Case Report - Current Pediatric Research (2017) Volume 21, Issue 2
Congenital lobar over inflation: A diagnostic challenge
Swarnim S, Divya Mishra, Brajesh Kumar RaiDepartment of Pediatrics, RML Hospital, New Delhi, India.
- *Corresponding Author:
- Swarnim S
Department of Pediatrics
RML Hospital, New Delhi, India.
Tel: +919939453222
E mail: itsswarnim@gmail.com
Accepted date: April 29, 2017
Abstract
Congenital lobar over inflation is a rare congenital malformation of the lung characterized by over inflation of a lobe of the lung due to partial obstruction of the bronchus resulting in compression of normal lung tissue. We are describing two cases of Congenital Lobar over inflation (CLO) which presented in early infancy with severe respiratory distress. One of the cases was initially misdiagnosed as Pneumothorax and CLO were thought of only after chest tube insertion failed to provide any relief in respiratory distress. Both the cases were subsequently managed surgically with lobectomy followed by an uneventful recovery.
Keywords
Congenital lobar overinflation, Lung malformation, Respiratory distress.
Introduction
CLO, previously called congenital lobar emphysema is a rare congenital malformation of lungs. It is characterized by over inflation of pulmonary lobe, with compression and displacement of adjacent normal lung tissues.
The prevalence of CLO is reported to be 1 in 20,000 to 1 in 30, 000 with a male to female ratio is 3:1 [1]. CLO usually involves one lobe, with 47 % involvement of left upper lobe followed by right middle lobe (34%) and right upper lobe (21%) [2]. It presents as life threatening respiratory distress especially within the first 6 months of life due to compression atelectasis, mediastinal shift, hypoxia, and associated hypotension [3].
Case 1
A two months old baby presented to us with six weeks history of cough, wheezing and progressive difficulty in breathing (Figure 1).
On examination, the child was tachypnoeic with severe chest in drawing, chest had decreased expansion, the trachea was shifted to the right and a hyper resonant percussion note was heard over the left anterior thoracic region. Bilateral scattered rhonchi were present. Other systemic examination was normal.
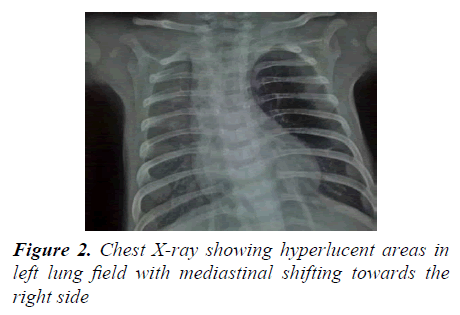
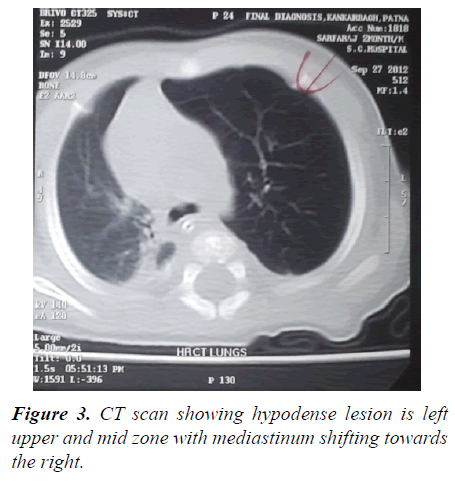
Chest X-ray (Figure 2) showed hyper lucent areas in left lung field with mediastinal shifting towards the right side. CT scan (Figure 3) showed thin walled air density (hypodense) lesion in left the upper and mid zone. Left lower zone and right lung were normal with mediastinum shifting towards the right side.
The diagnosis of CLO was made and the patient was referred to surgery department for surgical management. Postoperatively the patient remained stable with marked improvement in distress seen on follow-up visits of the child.
Case 2
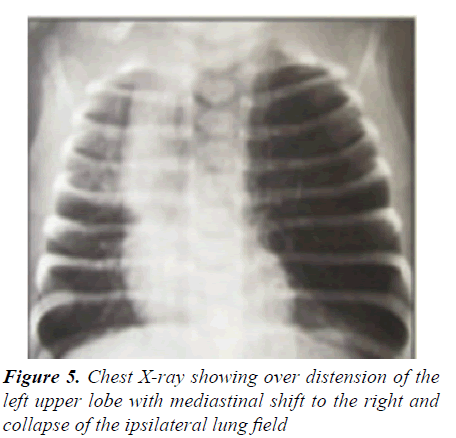
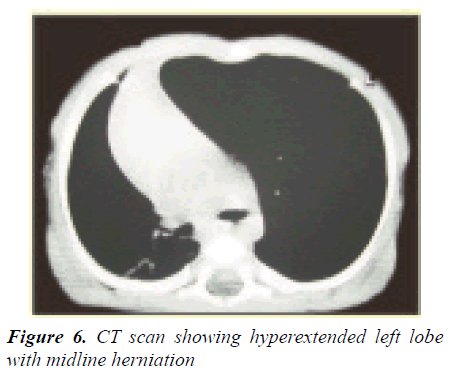
A forty-five days old male baby having severe respiratory distress since birth presented to our hospital after nonresponse to treatment taken at private hospitals (Figures 4-6). There a provisional diagnosis of pneumonia was made initially and the child was given I.V. antibiotics and later on in view of hyper lucency of the left upper lobe with mediastinal shift, pneumothorax was thought of and a chest tube was inserted. In view of no symptomatic relief in the child with any chest expansion on repeat chest X-ray, chest tube was removed and the child was referred to our hospital.
