Research Article - Biomedical Research (2017) Volume 28, Issue 4
Complications and success rates of stellate ganglion blockade; blind technique vs. fluoroscopic guidance
Haktan Karaman*Department of Pain Management Centre, Dicle University, Diyarbakir, Turkey
- *Corresponding Author:
- Haktan Karaman
Department of Pain Management Centre
Dicle University, Diyarbakir, Turkey
Accepted date: September 14, 2016
Abstract
Objective: Stellate Ganglion Blockade (SGB) is a cervical sympathetic blockade technique that has been long applied for a variety of purposes in Anesthesiology and Pain Clinics. In this study, our goal is to reveal the kind of SGB complications, their frequency and success rates of SGBs based on the application methods (blind technique vs. fluoroscopy guidance).
Material and Methods: This retrospective study was conducted in the pain management center of a university hospital using patients’ chart. Patients’ charts compilation began in January 2004 and ended in June 2014. Then, the patient charts collected for the study were divided into two groups: the ones applied with blind techniques (Group-B) and the ones applied under fluoroscopy (Group-F). Thus, 223 patients in Group-B and 197 patients in Group-F, in total, data of 420 patients were collected.
Results: Complications were seen in fourteen patients in Group-B, while twelve of them were blood aspirations due to the vertebral artery puncture. This puncture was observed in eight patients of Group- F. No statistically significant difference was observed between the groups when compared in terms of complications (P=0.311). However, two patients in blind technique group were developed pneumothorax. Block failures of 6.28% in Group-B and 1.52% in Group-F were determined when compared in terms of failure rates. This difference between the two groups was statistically significant (P=0.016).
Conclusion: Complication rates are low and success rates are considerably high, if SGB is applied by experienced hands, even if with blind method.
Keywords
Complications, Stellate ganglion blockade, Sympathetic blocks, Fluoroscopy, Blind technique
Introduction
The sympathetic nervous system is a system controlling “involuntary homeostatic human activity" directly, and having an important role in vascular and visceral pain. Stellate Ganglion Blockade (SGB) is a cervical sympathetic blockade technique that has been long applied for a variety of purposes in Anesthesiology and Pain Clinics [1]. Sympathetic flow is interrupted in head, neck and upper extremity by SGB, and thus peripheral vasodilatation develops [2,3]. At the same time, a pain relief emerges in sympathetically chronic pains in these regions with SGB [4]. Therefore, SGB is applied in a wide range of indication fields for therapeutic and diagnostic purposes. While it is applied as a therapeutic in cases such as complex regional pain syndrome (CRPS), phantom limb pain, vascular headache, Raynaud's phenomenon, arterial embolism, conditions in which drugs applied intra-arterial by accident, Meniere's syndrome, pulmonary embolism, cardiac arrhythmias, refractory angina, perimenopausal hot flashes, herpes zoster and post-herpetic neuralgia, combat-related posttraumatic stress disorder, to treat digital ischemia in a patient with sepsis and to relieve symptoms and pain and to prevent facial nerve damage; it is applied also as a diagnostic in determination of hyperhidrosis etiology and diagnosis of diseases such as Raynaud’s phenomenon [5-17].
As stellate ganglion shows a very close neighborhood to the vital main structures, incorrect application of SGB may lead to many serious complications which can be crippling and even fatal [18]. Serious complication rate based on SGB is reported as 0.17% in a large series study [19]. This situation has recently caused SGB, which are often applied with blind technique, to be applied in company with the devices such as fluoroscopy and ultrasound (USG). This led to an effort to reduce the frequency of complications and increase the chances of successful SGB. Fluoroscopy-guided SGB has important advantages such as allowing detailed visualization of the bone structures and avoiding a possible incorrect intravascular, epidural or intrathecal injection by using opaque substance [2,20]. However, requirement of special training and experience in fluoroscopy and exposure to radiation during the application, and similarly requirement of special training and experience in SGB application under USG leads to SGB applications that widely performed with blind technique. In this study, all SGBs applied by the author of this article in a pain center between 2004-2014 years are compiled retrospectively. Our goal is to reveal the kind of SGB complications, their frequency and success rates of SGB based on the application methods (blind technique vs. fluoroscopy guidance) and contribute to the literature in this area through this article including a relatively large series of cases.
