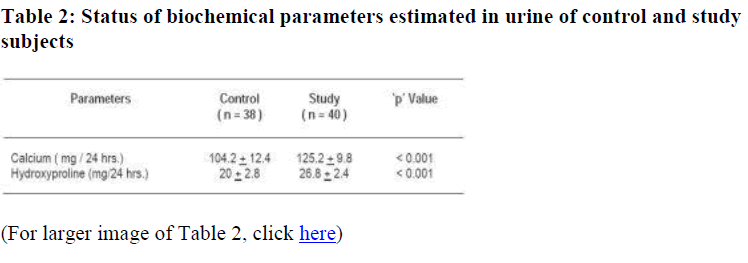
2. Significant decrease (p < 0.001) in the serum calcium and phosphorus level is found in the study group (Table 1) with an associated increase (p < 0.001) of urinary calcium and hydroxyproline levels (Table 2).
3. Blood sugar levels and HbA1c values were signifycantly high (p < 0.001) in the study group subjects (Table 1).
Discussion
During the course of their lifetime, women lose approximately 50% of their trabecular bone and 30% of all postmenopausal women eventually will have osteoporotic fractures. In the pre-sent study the postmenopausal women had an increased serum alkaline phosphatase (Table 1) level. This result is similar to the reports of many earlier studies which demonstrated that bone-specific alkaline phosphatase tends to be higher in diabetic subjects [10,11,12]. A decline in alkaline phosphatase expression with maturation of osteoblasts at mineralization phase [13] sug-gested that hyperglycemia causes a suppression of osteoblast maturation [11]. However, histomorphometric analyses of bones from diabetes type 2 patients do not show such changes [14,15]. In normal postmenopausal women, an increase in bone turnover accelerates the reduction in bone mass, whereas a decrease in bone turnover is associated with preservation of bone mass [16,17,18]..
Although osteoporosis is reported as a potential complication of type 1 diabetes mellitus, the effects of type 2 diabetes mellitus on bone mass are conflicting in postmenopausal women. One study suggested that the bone turnover rate is remarkably lower in diabetes mellitus type 2 patients compared to healthy post-menopausal subjects [19]. In the present study the serum calcium and phosphorus levels were decreased in the study group (Table 1). Poorly controlled NIDDM patients have relative hypercalciuria probably caused by osmotic diuresis associated with glycosuria [20,21]. This could lead to negative calcium balance which might result in accelerated bone resorption and loss of bone [22]. The decrease in urinary calcium excretion after metabolic control correlated with the decrease in urinary glucose excretion as previously reported [20,21,23,24]. Another study found that there is a significant relation between the state of metabolic normalization of diabetes and the degree of biochemical aberrations concerning calcium phosphate metabolism [25]. The increased level of urinary hydroxyproline in diabetic postmenopausal women (Table 1) show increased bone loss [26].
Postmenopausal diabetic women have higher blood sugar values as compared to the control group (Table 1) because the estrogen hormone which makes the body cells more receptive or sensitive to insulin is either not secreted at all or is in limited supply. The estrogen hormone in females is protective for developing diabetes [27]. Estrogen seems to contribute to glucose homeostasis in women [28]. Bone turnover is regulated by many
local cytokines, cell-cell and cell-matrix interactions as well as systemic hormones and hyperglycemia may affect any of these local micro-environments that regulate bone turnover [22].
It is therefore concluded that the biochemical indices of bone turnover estimation show significantly increased bone activity in hyperglycemic postmenopausal women as compared to normal postmenopausal women.
References
- Jehle pm, Jehle DR, Mohan S, Bohm BO. Serum levels of insulin-like growth factor system components and relationship to bone metabolism in Type 1 and Type 2 diabetes mellitus patients. J Endocrinol 1998; 159: 297-306.
- Miedany YM, Gaafary S, Baddini MA. Osteoporosis in older adults with non-insulin dependent diabetes mellitus: is it sex related? Clin Exp Rheumatol 1999; 17: 561-567.
- Barrell?Connor E, Holbrook TL. Sex differences in osteoporosis in older adults with non-insulin dependent diabetes mellitus. JAMA 1992; 268: 3333-3337.
- Bauer DC, Browner WS, Cauley JA et al. Factors associated with appendicular bone mass in older women. The study of Osteoporotic Fractures Research Group. Ann Intern Med 1993; 118: 657-665.
- Van-Daele PL, Stolk RP, Burger H et al. Bone-density in non-insulin dependent diabetes mellitus. The Rotterdam Study. Ann Intern Med 1995; 122: 409-414.
- Rishaug U, Birkeland KI, Falch JA, Vaaler S. Bone mass in non-insulin dependent diabetes mellitus. Scand J Clin Lab Invest 1995; 55: 257-262.
