Research Article - Biomedical Research (2017) Volume 28, Issue 7
Correlation between blood lactate and regional cerebral oxygen saturation in complex cardiac pathology neonates and infants: the effect on extubation time and ICU stay
Pelin Karaaslan1*, Aytekin Unlukaplan2, Banu Vural Gokay3, Kamil Darcin2, Burcu Hizarci11, Tijen Alkan Bozkaya4, Arda Ozyuksel5 and Atif Akcevin51Department of Anesthesiology and Reanimation, Medipol University Hospital, Istanbul, Turkey
2Department of Anesthesiology and Reanimation, Koç University Hospital, Istanbul, Turkey
3Department of Anesthesiology and Reanimation, Acıbadem University Hospital, Istanbul, Turkey
4Department of Cardiovascular Surgery, Koç University Hospital, Istanbul, Turkey
4Department of Cardiovascular Surgery, Medipol University Hospital, Istanbul, Turkey
- *Corresponding Author:
- Pelin Karaaslan
Department of Anesthesiology and Reanimation
Medipol University Hospital
Turkey
Accepted date: December 06, 2016
Abstract
Background: The monitoring of regional cerebral O2 saturation (rSO2) with near-infrared spectroscopy (NIRS) is a noninvasive technique to measure tissue oxygenation in the brain. It may be an effective monitoring technique in the early diagnosis of pre-, intra- and post-operative insufficient oxygen supply to the brain in surgery for congenital heart diseases. In pediatric patients, a variety of clinical and laboratory parameters, including serum lactate and regional cerebral oxygen saturation, may be helpful in monitoring global tissue and cerebral oxygen delivery and consumption.
Aim: Our study was designed to investigate whether there is a correlation between the NIRS scores and serum lactate levels during congenital heart surgery. Our secondary objective was to define the predictive value of this correlation on the duration of extubation and intensive care unit stay.
Method: A total of 82 successive neonatal and infant patients with complex cardiac pathologies were enrolled in the study. Blood lactate levels and NIRS values were measured during the phases of anesthesia induction, sternotomy, cannulation, onset of CPB, the beginning of aortic cross-clamping and the end of the CPB.
Study Design: Prospective randomized Results: Patients with normal rSO2 /normal lactate during the operation represented the largest percentage of patients during anesthesia induction (n=50, 60.9%) and sternotomy (n=54, 65.8%). The only negative correlation between lactate and rSO2 was detected during anesthesia induction. The time to extubation and the stay in the intensive care unit were longer in patients with low rSO2 values during anesthesia induction and sternotomy. In the same periods, elevated lactate levels were associated with longer time to extubation and intensive care unit stay than the patients with normal lactate levels.
Conclusion: In our study, no correlation was demonstrated between NIRS scores and serum lactate levels in children during congenital heart surgery, except for anesthesia induction. The only negative correlation between the decrease in NIRS scores and the increase in serum lactate levels was observed during anesthesia induction. This result indicated that cerebral NIRS monitoring cannot be used as an indicator of global hypoperfusion in the same way as lactate.
Keywords
Lactate, Near infrared spectroscopy, Congenital heart diseases
Introduction
Due to advances in myocardial protection, surgical techniques, cardiac anesthesia and postoperative care in recent decades, many congenital heart diseases have been surgically treated with acceptable mortality rates [1]. Although mortality rates have decreased to 3 percent, morbidity is still relatively high in infants undergoing complex cardiac surgical procedures [2,3].
Complex cardiac pathologies are the multiple ones occurring together. Morbidity is thought to be related to inadequate tissue oxygen delivery due to impaired cardiac output, which is a relatively common problem after pediatric cardiac surgery [4]. Intraoperative deterioration in regional cerebral oxygen saturation (rSO2) has also been identified as a potential contributor to neurologic outcomes among children undergoing cardiac surgery [5]. Therefore, the early identification and correction of impaired global tissue perfusion or cerebral blood flow may be expected to decrease the morbidity and mortality of these critical patients. In pediatric patients, a variety of clinical and laboratory parameters, including serum lactate and regional cerebral oxygen saturation, may be helpful in monitoring global tissue and cerebral oxygen delivery and consumption. The level of serum lactate is one of the best indicators of cardiac output, oxygen supply and cellular perfusion [6]. Elevated serum lactate levels during congenital cardiac surgery are associated with poorer outcomes. They mainly appear to be related to an imbalance between oxygen delivery and needs during cardiopulmonary bypass (CPB) or after cardiac surgery [1,7,8]. However, the utility of lactate measurement may be limited because of the need for intermittent blood sampling.