Materials and Methods
Study design and setting
After obtaining approval from the institutional review board, this retrospective study was conducted in the pain management unit of a university hospital using patients’ chart. Patients’ charts compilation began in January 2004 and ended in June 2014. All patients included to this study had been provided written and oral information related to the intervention and treatment modality, and written consent had been obtained from all of them. Routinely, Follow-up period was determined immediately and 3 weeks after interventions for these interventions in our center.
Then, the patient charts collected for the study were divided into two groups: the ones applied with blind techniques (Group-B) and the ones applied under fluoroscopy (Group-F). SGB applications in our clinic are generally performed "at random" either with blind technique or under fluoroscopy. If fluoroscopy was selected for a known purpose (for example, cases expected to be difficult because of anatomical characteristics), these patients were excluded in order to avoid unfavorable effect to the results of the study. Patients without satisfactory data in their chart were also excluded. Thus, 223 patients in Group-B and 197 patients in Group-F, in total, data of 420 patients were collected.
Participants
The following criteria were used for SGB as indications:
1. Raynaud's Phenomenon
2. Hyperhidrosis in their armpits and/or in their hands
3. Neuropathic pain due to various etiologies (CPRS, postherpetic neuralgia, etc.).
The following criteria were used for SGB as contraindications:
1. Anticoagulant therapy
2. Pneumothorax or pneumonectomy on other side
3. Cardiac conduction anomaly
4. Glaucoma
5. Recent MI
6. Bilateral application
7. The presence of psychiatric disorder
8. Presence of general contraindications to invasive procedures (e.g., hemorrhagic diathesis, systemic infection or local infection where the procedure is to be applied, and a known history of allergies to substances that are to be used).
Procedures
Sedation was not applied as far as possible in order not to miss out possible complications in any patient, whether with blind technique or under fluoroscopy. Whichever method is applied, all patients was informed about the process once again just before the interventions. To reduce the possibility of having any complication, they were asked not to move, not to gulp and not to speak in no way until the end of the operation. All applications were performed in an operating room where allowing emergency interventions. No matter which application would be performed, the patients were fully monitored including electrocardiogram (EKG), tension arterial (TA), heart rate (HR) and pulse oximetry (SpO2) and were taken into the application with an IV solution. Strict sterilization rules were never neglected even if the application was just "an injection". In the operating room, after undergoing routine monitoring, they were placed in the supine position on the table. In order to facilitate the application, hyperextension of the head was achieved by placing a pillow between two scapulas of each patient. The area where the procedure was to be performed was cleaned with an iodine antiseptic solution and draped to maintain a sterile environment. So as not to mask potential complications, in general, sedation was not preferred.
However, when necessary, for light sedation, 1-3 mg midazolam and/or 50-100 μg fentanyls were given intravenously. Local anesthetic was applied subcutaneously with a 1% lidocaine infiltration.
Blind technique
Anterior approach was preferred in all applications. 10 mL injector with green needle containing medication was prepared for the application. 1% lidocaine was used in diagnostic blockade, while 0.25% bupivacaine+steroid mixture were used in prognostic blocks. Application was started after recording the initial vital values. Cricoid Cartilage was selected as the sign point. A skin wheal is made over the anterolateral aspect of the body of C6 with 1 mL of local anesthetic with a 25- gauge needle. Transverse process of cervical vertebra (Chassaignac's tubercle) is felt through deep palpation by pulling sternocleidomastoid muscle and carotid sheath in the immediately lateral of cricoid cartilage with 2nd and 3rd fingers of the left hand. Skin is vertically punctured with a 21G syringe containing medication, and then advanced until C6 transverse process is contacted. In this point, the needle tip is retracted 1-2 mm and it is assured that BOS and /or blood do not come with aspiration.
Thereafter, medication is injected in a controlled and slow manner. Patient's head is raised immediately after the application and observed on the table for 10 minutes in this position. If there is no complication, the patients are taken to their beds for 1 hour. At this time, effectiveness of the block is evaluated.