- Inaba M, Nishizawa Y, Mita K, Kumed Y, Emoto M et al. Poor glycemic control impairs the response of biochemical parameters of bone formation and resorption to exogenous 1, 25-dihydroxy vitamin D3 in patients with type 2 diabetes. Osteoporos Int 1999; 9: 525-531.
- Sosa M, Dominguez M, Navarro MC, Segarra MC et al. Bone mineral metabolism is normal in non-insulin dependent diabetes mellitus. J Diabetes Complications 1996; 10: 201-205.
- The expert committee on the diagnosis and classification of diabetes mellitus: Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 1997; 10: 1183-1197.
- Stepan J, Havranek T, Formankova J, Skrha J, Skrha F, Pacovsky V. Bone isoenzyme of serum alkaline phosphatase in diabetes mellitus. Clin Chim Acta 1980; 105: 75-81.
- Bouillon R, Bex M, Van Herck E et al. Influence of age, sex and insulin on osteoblast function: osteoblast dysfunction in diabetes mellitus. J Clin Endocrinol Metab 1995; 80: 1194-1202.
- Gallacher SJ, Fenner JA, Fisher BM et al. An evaluation of bone density and turnover in pre-menopausal women with type 1 diabetes mellitus. Diabet Med 1993; 10: 129-133.
- Stein GS, Lian JB. Molecular mechanisms mediating proliferating / differentiation interrelationships during progressive development of the osteoblast phenotype. Endocr Rev 1993; 14: 424-442.
- Krakauer JC, Mckenna MJ, Buderer NF, Rao DS, Whitehouse FW, Parfitt AM. Bone loss and bone turnover in diabetes. Diabetes 1995; 44: 775-782.
- De-Leeuw I, Mulkens N, Vertommen J, Abs R. A histomorphometric study on the trabecular bone of diabetic subjects. Diabetologia 1976; 12: 385-386.
- Christiansen C, Riis BJ, Rodbro P. Screening procedure for women at risk of developing postmenopausal osteoporosis. Osteoporos Int 1990; 1: 35-40.
- Uebelhart D, Gineyts E, Chapuy MC, Delmas PD. Urinary excretion of pyridinium crosslinks: A new marker of bone resorption in metabolic bone disease. Bone Miner 1990; 8: 87-96.
- Nordin BE, Cleghorn DB, Chatterton BE, Morris HA, Need AG. A 5- year longitudinal study of forearm bone mass in 307 postmenopausal women. J Bone Miner Res 1993; 8: 1427-1432.
- Akin O, Gol K, Akturk M, Erkaya S. Evaluation of bone turnover in postmenopausal patients with type 2 diabetes mellitus using bio-chemical markers and bone mineral density measurements. Gynecol Endocrinol 2003; 17: 19-29.
- Thalassinos NC, Hadjiyanni P, Tzanela M, Alevizaki C, Philokiprou D. Calcium metabolism in diabetes mellitus: effect of improved blood glucose control. Diabet Med 1993; 10: 341-344.
- Nagasaka S, Marakami T, Uchikawa T, Ishikawa SE, Saito T. Effect of glycemic control on calcium and phosphorus handling and parathyroid hormone level in patients with non-insulin dependent diabetes mellitus. Endocr J 1995; 42: 377-383.
- Ryo Okazaki, Yasuo Totsuka, Kumiko Hamano et al. Metabolic improvement of poorly controlled non-insulin dependent diabetes mellitus decreases bone turnover. J Clin Endocrinol Metab 1997: 82; 2915-2920.
- Raskin P, Stevenson MRM, Barilla DE, Pak CYC. The hypercalciuria of diabetes mellitus: its amelioration with insulin. Clin Endocrinol 1978; 9: 329-335.
- Gertner JM, Tanborlane WV, Horst RL, Serwin RS, Felig P, Genel M. Mineral metabolism in diabetes mellitus: changes accompanying treatment with porTable subcutaneous insulin infusion system. J Clin Endocrinol Metab 1980; 50: 862-866.
- Blasiak M, Kuska J, Kokot F, Irzyniec T. Selected indicators of calcium- phosphate metabolism in patients with diabetes mellitus. Endokrynol Pol 1989; 40: 251-62.
- Sachdeva A, Seth S. Study of some common Biochemical bone turnover marker in postmenopausal women. Ind J Clinical Biochem 2005; 20: 135-138.
- Evan JL, Goldfine ID. Glucose status in postmenopausal women. Endocr Rev 2002; 23: 599-622.
- Mayumi Okada, Seiji Namura, Yoko Ikoma, Eiko Yamamnto et al. Effects of postmenopausal hormone replacement therapy on HbA1c levels. Diabetes Care 2003; 26: 1088-1092.