Research Article - Current Pediatric Research (2017) Volume 21, Issue 2
Cord blood albumin as a predictor of neonatal hyperbilirubinemia in healthy neonates
Gaurav Aiyappa KC*Department of Pediatrics, AJ Institute of Medical Sciences and Research Centre, India.
- *Corresponding Author:
- Gaurav Aiyappa KC
AJ Institute of Medical Sciences and Research Centre
Department of Pediatrics, Kuntikana, Mangalore
Karnataka, 575004, India.
Tel: +919481961779
E-mail: gauravaiyappa426@gmail.com
Accepted date: March 07, 2017
Abstract
Objective: To determine the correlation between cord albumin levels and development of hyperbilirubinemia in term healthy neonates. Methods: A Prospective study was conducted on 165 term healthy neonates. Gender, gestational age, anthropometric measurements were taken into consideration. It was ascertained that there was no other risk factor for hyperbilirubinemia amongst the neonates. The neonates were divided into two groups A and B based on the cord albumin levels of <2.8 mg/dl and >2.8 mg/dl. Results: Of the 165 babies included in the study, 126 babies were under Group 1 and 39 under Group 2. 44 babies (34%) in group 1 and 28 babies (71.7%) in group 2 (p<0.0005) developed clinical icterus of which 16 in group 1 and 19 in group 2 required phototherapy (p<0.05). 1 baby in group 2 required exchange transfusion. The sensitivity and specificity of cord albumin in detecting neonatal hyperbilirubinemia in this study was determined to be 71.8% and 65.1%, respectively. Conclusion: Cord albumin levels help to determine and predict the possibility of hyperbilirubinemia among neonates. Hence this can help to identify the at risk neonates. So routine determination of cord albumin can be advocated to keep a track on at risk neonates.
Keywords
Cord albumin, Hyperbilirubinemia, Icterus.
Introduction
Neonatal Jaundice or icterus neonatrum has been observed in new-born babies for many centuries. It was in the early 18th century that Juncker first differentiated between true jaundice and the yellowish tinge observed in many neonates [1].
About 84% of the new-borns are affected by neonatal hyperbilirubinemia and it is considered as the most common cause for readmission to the hospital during this period [2]. Severe hyperbilirubinemia is when the total serum bilirubin [TSB] level is more than 20 mg per dL and it occurs in less than 2% of term infants and can lead to kernicterus. Hence it is important to evaluate all newborns for clinical signs of hyperbilirubinemia.
Risk factors for the hyperbilirubinemia include cephalhematoma or significant bruising, early gestational age, exclusive unsuccessful breastfeeding, isoimmune or other hemolyticanemia and a sibling with a history of neonatal jaundice [3]. In addition to hyperbilirubinemia, earlier gestational age, hemolysis, sepsis, and low birth weight are associated with the development of bilirubin encephalopathy. As per the guidelines set down by the American Academy of Pediatrics neonates discharged within 2 days of birth must report back for a follow-up visit within 48-72 h after discharge [4].
Physiological hyperbilirubinemia is a result of immature liver cell which have low uridine diphosphoglucuronosyl transferase activity when compared to mature hepatocyte, low concentration of albumin which is a bilirubin binding ligand and increased number of erythrocytes which have a shorter life span. Physiological jaundice is a normal response on the part of the baby due limitations in the ability to excrete bilirubin. Neonates develop an unconjugated hyperbilirubinemia due to increased level of unconjugated Bilirubin above 1.0 mg/dl. Early treatment with phototherapy is effective, simple and cheap. This is the appropriate treatment for exaggerated neonatal jaundice [5].
Liver is the site of synthesis of albumin. It binds to unconjugated bilirubin and helps in the transport. This in turn reduces the bilirubin toxicity on the tissues and thereby competing with tissues for bilirubin binding. Extremely avid binding to albumin may be detrimental, however, because it limits the rate of hepatic removal of unconjugated bilirubin from the plasma [6,7].
Low production of albumin will lower its transport and binding capacity and hence determination of at risk neonates early on will help to avoid the complications associated with neonatal jaundice [8]. It has been noted that there is a dramatic decrease in the hospital stays of healthy neonates over the past few decades. It has been noted that the neonates that appear healthy are usually discharged within 48 hours of birth [9]. Hence it is important to determine the babies who are at risk of developing hyperbilirubinemia following an early discharge from the hospital. Hence the present study was conducted in order to determine the correlation between cord albumin and development of neonatal hyperbilirubinemia.