The monitoring of regional cerebral O2 saturation (rSO2) with near-infrared spectroscopy (NIRS) is a noninvasive technique to measure tissue oxygenation in the brain [9]. It may be an effective monitoring technique in the early diagnosis of pre-, intra- and post-operative insufficient oxygen supply to the brain in surgery for congenital heart diseases [10]. In addition, the use of NIRS has expanded to examine oxygenation in other tissues and to estimate the adequacy of systemic circulation [11]. If a correlation between NIRS measurements and lactate levels can be demonstrated, then it will ensure more reliable monitoring for cardiac output, earlier diagnosis of global tissue perfusion and earlier intervention. This study was designed to investigate whether there is a correlation between the NIRS scores and serum lactate levels during congenital heart surgery. Our secondary objective was to define the predictive value of this correlation on the duration of extubation and intensive care unit stay.
Patients and Methodology
Patients and study design
This was a prospective study of the infants with congenital heart diseases who underwent corrective surgery between September 2012 and May 2013 at a university hospital. The study was approved by the institutional ethics committee of the university. A total of 82 successive neonatal and infant patients with complex cardiac pathologies were enrolled in the study. Emergency cases, off-pump surgeries, hemodynamically unstable patients during the preoperative period, and infants weighing less than 2 kg were excluded from the study.
Monitoring of the patients
Noninvasive monitoring included electrocardiography, pulse oximetry, and analysis of inspiratory and expiratory gas concentrations. The body temperature of the patients was continuously measured from the nasopharynx. The right femoral artery and right internal jugular vein were catheterized for the measurement of arterial pressure and central venous pressure, respectively. Near infrared spectroscopy monitoring was performed continuously using a NIRS sensor (INVOSTM-5100 C, Medtronic Inc., Minneapolis, MI, USA) attached on the forehead of the patients. The first NIRS score after induction of anesthesia was considered the baseline rSO2.
Anesthetic management
All patients over 6 months of age were pre-medicated using oral midazolam (0.5 mg/kg) preoperatively. Anesthesia was induced with inhalation of sevoflurane (6 %) in a 70% O2 + 30% air mixture. After accessing the intravenous line, fentanyl (3 mcg/kg) and rocuronium (0.6 mg/kg) were administered intravenously, and the patients were intubated. Anesthesia was maintained with 2% sevoflurane in the oxygen-air mixture and intermittant fentanyl and rocuronium boluses were administered.
Intraoperative management of patients
All operations were performed by the same team of two cardiac surgeons during the study period. Cardiac procedures were performed in all patients using median sternotomy. Following systemic heparinization (4 mg/kg), the aorta and superior and inferior vena cava were cannulated and cardiopulmonary bypass (CPB) was initiated. Pulsatile perfusion was achieved using a pulsatile roller pump (Maquet HL20, Hirrlingen, Germany). During CPB, hematocrit, mean arterial pressure and arterial oxygen saturation were maintained at 28-35%, 40 mmHg and 70-90%, respectively. Myocardial protection was achieved with blood cardioplegia applied at 20-minute intervals. Hypothermic circulatory arrest was not performed in any patient. At the end of the surgical correction, dopamine and milrinone were initiated routinely at low-moderate doses to maintain a mean pressure at 40 mmHg, and CPB was terminated. In cases of need, doses were adjusted. In required patients, modified ultrafiltration was applied. In cases of regional cerebral oxygenation deterioration, the algorithm in the use of brain oximetry proposed by Denault et al. was used to treat the decrease in rSO2.