Fluoroscopy guidance technique
While the patients, who were prepared as in the blind technique, are PA position at fluoroscopy table, C6 vertebra transverse process is targeted with a 100 mm stimulator needle in the style of "tunnel vision". By retracting the needle 1-2 mm after contacting the bone, it is necessary to see if the opaque material of 0.5 mL is spread properly. Also, it is vital to be sure that vascular leakage does not exist or there is no spread towards BOS. If everything is fine, the prepared medication is injected carefully and slowly. Similarly, patient's head is raised immediately after the application and monitored on the fluoroscopy table for 10 minutes. If there is no complication, the patients are taken to their beds for 1 hour. At this time, effectiveness of the block is evaluated as in the blind technique.
Effectiveness of SGBs
• Patients were evaluated after one hour according to their initial diagnosis.
• For Hyperhidrosis: Horner's syndrome + significant reduction in sweating.
• Raynaud's phenomenon: Horner's syndrome + getting pink and warming up in the hands
• Neuropathic pain: Horner's syndrome + pain reduction
Outcome measurements
Patients' ages, gender, applied side of the SGB, the applied blockade method, SHP block indication, success and complications were documented for statistical evaluation.
Statistical methods
All data were analyzed using MedCalc Statistical Software version 16.2.1 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2016). Chi-squared test was applied to investigate the homogeneity between groups in terms of gender, blockage application side and diagnosis. Independent samples T-test was used to investigate homogeneity between groups in terms of age. Chi-squared test was used to investigate the differences between groups in terms of complication frequencies and failure rates. P<0.05 was considered statistically significant in all analyses.
Results
Demographic characteristics
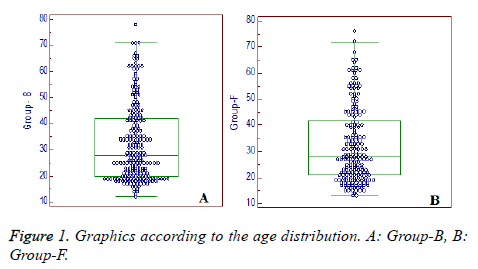
420 patients in total were included in the study. 223 of these patients were applied SGB with blind technique and remaining 197 patients were applied SGB under fluoroscopy. Groups were similar when gender rates, age, diagnosis and SGB application sides were compared (Table 1). It drew attention that numbers of patients were not normally distributed in terms of age in both groups and there were been clustered in the younger age groups (Figure 1). Other parameters (gender, diagnosis, side) were observed to be normally distributed.
| Group-B | Group-F | P-value | |
|---|---|---|---|
| Total (n) | 223 | 197 | |
| Years (n) | |||
| 2004 | 27 | 1 | - |
| 2005 | 19 | 29 | |
| 2006 | 25 | 15 | |
| 2007 | 18 | 19 | |
| 2008 | 21 | 28 | |
| 2009 | 26 | 23 | |
| 2010 | 28 | 22 | |
| 2011 | 18 | 21 | |
| 2012 | 21 | 13 | |
| 2013 | 15 | 24 | |
| 2014 | 5 | 2 | |
| Gender | |||
| K | 121 | 101 | 0.54 |
| E | 102 | 96 | |
| Patients’ diagnosis | |||
| Raynaud's Phenomenon | 70 | 65 | 0.587 |
| Hyperhidrosis | 70 | 68 | |
| Neuropathic pain | 83 | 64 | |
| Side | |||
| Right | 113 | 95 | 0.617 |
| Left | 110 | 102 | |
| Age (year) | |||
| Mean ± SD | 32.59 ± 14.69 | 32.27 ± 14.43 | 0.826 |
| Range | 12 to 78 | 13 to 76 | |
| Group-B : blind technique; Group-F: fluoroscopic guidance; SD: Standard Deviation | |||
Table 1. Demographic characteristics of patients.