Materials and Methods
This was a hospital based, prospective study and was conducted in the department of paediatrics, A J Institute of Medical Sciences, Mangalore. The study group consisted of 165 simultaneously born full term healthy neonates delivered at A J Institute of Medical Sciences between November 2015 and June 2016. Ethical clearance was obtained from the institutional research board of A J Institute of Medical Sciences.
All the healthy term new-borns during the study period were included in the study after obtaining consent from the parents. Neonates with ABO or Rh incompatibility, Major congenital malformations, Cephalhematoma, Early onset sepsis and Preterm babies were excluded from the study. The data was entered into the Performa in which the gender, gestational age, mode of delivery, anthropometric measurements at birth, cord TSH, Cord albumin and total and direct bilirubin of the babies were noted.
3 ml of cord blood was collected at birth in a SST and was sent for estimation of cord blood albumin and TSH. Cord Albumin was assessed using the Biuret reaction technique using an automated analyzer. Babies were examined daily for the presence of icterus up to the 5th day following which they were discharged. On detecting the presence of icterus, Blood was sent for estimation of Total Bilirubin (TB) and the results were plotted on the chart to identify the type of intervention the baby required. Data was collected as per the Performa after obtaining consent from the parents of the neonates.
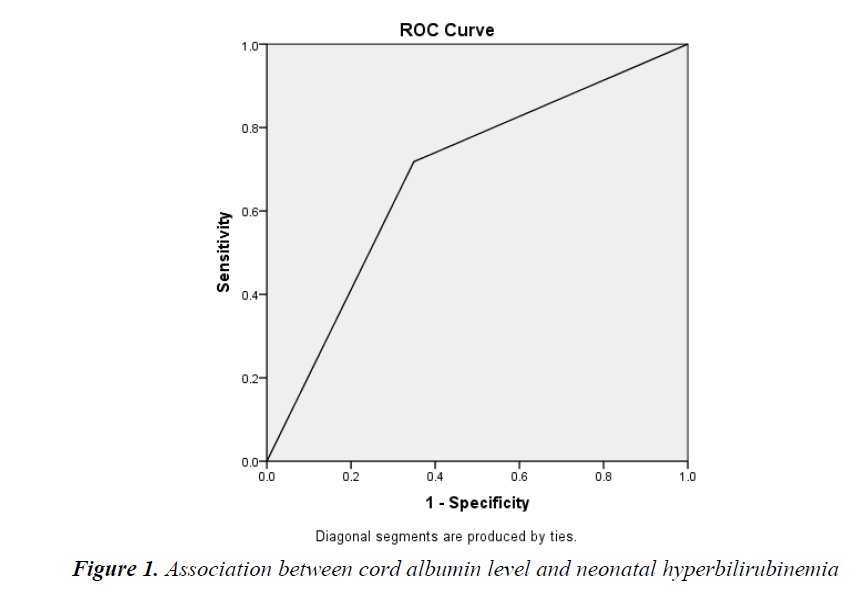
The main outcome of the study was inferred in terms of neonatal hyperbilirubinemia. All the data was entered in Microsoft excel sheet and SPSS Version 21.Statistical data were analysed with t test, chi-square test and ANOVA. Sensitivity, specificity, negative and positive predicative value of the tests was calculated. The cord albumin levels having highest specificity and sensitivity was determined with the Receiver Operating Characteristics (ROC) curve analysis.
Results
In the study a total of 165 babies were registered. Out of this 52.7% were female and 47.3% were male. There was no significant difference in the number of male and female babies. Depending on the cord albumin levels the babies were grouped into two: >2.8 mg/dl (Group 1) and <2.8 mg/dl (Group 2). Lower normal limit for cord serum albumin in term babies is 2.8gm/dl [10]. There were a total of 126 babies in Group 1 and 39 babies in Group 2. The mean gestational age was among Group 1 was 39.022 ± 1.144 weeks and Group 2 was 38.194 ± 2.039. It was noted that babies born at a lower gestational age had a higher chance of having a low albumin value and subsequent hyperbilirubinemia (p=0.002). 84 babies were born by normal vaginal delivery and 81 were born by LSCS and there was no significant difference between the babies developing icterus based on the mode of delivery. The anthropometric profile of both the groups were compared and it was noted that only the birth weight had a significant correlation with cord albumin (p<0.001) (Table 1). A significant correlation was noted between the Cord TSH and cord Albumin levels in this study (Table 2).
Discussion
Out of 165 babies, 72 babies developed icterus. Under group 1, 44 babies developed icterus and under group 2, 28 babies developed icterus. The total bilirubin levels were significant in Group 2 (p<0.001) (Table 3). 35 babies of the 72 with icterus required phototherapy and it was noted that majority of these babies were from group 2 (p<0.05) (Table 4). Only 1 baby required exchange transfusion and it belonged to group 2.