Measurements
Blood lactate levels, obtained from the peripheral arterial line, were measured during the phases of anesthesia induction, sternotomy, cannulation, onset of CPB, the beginning of aortic cross-clamping and the end of the CPB. A lactate level over 3 mmol/L was considered to represent hyperlactatemia. Heart rate, mean arterial pressure, temperature, pH, PaCO2, PaO2, SaO2, and hematocrit level were recorded in the same time periods. The duration of cardiopulmonary bypass, the amounts of blood products used, duration of the surgery, the time to extubation and intensive care unit (ICU) stays were also recorded.
Statistical analysis
Power analysis was performed in G Power 3.1.9.2, and based on previous studies 95% actual power, total sample size was found to be 72 patients. Categorical values and continuous numerical data were analyzed using the chi-square and Mann- Whitney U tests, respectively. Pearson’s correlation coefficient was employed to compare lactate and NIRS levels. p<0.05 was accepted as the level of significance. All values were presented as mean ± standard deviation.
Results
The patients’ demographics and operative variables are summarized in Table 1 and Table 2.
| Variable | Value |
|---|---|
| Age (months) | 6.01 ± 3.7 |
| Weight (kg) | 6.0 ± 2.1 |
| Preoperative arterial oxygen saturation (%) | 87.5 ± 11.2 |
| Preoperative hematocrit (%) | 37.25 ± 2.1 |
| Aortic cross-clamp time (min) | 67.75 ± 10.4 |
| CPB time (min) | 101.8 ± 21.1 |
Table 1: Preoperative and operative variables (Mean±S.D.)
| Lesion Classification | Diagnosis | No. |
|---|---|---|
| Two Ventricle | Tetralogy of Fallot | 12 |
| Ventricular septal defect | 12 | |
| Atrial septal defect | 10 | |
| Transposition of the great arteries | 8 | |
| Atrioventricular septal defect | 8 | |
| Totally anomalous pulmonary venous drainage | 4 | |
| Aortic insufficiency | 4 | |
| Aortic stenosis | 4 | |
| Corrected transposition | 2 | |
| Pulmonic stenosis | 2 | |
| RVOT obstruction | 2 | |
| Truncus arteriosus | 2 | |
| Aortic coarctation | 1 | |
| Single Ventricle | Hypoplastic left heart syndrome | 5 |
| Tricuspid atresia/pulmonary atresia | 4 | |
| Double outlet ventricle | 2 |
Table 2: Summary of congenital heart disease diagnosis by anatomical group
Most of the patients included in study had tetralogy of Fallot (n=12), ventricular septal defect (n=12), followed by atrial septal defect (n=10), atrioventricular septal defect (n=10) and transposition of great arteries (n=8). Three patients died following Benthall operation, Norwood Stage 1, and arterial switch operation.
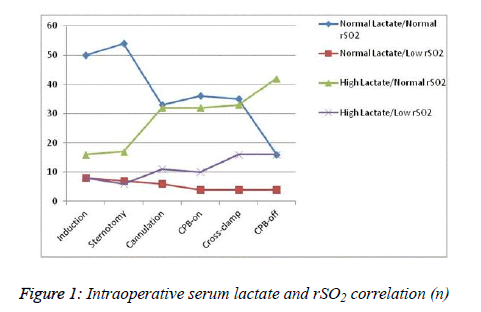
Patients with normal rSO2/normal lactate during the operation represented the largest percentage of patients during anesthesia induction (n=50, 60.9%) and sternotomy (n=54, 65.8%) (Figure 1). During CPB, the percentage of patients with abnormal rSO2 or lactate was higher than that of patients with normal rSO2/ normal lactate in all measurement phases. The only negative correlation between lactate and rSO2 was detected during anesthesia induction.