Complications and failure rates of SGBs
Complications were seen in fourteen patients in Group-B, while twelve of them were blood aspirations due to the vertebral artery puncture. This puncture was observed in eight patients of Group-F (Table 2). No patients in both groups were observed with any other complications related to this puncture and a successful blockage was applied then by repositioning the needle tip. No statistically significant difference was observed between the groups when compared in terms of complications (P=0.311). However, two patients in blind technique group were developed pneumothorax. Development of serious pneumothorax was observed in these patients in PA chest radiography taken at the onset of severe chest pain immediately after the intervention (in approximately 30 minutes). Hereupon, patients were directed to the thoracic surgery clinic to be inserted with chest tube. These patients were discharged without any sequela after staying with chest tube during three days. Block failures of 6.28% in Group-B and 1.52% in Group-F were determined when compared in terms of failure rates. This difference between the two groups was statistically significant (P=0.016) (Table 2).
| Group-B (n:223) | Group-F (n:197) | p-value | |
|---|---|---|---|
| Complications n (%) | 14 (%6.28) | 8 (%4.06) | 0.485 |
| Bleeding | 12 | 8 | |
| Pnömotoraks | 2 | 0 | |
| Failure Rate n (%) | 14 (%6.28) | 3 (%1.52) | 0.016* |
| *Statistically significant value | |||
Table 2. The complications and failure rates of stellate ganglion blockade.
Discussion
SGB is not an intervention without risks. Although rarely, vertebral artery injection, subarachnoid block, phrenic nerve blocks and recurrent laryngeal nerve block are serious complications that may be encountered irrespective of the technique used (blind or guidance), because of close neighborhoods [21]. SGB on the right side may cause a significant prolongation of the QT interval and QT dispersion [22]. When we scanned PubMed in terms of publications reporting SGB complications, we saw that these kinds of studies were clustered in 1950's. After all these publications that we cannot reach even their abstracts, Wulf and Maier's study [16] published in 1992 and involving a very large series of cases can be considered as probably the most important study. Authors examined approximately 45.000 SGB in terms of complications and they reported serious complications as 0.17%. Most of these complications were reported to be CNS complications such as convulsions, a high spinal block (developed in 6 cases), a high epidural block (developed in 3 cases), pneumothorax (developed in 9 patients) and allergic reaction (developed in 2 patients). It is possible to interpret the results of these studies as SGB complications with blind technique, because the applications were performed with blind technique in the period when they were published. Apart from this, it is possible to encounter different complications in the literature in the form of case reports with blind technique. Saxena et al. [23] reported in their case report published in 2004 that they encountered sinus arrest which is an extraordinary complication developed after right-sided SGB with blind method.
Sarı and Aydın [24] reported in their case report that they encountered complications in two SGB applications with blind technique, and they recommended that SGB should be applied under visualization guidance. Kimura et al. [25] reported seven patients who developed severe hypertension (systolic arterial pressure >200 mm Hg) after SGB in their pain center. They postulated that diffusion of the local anesthetic along the carotid sheath might produce vagal blockade causing unopposed sympathetic activity as a result of attenuation of the baroreceptor reflex. Chaturvedi and Dash [26] reported in their case report that a "locked-in" syndrome developed during SGB application with blind method due to the intra-arterial injection of local anesthetic. They stated that the patient could not move, talk and breathe during these unusual complications, although patient did not lose his consciousness. Pneumothorax is one of the most complications of SGB. Because of very close neighborhood to apex of the lung, the probability of encountering this complication increases with SGB applied under C6 level. Therefore, this complication is seen almost always blind method. Indeed, in our study, this complication was developed in two patients with blind technique. These patients who were recovered without sequel directed us to apply SGB under visualization guidance. Indeed, Makharit et al. [13] reported that they encountered no serious complications in 64 patients included in their study in which they researched the effect of early SGB under fluoroscopy guided to treat facial pain related to Acute Herpes Zoster. Also, in a study that was performed 250 SGBs for the management of PTSD symptoms, McLean [27] reported that they do not encounter immediate or delayed complications.