In our study, the sensitivity of cord albumin to detect hyperbilirubinemia in new-born was determined and found to be 71.8%, while specificity was 65.1%. The positive predictive value was found to be 38.9% and the negative predictive value was found to be 88.2%. The accuracy rate was 67.3%. The same has been depicted in the ROC shown in Figure 1 (AUC=0.684).
In the present study we assessed the ability if cord albumin in assessing and acting as a tool for screening for neonatal jaundice. Albumin in a neonate is the major binder of bilirubin and decrease the binding and transport of it [11]. The study group has a uniform representation from both the sexes with no significant correlation. However studies done by Satrya et al. [12] and Maisels et al. [13] had showed that male babies are at a higher risk of developing icterus and subsequent intervention for icterus. But the present study is in correlation with study done by Taksande et al. [14] which states that there is no relation between neonatal hyperbilirubinemia and the sex of the baby.
In this study it was noted that the gestational age at which the baby was born had a positive correlation with the presence lower albumin levels. It was noted that lower the gestational age higher was the chance of the baby developing icterus.
| Group 1 | Group 2 | P value | |
|---|---|---|---|
| Gestational age | 39.022 ± 1.144 | 38.194 ± 2.039 | 0.002 |
| Birth weight | 3.042 ± 0.387 | 2.642 ± 0.544 | <0.001 |
| Length | 47.5 ± 3.45 | 47.64 ± 2.30 | 0.239 |
| Head circumference | 34.68 ± 2.026 | 34.59 ± 2.468 | 0.805 |
Table 1. Gestational age and Anthropometric data
| Group 1 | Group 2 | P value | |
|---|---|---|---|
| Cord TSH | 10.384 ± 7.013 | 17.045 ± 6.220 | <0.001 |
Table 2. Relation between cord TSH and cord albumin
| Total number | Total Bilirubin value | P value | |
|---|---|---|---|
| Group 1 | 44 (34%) | 11.78 ± 3.13 | <0.001 |
| Group 2 | 28 (71.7%) | 15.96 ± 3.960 | |
| Direct Bilirubin Value | |||
| Group 1 | 0.638 ± 0.199 | 0.714 | |
| Group 2 | 0.6564 ± 194 |
Table 3. Relation between cord albumin and bilirubin
| Group 1 | Group 2 | P value | |
|---|---|---|---|
| Neonates with Icterus | 44 | 28 | <0.0005 |
| New-borns requiring phototherapy | 16 | 19 | <0.05 |
Table 4. Relation between cord albumin and interventions required
It was noted that there was no relation between the mode of delivery and the development of icterus and the cord albumin levels were not significantly different. This was in correlation with the studies done by Sun et al. [15] and Sahu et al. [16]. When the birth weight of the neonate was considered it was seen that babies born with lower weight had a significantly higher chance of developing of icterus and the babies mostly had low cord albumin levels. Whereas previous studies by Knusden et al. [17], Awasthi et al. [18] had stated that there was no significant correlation between the birth weight and low cord albumin values.
Out of the 165 neonates included in our study, 71.8% and 34.9% babies from group A and B developed icterus. In group a 76.9% required phototherapy and 50% required exchange transfusion while in Group B 14.7% required phototherapy and none underwent exchange transfusion. Trivedi et al. [19] in their study involving 605 neonates had concluded that majority of the infants who required phototherapy had a cord albumin level lower than 2.8 mg/dl. Sahu et al. [20] in a study of 40 neonates found that 80% neonates with cord albumin less than 2.8 mg/dl required phototherapy.
Pahuja et al. [21] in their had noted that predictive value of cord albumin for development of neonatal hyperbilirubinemia was 75% which implies a fair predictive value of the criteria with 61.3% sensitive and 76.8% specific and is in correlation with the present study. A study by Nahar et al. [22] showed cord bilirubin level >2.5 mg/dl had a sensitivity of 77%, specificity of 98.6% with negative predictive value of 96% which is in correlation with the present study. Sahu et al. [20] showed that 70% new-born who developed significant Neonatal hyperbilirubinemia had cord albumin level <2.8 g/dL, 30% new-born had cord albumin level 2.9-3.3 g/dl and none of the new-borns with cord albumin level >3.4 g/ dL developed hyperblirubinemia [16]. In this study it was noted that between cord albumin and development of neonatal hyperbilirubinemia (p value <0.001) there was a significant correlation. Trivedi et al. [23] studied a total of 605 new-borns. Off these, 205 new-borns developed significant neonatal hyperbilirubinemia in study group with 58.35% (120/205) of the neonates with cord albumin level <2.8 g/dl developing significant neonatal hyperbilirubinemia (P ≤ 0.05). Our study results correlated with these studies.