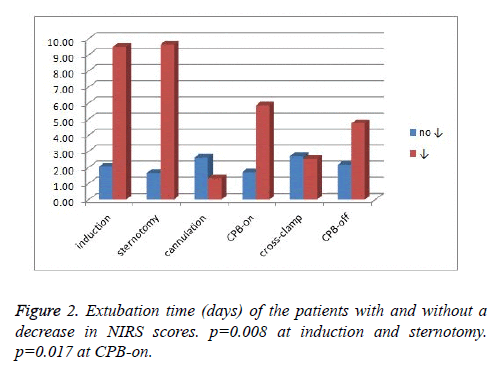
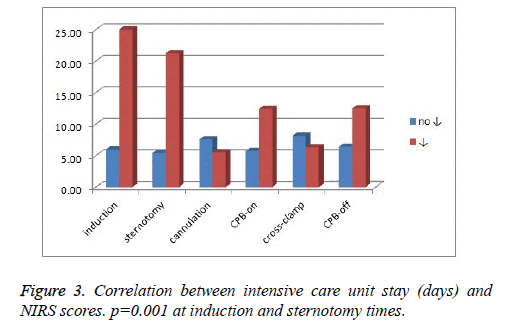
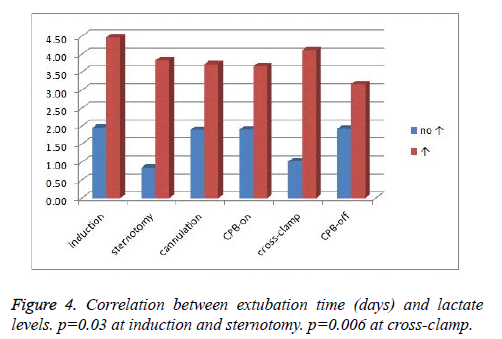
Postoperative variables
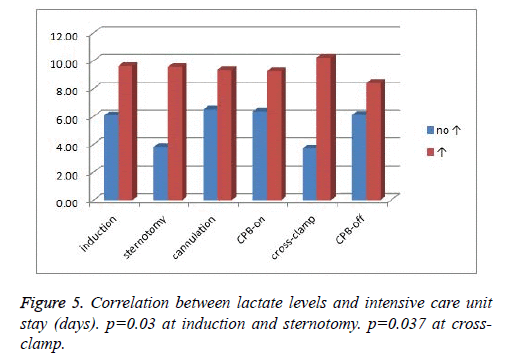
The time to extubation and the stay in the intensive care unit were longer in patients with low rSO2 values during anesthesia induction and sternotomy (p=0.008, p=0.001, respectively) than the patients with normal NIRS values during the same time periods. In the same periods, elevated lactate levels were associated with longer time to extubation and intensive care unit stay than the patients with normal lactate levels (p=0.03). The decrease in rSO2 at the onset of CPB and the increase in serum lactate during cross clamping were associated with time to extubation and intensive care unit stay (p=0.017, p=0.037, respectively) (Figures 2-5). Upon the termination of CPB, a significant increase in blood lactate levels of 34 patients was recorded, which was not significantly correlated with extubation time and intensive care unit stay (Figures 3 and 4).
During anesthesia induction, a negative correlation was detected in between the decrease in NIRS scores and the increase in lactate levels (p=0.01). In all other measurements, this negative correlation did not reach significant levels.
Discussion
In this study, we demonstrated that low NIRS and high lactate levels were associated with an increased risk of prolonged time to extubation and intensive care unit stay in children undergoing congenital heart surgery. However, we failed to demonstrate a correlation between NIRS scores and serum lactate levels during congenital heart surgery except for the negative correlation during anesthesia induction. This result indicated that cerebral NIRS monitoring cannot be used as an indicator of global hypoperfusion in the same way as lactate during congenital heart surgery.
Inadequate tissue oxygen delivery due to impaired cardiac output is a relatively common problem during pediatric cardiac surgery. Global or regional tissue hypoperfusion should be diagnosed early and treated immediately to prevent organ dysfunction and organ failure in these patients [12]. Routinely monitored parameters, such as blood pressure, heart rate, arterial oxygen saturation, and urine output, may not reflect the adequacy of global perfusion in these patients. Therefore, various clinical indicators and biochemical markers reflecting tissue perfusion and systemic oxygen delivery have been commonly investigated to gauge the adequacy of tissue oxygen delivery during this critical time period [12]. Blood lactate has been studied as a potential clinical marker of global hypoperfusion after cardiac surgery, particularly in children [4,13,14]. In these studies, elevated lactate levels were reported to be associated with metabolic acidosis, tissue hypoperfusion and hypoxia during cardiac surgery with cardiopulmonary bypass (CPB).