On respiratory examination, less movement of the left upper chest, the trachea was shifted to the right, vocal resonance was decreased on left side and on auscultation diminished breath sound was found on the left side. Other systems appeared normal.
CT scan (Figure 6) showed a hyper lucent hyperextended lobe with midline substantial herniation and compression of the remaining lung. The mediastinum is significantly shifted away from the side of the abnormal lobe.
The diagnosis of CLO was made and the patient was referred to surgery department for surgical management. Conservative management was given; the patient responded well and was referred to surgery department for further surgical management.
Discussion
CLO is characterized by over inflation of pulmonary lobe and is caused by localized bronchial obstruction [4]. Overdistension of the airspaces within a pulmonary lobe leads to air trapping and compressive changes in the remainder of the lung and mediastinal shift away from the increased volume results in compression of the contralateral lung [2,4]. The formation of CLO may be caused by abnormal lobar bronchus development, most often it is a cartilage defect, less frequently a muscular coat defect, mucous membrane fold, stenosis, compression of the abnormally located vessel, tumor, etc. [2]. CLO usually involves one lobe, with 47% involvement of left upper lobe followed by right middle lobe (34%) and right upper lobe (21%) [2]. In some rare cases with bilateral involvement, the patient presents with severe respiratory distress, which needs urgent surgical management [5].
Antenatal diagnosis can be done with Ultrasonography which was missing in our case [6]. The diagnosis, although not definitive, is made by clinical examination and chest X-ray and can be confirmed by CT, as we performed in our case. The condition is most commonly confused with pneumothorax leading to ICD tube insertion as done in one of our cases. A series of 3 cases has been described by Tempe et al. [7] which presented with respiratory distress and were mistakenly diagnosed as pneumothorax and an ICD was inserted in all the 3 cases, but later on, all turned out to be CLE [7]. ICD insertion does not help; rather it may further increase the respiratory distress and lead to injury of the lung parenchyma [8]. In CLE the pulmonary vessels extend to the periphery of the hyperinflated lobe and there is no visualization of a pleural line unlike in pneumothorax. Concomitant Congenital Heart Disease (CHD) is also found in 12 to 20% cases of CLO [9]. There were no such anomalies in our patients. Congenital Lobar Emphysema typically causes unilateral hyperinflation. Since it is hyper-inflated, often there is air trapping and the diseased lung does not take an effective part in the respiratory gas exchange. Also, there can be significant air trapping, which can be later revealed in the pulmonary function tests including plethysmograph [10]. Also, the V-Q scan has shown reduced blood supply to the affected lungs, but it is unavailable at most of the hospitals in a developing country like India [11,12]. Children with CLE can present with hypoxia and decompensated respiratory failure. Under those circumstances, those children may need to augment their respiratory pump and in the clinical setting, it can be evident as orthopnea and tachypnea. It is similar to the animal models, where cats try to use their inspiratory muscle activity to compensate respiratory failure as described by the Physiologist Paul Davenport et al. [12]. Özçelik et al. have described the outcome based comparative analysis of 30 cases of CLE, which showed the majority of the children did very well with conservative management. This observation indicates that there may be a need for a more conservative approach in the developing countries, where many of the families cannot bear the cost of surgical management [13].
Conclusion
CLO is an uncommon condition, but it is a relatively well-recognized cause of infantile respiratory distress. The diagnosis of CLO may present a diagnostic challenge and high index of suspicion in neonates with progressive respiratory distress is important to make any diagnosis.
References
- Kravitz RM. Congenital malformations of the lung. Pediatr Clin North Am 1994; 41: 453-472.
- Martin R, Avroy F, Fanaroff MBCH, et al. Neonatal-perinatal medicine, 9th Edition 2008: 1002-1003.
- Chao MC, Karamzadeh AM, Ahuja G. Congenital lobar emphysema. Int J Pediatr Otorhinolaryngol 2005; 69: 549-554.
- Behrman R, Kliegman R. Nelson Textbook of Pediatrics, Vol2 , 19th Edition, W.B. Saunders Elsevier, Philadelphia 2010: 1742-1803.
- Dewan RK, Kesieme EB, Sisodia A, et al. Congenital malformation of lung parenchyma: 15 years? experience in a thoracic surgical unit. Indian J Chest Dis Allied Sci 2012; 54: 105-109.
- Toyoshima M, Suda T, Chida K. Asymptomatic congenital lobar emphysema in a young adult. Intern Med 2012; 51: 2839-2840.
- Tempe DK, Virmani S, Javetkar S, et al. Congenital lobar emphysema: Pitfalls and management. Annals of Cardiac Anesthesia 2010; 13: 53-58.
- Man DW, Hamdy MH, Hendry GM, et al. Congenital lobar emphysema: Problems in diagnosis and management. Arch Dis Child 1983; 58: 709-712.
- Dogan R, Dogan OF, Yilmaz M, et al. Surgical management of Infant with congenital; lobar emphysema and concomitant heart disease. Heart Surg Forum 2004; 7: E644-E649.
- Eigen H, Lemen RJ, Waring WW. Congenital lobar emphysema: Long-term evaluation of surgically and conservatively treated children 1-4. American Review of Respiratory Disease 1976; 113: 823-831.
- Markowitz RI, Mercurio MR, Vahjen GA, et al. Congenital lobar emphysema: The roles of CT and V/Q scan. Clin Pediatr 1989; 28: 19-23.
- Mondal P, Hasan AM, Saha A, et al. Effect of laparotomy on respiratory muscle activation pattern. Physiol Rep 2016; 4: e12668.
- Ãzçelik U, Göçmen A, Kiper N, et al. Congenital lobar emphysema: Evaluation and long-term follow-up of thirty cases at a single center. Pediatr Pulmonol 2003; 35: 384-391.