Conclusion
Cord Albumin levels in a healthy term neonate helps to predict the possibility of the neonate having hyperbilirubinemia. It helps to determine the neonates who are at a higher risk of developing jaundice. A value less than 2.8 mg/dl has found to be more associated with clinical icterus. Hence routine determination of cord Albumin along with TSH can be implemented to keep track of at risk neonates.
References
- Bryon JL, Nancy DS. Hyperbilirubinemia in the new-born. Pediatr Rev 2011: 32: 341-349.
- Sgro M, Campbell D, Shah V. Incidence and causes of severe neonatal hyperbilirubinemia in Canada. CMAJ 2006; 175: 587-590.
- Maisels MJ, Bhutani VK, Bogen D, et al. Hyperbilirubinemia in the new-born infant = 35 weeks? gestation: An update with clarifications. Pediatrics 2009; 124: 1193-1198.
- American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the new-born infant 35 or more weeks of gestation. Pediatrics 2004; 114: 297-316.
- Taksande A, Vilhekar K, Jain M, et al. Prediction of the development of neonatal hyperbilirubinemia by increased umbilical cord blood bilirubin. Ind Medica 2005; 9: 5-9.
- Sahu S, Abraham R, John J, et al.. Cord blood albumin as a predictor of neonatal jaundice. JBiomed Res 2013; 2; 436-438.
- Trivedi. Cord serum bilirubin and albumin in neonatal hyperbilirubinemia. Int J Int Sci Inn Tech Sec A 2013; 2: 39-42.
- Bunt JE, Rietveld T, Schierbeek H, et al. Albumin synthesis in preterm infants on the first day of life studied with [1-13C] leucine. Am J PhysiolGastrointest Liver Physiol 2007; 292: 1157-1161.
- Purcell LK, Kennedy TJ, Jangaard KA. Early neonatal discharge guidelines: Have we dropped the ball? Paediatr Child Health 2001; 6: 769-772.
- Burtis CA, Ashwood AR, Bruns DE. Tietz text book of clinical chemistry and molecular diagnosis, 4th ed. Elsevier 2008: 2254.
- Sgro M, Campbell D, Shah V. Incidence and causes of severe neonatal hyperbilirubinemia in Canada. Can Med Assoc J 2006; 175: 561.
- Satrya R, Effendi SH, Gurnida DA. Correlation between cord blood bilirubin level and incidence of hyperbilirubinemia in term new-borns. PaediatricaIndonesiana 2009; 49: 349-354.
- Maisels MJ, Kring E. Length of stay: Jaundice and hospital readmission. Pediatrics 1998; 101: 995-998.
- Taksande A, Vilhekar K, Jain M, et al. Prediction of the development of neonatal hyperbilirubinemia by increased umbilical cord blood bilirubin. IndMedica 2005; 9: 5-9.
- Sun G, Wang YL, Liang JF, Du LZ. Predictive value of umbilical cord bilirubin level for subsequent neonatal jaundice. ZhonghuaErKeZaZhi 2007; 45: 848-852.
- Sahu S, Abraham R, John J, et al. Cord blood albumin as a predictor of neonatal jaundice. Int J Biol Med Res 2011; 2: 436-438.
- Knudsen A. Prediction of the development of neonatal jaundice by increased umbilical cord blood bilirubin. Acta Paediatr Scand 1989; 78: 217-221.
- Awasthi S, Rehman S. Early prediction of neonatal hyperbilirubinemia. Indian J Pediatr 1998; 65: 131-139.
- Trivedi DJ, Markande DM, Vidya BU, et al. Cord serum bilirubin and albumin in neonatal hyperbilirubinemia. Int J IntSci Inn Tech Sec A 2013; 2: 39-42.
- Sahu S, Abraham R, John J, et al. Cord blood albumin as a predictor of neonatal jaundice. Int J Biol Med Res 2011; 2: 436-438.
- Pahuja M, Dhawan S, Chaudhary SR. Correlation of cord blood bilirubin and neonatal hyperbilirubinemia in healthy new-borns. Int J ContempPediatr 2016; 3: 926-930.
- Nahar Z, Mannan SA, Dey SK, et al. The value of umbilical cord blood bilirubin measurement in predicting the development of significant hyperbilirubinemia in healthy new-born. Bangladesh J Child Health 2009; 33: 50-54.
- Trivedi DJ, Markande DM, Vidya BU, et al. Cord serum bilirubin and albumin in neonatal hyperbilirubinemia. Int J Int sci Inn Tech Sec A 2013; 2: 39-42.