Elevated lactate levels as a result of impaired cardiac output have been associated with significant morbidity and mortality after pediatric cardiac surgery. [14,15] Therefore, multiple studies of pediatric data have examined the utility of blood lactate levels as both positive and negative predictors of outcome after surgery for CHD [1,8,16-18]. Basaran et al. demonstrated the presence of a correlation between high lactate levels detected in the early postoperative period and mortality in 60 patients who would undergo surgery to treat their congenital heart disease [1]. In addition, they stated that high lactate levels correlated significantly with inotrope score, intubation time, and duration of intensive care unit stay. Similarly, Charpie et al. [8] demonstrated that high lactate levels were a predictor of mortality within 72 h of surgery or the need for extracorporeal membrane oxygenation support in infants undergoing complex cardiac surgeries. Cheifetz et al. [17] demonstrated that lactate levels of the infants aged <1 year who had undergone cardiopulmonary bypass were very useful as markers of mortality. Hatherill et al. [18] also demonstrated that children with a complicated post-operative course had higher median serum lactate levels than patients with an uncomplicated course.
Similarly, in our study, increases in serum lactate levels during surgery were found to be correlated with increases in the duration of postoperative extubation and ICU stay. A positive correlation between hyperlactatemia and postoperative negative outcome forces clinicians to prevent, detect and treat the increase of serum lactate levels during pediatric cardiac surgery. Levels of lactate maintained at high levels following a complex surgery should be assigned importance as markers of mortality. If discerned in time, during this worsening disease progression, aggressive measures, which increase both cardiac output and arterial oxygen content, should be taken prematurely. Every effort should be made to increase cardiac output by optimizing heart rate, increasing preload, correcting ventricular contractility and decreasing afterload. Additionally, arterial oxygen content should be enhanced by increasing oxygen saturation of the inspiratory air and normalizing hemoglobin values. Adjusted oxygen supply will improve survival rates. Therefore, every method that can discern disequilibrium between oxygen demand and supply at an early stage is important.
Despite the fact that a correlation between lactate levels coursing at high levels and morbidity in pediatric cardiac surgery was demonstrated, the continuous measurement of lactate levels was not possible due to its invasive nature. Additionally, measurements at intervals may delay the recognition of deranged tissue perfusion. Therefore, considering the study performed by Chakravarti et al. [4], who demonstrated the presence of a serious negative correlation between high lactate levels and low NIRS values, we believed that we could discern the state of hypoperfusion at an early stage using continuous monitoring with NIRS measurements rather than intermittent lactate evaluations. Monitoring regional cerebral oxygen saturation (rSO2) with near-infrared spectroscopy (NIRS) is a noninvasive, continuous, and real-time measurement technique that monitors brain tissue oxygen saturation through the measurement of oxyhemoglobin and de-oxyhemoglobin concentrations. [9,10,19,20] NIRS provides valuable information not only about cerebral oxygenation but also about the oxygenation of systemic tissues [21]. Previous studies have provided some evidence that low rSO2 values reflect impaired global tissue perfusion and the development of organ dysfunction [22]. There is increasing evidence that low rSO2 values are associated with adverse neurological outcomes and death in congenital heart surgery. In a retrospective review of HLHS patients undergoing Norwood Stage I palliation, Phelps et al. [23] determined the relationship between mean rSO2 in the 48 hours postoperatively, with death, need for ECMO, and prolonged ICU stay >30 days. In the study of Dent et al. [24], a prolonged low rSO2 (>180 minutes with< rSO2 45%) was associated with a higher risk of new ischemic lesions on postoperative MRI when compared to the pre-surgical study in neonates undergoing the Norwood operation. Slater et al. [25] demonstrated that prolonged desaturation time observed in NIRS extends the period of hospital stay after cardiac surgery. Chakravarti et al. [4] also stated that low cerebral NIRS readings below 45% at any time point was correlated with postoperative mortality. In the first 24 postoperative hours, a mean arterial lactate level >9.3 mmol/L was correlated with adverse clinical events, primarily ECMO and death. In our study, the duration of extubation and ICU stay were found to be longer in patients with lower NIRS scores than the patients with normal NIRS scores. It should be emphasized that hemoglobin and PaCO2 levels during cardiac surgery have an impact on NIRS measurements. Hemodilution and reduced PaCO2 will decrease NIRS scores by decreasing the cerebral blood flow rate [26]. Despite our efforts to keep these values at similar levels, we believe that all of these subfactors effected the outcome of our study.