Another popular application method is the application of SGB under USG guidance. However, unfortunately, this practice has not been exempt from complications. Indeed, Shankar and Simha [28] reported the development of transient neuronal injury in their case report, although SGB was applied under USG guidance by an experienced pain physician. However, complications are generally low under USG guidance in the studies we were scanned. For example; Wei et al. [29] presented total of 156 SGBs results applied under USG guidance in 16 patients with CRPS. They reported that the frequency of mild complications (such as hoarseness, dysphagia) was 13.5% and that they did not encountered serious complications (such as plexus paresis or puncture of veins or other structures by accident) Similarly, Garneau et al. [30] reported that they encountered no complications in SGB applied under USG guidance to 40 patients including a control group. Also, ultrasound guided SGBs using lateral in-plane technique at C7 level were performed in 20 patients suffering from chronic pain of upper extremity, head, and neck using 4 ml of 0.25% bupivacaine + 1 ml of 40 mg triamcinolone mixture by Ghai et al. [31]. They reported that only hoarseness of voice was seen in four patients, and reported that there was no delayed complication.
Another issue we do not encounter in the literature is our comparison of success rates of two techniques in our study. We think that this situation will be important in determination of the method to be selected for the SGB application. Whether under fluoroscopy guided or under USG guided, the chances of success of SGB applied under visualization are very high compared to the SGB applied the blind method because anatomical landmark can be determined quite accurately. Indeed, we see that a statistically high rate of success is achieved in fluoroscopy group in our study (1.52% vs. 6.28%). Another point needs to be emphasized about the complications should be directed to the use of the drug. In applications such as SGB, it should attention drugs of choice due to close proximity to the vertebral artery. We never prefer particulate steroid for such applications. As a result of accidental escape of such drugs to vertebral artery, it can lead to quite fatal and irreversible outcomes. Therefore, the steroids without particulate (methylprednisolone, dexamethasone, betamethasone) must be preferred instead of the steroids with particulate in these regions. The most important limiting factor in our study is that our study was conducted retrospectively. However, when we scan the literature until today, we see quite few studies comparing stellate ganglion blockage complications and success rates. In this regard, we think that our study is an important contribution to the literature with its relatively large number of cases. In addition, we think that application of SGB by same person will give more precise and correct information, far from complications and interpersonal differences in success rates.
Conclusion
In conclusion we see that complication rates are low and success rates are considerably high, if SGB is applied by experienced hands, even if with blind method. However, it is important to express clearly that although there were no statistically significant difference in complication frequency when compared to the SGB under fluoroscopy, we think that to prefer SGB applying under visualization guidance is an appropriate way to reduce complication rates such as pneumothorax and to increase the success rates of SGB.
References
- Dönmez A, Tufan H, Tutar N, Araz C, Sezgin A, Karadeli E, Torgay A. In vivo and in vitro effects of stellate ganglion blockade on radial and internal mammary arteries. J Cardiothorac Vasc Anesth 2005; 19: 729-733.
- Zhang L, Yao J, Zhang T, Jin J, Zeng X, Yue Z. Stellate ganglion block may prevent the development of neurogenic pulmonary edema and improve the outcome. Med Hypotheses 2013; 80: 158-161.
- Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician 2000; 3: 294-304.
- Charlton J. Complex regional pain syndrome. In: Charlton J, editor. Corecurriculum for professional education in pain. Seattle: IASP press; 2005, 201-204.
- Schürmann M, Gradl G, Wizgal I, Tutic M, Moser C, Azad S, Beyer A. Clinical and physiologic evaluation of stellate ganglion blockade for complex regional pain syndrome type I. Clin J Pain 2001; 17: 94-100.
- Faxon HH, Flynn JH, Anderson RM. Stellate block as an adjunct to the treatment of pulmonary embolism. N Engl J Med 1951; 244: 586-590.
- Yanagida H, Kemi C, Suwa K. The effects of stellate ganglion block on the idiopathic prolongation of the Q-T interval with cardiac arrhythmia (the Romano-Ward syndrome). Anesth Analg 1976; 55: 782-787.
- Chester M, Hammond C, Leach A. Long-term benefits of stellate ganglion block in severe chronic refractory angina. Pain 2000; 87: 103-105.
- Lipov EG, Lipov S, Joshi JR, Santucci VD, Slavin KV, Beck Vigue SG. Stellate ganglion block may relieve hot flashes by interrupting the sympathetic nervous system. Med Hypotheses 2007; 69: 758-763.
- Lipov E, Kelzenberg BM. Stellate ganglion block (SGB) to treat perimenopausal hot flashes: clinical evidence and neurobiology. Maturitas 2011; 69: 95-66.