The correlation of intraoperative regional oxygen saturation (rSO2) estimated by near-infrared spectroscopy with serum lactate levels in infants with congenital heart disease who had previously undergone cardiac surgery has been investigated [21]. In a prospective study, the averaged cerebral and renal rSO2 was found to be a good predictor of lactate, with a value less than or equal to 65%, predicting a lactate level of greater than or equal to 3.0 mmol/L with a sensitivity of 95% and a specificity of 83% in the patients investigated. Furthermore, the authors claimed that rSO2 may be an early indicator of impaired oxygen delivery to the tissues, and the monitoring of rSO2 could aid in the prompt identification of patients at risk for low cardiac output syndrome [4]. In contrast, Bhalala et al. [27] reported that splanchnic and/or renal hypoxemia as detected by near-infrared spectroscopy may not be an accurate indicator of low cardiac output after surgery for congenital heart defects. Similarly, Dodge-Khatami et al. [20] reported that they found a weak correlation between either cerebral or renal NIRS with lactate levels when the full 24 postoperative hours were considered. However, when each time point was considered separately, they found that cerebral rSO2 readings had a strong inverse correlation with arterial lactate levels up to 6 hours and lesser so thereafter until study completion. During states of low cardiac output, cerebral blood flow and thus cerebral NIRS may be better preserved than in somatic tissue sites. The physiological protection mechanism of cerebral blood flow may explain the lack of the correlation between NIRS scores and blood lactate levels during low cardiac output situations. Ciccone et al. demonstrated in their study that different degrees of maturity influence morpho-functional cardiac alterations during the transitional period [28]. In our study different ages and different pathologies of the children might be another reason for the results. In our study, no correlation was demonstrated between NIRS scores and serum lactate levels in children during congenital heart surgery, except for anesthesia induction. The only negative correlation between the decrease in NIRS scores and the increase in serum lactate levels was observed during anesthesia induction. This result indicated that cerebral NIRS monitoring cannot be used as an indicator of global hypoperfusion in the same way as lactate.
Limitations
The most important limitation of our study was that despite long-term follow-ups of our patients, we did not record long-term outcomes of these patients using neurological tests. Patient sample size could be larger. So in a similarly designed study with a larger sample size, we aimed to evaluate and present the outcomes of long-term neurological innovations. We believe that in the future, using a combination of serial lactate measurements and NIRS monitorization, modifications that will change the direction of the treatment without a loss of time would be made. Thus, it will be possible to correct lower cardiac output with an early intervention [12] in children undergoing congenital heart surgery.
Acknowledgements
The English in this document has been checked by at least two professional editors, both native speakers of English.
References
- Basaran M. Serum lactate level has prognostic significance after pediatric cardiac surgery. J Cardiothorac Vasc Anesth 2006; 20: 43-47.
- Redlin M. Regional differences in tissue oxygenation during cardiopulmonary bypass for correction of congenital heart disease in neonates and small infants: relevance of near-infrared spectroscopy. J Thorac Cardiovasc Surg 2008; 136: 962-967.
- Welke KF, Shen I, Ungerleider RM. Current assessment of mortality rates in congenital cardiac surgery. Ann Thorac Surg 2006; 82: 164-170.
- Chakravarti SB. Multisite near-infrared spectroscopy predicts elevated blood lactate level in children after cardiac surgery. J Cardiothorac Vasc Anesth 2009; 23: 663-667.
- Daubeney PE. Cerebral oxygenation during paediatric cardiac surgery: identification of vulnerable periods using near infrared spectroscopy. Eur J Cardiothorac Surg 1998; 13: 370-377.
- Allen M. Lactate and acid base as a hemodynamic monitor and markers of cellular perfusion. Pediatr Crit Care Med 2011; 12: S43-49.
- Hajjar LA. High lactate levels are predictors of major complications after cardiac surgery. J Thorac Cardiovasc Surg 2013; 146: 455-460.
- Charpie JR, Dekeon MK, Goldberg CS, Mosca RS, Bove EL. Serial blood lactate measurements predict early outcome after neonatal repair or palliation for complex congenital heart disease. J Thorac Cardiovasc Surg 2000; 120: 73-80.
- Owen-Reece H, Smith M, Elwell CE, Goldstone JC. Near infrared spectroscopy. Br J Anaesth 1999; 82: 418-426.
- Durandy Y, Rubatti M, Couturier R. Near Infrared Spectroscopy during pediatric cardiac surgery: errors and pitfalls. Perfusion 2011; 26: 441-446.
- Moerman A, Wouters P. Near-infrared spectroscopy (NIRS) monitoring in contemporary anesthesia and critical care. Acta Anaesthesiol Belg 2010; 61: 185-194.
- Hu BY. Combined central venous oxygen saturation and lactate as markers of occult hypoperfusion and outcome following cardiac surgery. J Cardiothorac Vasc Anesth 2012; 26: 52-57.
- Agrawal A. Point of care serum lactate levels as a prognostic marker of outcome in complex pediatric cardiac surgery patients: Can we utilize it? Indian J Crit Care Med 2012; 16: 193-197.
- Cheung PY, Chui N, Joffe AR, Rebeyka IM, Robertson CM; Western Canadian Complex Pediatric Therapies Project. Postoperative lactate concentrations predict the outcome of infants aged 6 weeks or less after intracardiac surgery: a cohort follow-up to 18 months. J Thorac Cardiovasc Surg 2005; 130: 837-843.
- Duke T. Early markers of major adverse events in children after cardiac operations. J Thorac Cardiovasc Surg 1997; 114: 1042-1052.
- Schumacher KR. Rate of increase in serum lactate level risk-stratifies infants after surgery for congenital heart disease. J Thorac Cardiovasc Surg 2014; 148: 589-595.
- Cheifetz IM. Serum lactates correlate with mortality after operations for complex congenital heart disease. Ann Thorac Surg 1997; 64: 735-738.
- Hatherill M, Sajjanhar T, Tibby SM, Champion MP, Anderson D. Serum lactate as a predictor of mortality after paediatric cardiac surgery. below Arch Dis Child 1997; 77: 235-238.
- Mauriat P, Tafer N, Ouattara A. Monitoring of oxygen saturation by near-infrared spectroscopy and paediatric cardiac surgery: Not just for the brain. Anaesth Crit Care Pain Med 2015; 34: 257-258.
- Dodge-Khatami J, Gottschalk U, Eulenburg C, Wendt U, Schnegg C. Prognostic value of perioperative near-infrared spectroscopy during neonatal and infant congenital heart surgery for adverse in-hospital clinical events. World J Pediatr Congenit Heart Surg 2012; 3: 221-228.
- Zulueta JL. Role of intraoperative regional oxygen saturation using near infrared spectroscopy in the prediction of low output syndrome after pediatric heart surgery. J Card Surg 2013; 28: 446-452.
- Nagdyman N. Comparison between cerebral tissue oxygenation index measured by near-infrared spectroscopy and venous jugular bulb saturation in children. Intensive Care Med 2005; 31: 846-850.
- Phelps HM, Mahle WT, Kim D, Simsic JM, Kirshbom PM. Postoperative cerebral oxygenation in hypoplastic left heart syndrome after the Norwood procedure. Ann Thorac Surg 2009; 87: 1490-1494.
- Dent CL. Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 2006; 131: 190-197.
- Slater JP. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg 2009; 87: 36-44.
- Pollard V. The influence of carbon dioxide and body position on near-infrared spectroscopic assessment of cerebral hemoglobin oxygen saturation. Anesth Analg 1996; 82: 278-287.
- Bhalala US. Change in regional (somatic) near-infrared spectroscopy is not a useful indicator of clinically detectable low cardiac output in children after surgery for congenital heart defects. Pediatr Crit Care Med 2012; 13: 529-534.
- Ciccone MM, Scicchitano P, Zito A, Gesualdo M, Sassara M. Different functional cardiac characteristics observed in term/preterm neonates by echocardiography and tissue doppler imaging. Early Hum Dev 2011; 87: 555-558.