- Lipov EG, Joshi JR, Sanders S, Slavin KV. A unifying theory linking the prolonged efficacy of the stellate ganglion block for the treatment of chronic regional pain syndrome (CRPS), hot flashes, and posttraumatic stress disorder (PTSD). Med Hypotheses 2009; 72: 657-661.
- Alino J, Kosatka D, McLean B, Hirsch K. Efficacy of stellate ganglion block in the treatment of anxiety symptoms from combat-related post-traumatic stress disorder: a case series. Mil Med 2013; 178: e473-476.
- Makharita MY, Amr YM, El-Bayoumy Y. Effect of early stellate ganglion blockade for facial pain from acute herpes zoster and incidence of postherpetic neuralgia. Pain Physician 2012 ; 15: 467-474.
- Raj PP. Practical Management of Pain, 3rd Ed. St Louis: Mosby, 2000:651-682.
- Bataille B, Nucci B, Mora M, Silva S, Cocquet P. Ultrasound-guided bilateral stellate ganglion blockade to treat digital ischemia in a patient with sepsis: a case report. Can J Anaesth 2016; 63: 56-60.
- Lipov E, Ritchie EC. A review of the use of stellate ganglion block in the treatment of PTSD. Curr Psychiatry Rep 2015; 17: 599.
- Gogia AR, Chandra KN. Stellate ganglion block can relieve symptoms and pain and prevent facial nerve damage. Saudi J Anaesth 2015; 9: 204-206.
- Siegenthaler A, Mlekusch S, Schliessbach J, Curatolo M, Eichenberger U. Ultrasound imaging to estimate risk of esophageal and vascular puncture after conventional stellate ganglion block. Reg Anesth Pain Med 2012; 37: 224-227.
- Wulf H, Maier C. Complications and side effects of stellate ganglion blockade. Results of a questionnaire survey. Anaesthesist 1992; 41: 146-151.
- Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician 2000; 3: 294-304.
- Hey M, Wilson I, Johnson MI. Stellate ganglion blockade (SGB) for refractory index finger pain - a case report. Ann Phys Rehabil Med 2011; 54: 181-188.
- Biernawska J, Kaźmierczak J, Kotfis K, Żukowski M. The influence of regional anaesthesia and local anesthetics on cardiac repolarization. Anaesthesiol Intensive Ther 2016; 48: 135-141.
- Saxena AK, Saxena N, Aggarwal B, Sethi AK. An unusual complication of sinus arrest following right-sided stellate ganglion block: a case report. Pain Pract 2004; 4: 245-248.
- Sarı S, Aydın ON. Complication belong to stellate ganglion blockade after cervical trauma. Agri 2014; 26: 97-100.
- Kimura T, Nishiwaki K, Yokota S, Komatsu T, Shimada Y. Severe hypertension after stellate ganglion block. Br J Anaesth 2005; 94: 840-842.
- Chaturvedi A, Dash H. Locked-in syndrome during stellate ganglion block. Indian J Anaesth 2010; 54: 324-326.
- McLean B. Safety and Patient Acceptability of Stellate Ganglion Blockade as a Treatment Adjunct for Combat-Related Post-Traumatic Stress Disorder: A Quality Assurance Initiative. Cureus 2015; 7: e320.
- Shankar H, Simhan S. Transient neuronal injury followed by intravascular injection during an ultrasound guided stellate ganglion block. Anesth Pain Med 2013; 134-137.
- Wei K, Feldmann RE Jr, Brascher AK, Benrath J. Ultrasound-guided stellate ganglion blocks combined with pharmacological and occupational therapy in Complex Regional Pain Syndrome (CRPS): a pilot case series ad interim. Pain Med 2014; 15: 2120-2127.
- Garneau SY, Deschamps A, Couture P, Levesque S, Babin D, Lambert J, Tardif JC, Perrault LP, Denault AY. Preliminary experience in the use of preoperative echo-guided left stellate ganglion block in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth 2011; 25: 78-84.
- Ghai A, Kaushik T, Kundu ZS, Wadhera S, Wadhera R. Evaluation of new approach to ultrasound guided stellate ganglion block. Saudi J Anaesth 2016; 10: 161-167.