Research Article - Current Pediatric Research (2018) Volume 22, Issue 1
Complementary feeding timing and its predictors among mother's of children aged (6-23) months old in Halaba Kulito town, Southern Ethiopia.
Desalegn Tsegaw Hibstu1*, Dawit Jember Tesfaye2, Teshome Abuka Abebo1, Fanuel Belayneh Bekele21Department of Reproductive Health, School of Public Health, College of Medicine and Health Sciences, Hawassa University, Ethiopia.
2Department of Epidemiology, School of Public Health, College of Medicine and Health Sciences, Hawassa University, Ethiopia.
- Corresponding Author:
- Desalegn Tsegaw Hibstu
Department of Reproductive Health
School of Public Health, College of Medicine and Health Sciences Hawassa University, Ethiopia
Tel: +251917187974
E-mail: desuethiopia@yahoo.com
Accepted date: February 22, 2018
Abstract
Background: Infants are at an increased risk of malnutrition from six months of age onwards and hence timely initiation of nutritionally enough, reliable, age appropriate complementary feeding is urged for improved health and development of infants. The aim of this study was to assess the magnitude and associated factors of timely initiation of complementary feeding in Halaba Kulito town, Southern Ethiopia. Method: A community-based cross-sectional study was conducted from May 30 to June 4, 2016 among 320 mothers with their 6-23 months using systematic random sampling technique. Data was collected using pretested and interviewer administered structured questionnaire. Bivariate and multivariate logistic regression was carried out using SPSS version 20.0 software. Result: The magnitude of complementary feeding timing was 57.8%. Maternal education (AOR=4.18, CI: 1.02, 17.20), age at first pregnancy (AOR=5.82, CI: 2.45, 13.81) were predictors while maternal job status (AOR=0.49, CI: 0.07, 3.51) and paternal job status (AOR=0.16, CI: 0.06, 0.42) were negative predictors of complementary feeding timing. Conclusion: Nearly, three among five mothers (57.8%) initiated complementary feeding timely. Maternal education, age at first pregnancy and maternal and paternal occupational status were the main factors for timely initiation of complementary feeding. Women education, health education dissemination strategies using mass media as a vehicle and through Health Extension workers need to be considered to improve timely initiation of complementary feeding.
Keywords
Complementary feeding timing, Children, Age.
Introduction
Complementary feeding is providing young children additional foods or fluids besides breast feeding at six months of infancy [1]. The World Health Organization advocates breast feeding alone for six months of age with the addition of complementary feeds at six months of age [2,3].
Appropriate nutrition during early childhood is vital to a child’s development. Breastfeeding alone is vital and enough for the first six months. Nevertheless, young children are at risk of malnutrition from six months of age a head, when breast milk alone is no longer sufficient to satisfy all their nutritional demands and, hence, timely introduction of nutritionally enough, reliable, age appropriate complementary foods at sixth month of age is advocated for improved health outcome of infants [4].
Studies revealed that introduction of adequate and safe complementary foods timely reduced the risk of malnutrition, morbidity and mortality [5,6]. For instance, complementary feeding actions exclusively were indicated to avoid nearly one fifth of under-five mortality in developing countries [7,8]. Inadequate amounts and poor quality of complementary foods, poor childhood feeding habits, and increased rates of morbidity have a prejudicial outcome on health and growth among young children. Even with continuous breast feeding, children will experience stunting, future learning difficulty and lack of immunity without ample dietary variety and meal frequency at 6 months of age and above [9-12].
The magnitude of complementary feeding timing varies across countries. For instance, a study in china showed that of complementary feeding timing was 41.6% and maternal age, maternal education, employment and infant’s sexes were identified predictors with complementary feeding timing [13]. Studies conducted in India indicated that more than 75% of mothers had initiated complementary feeding at 6 month [14,15]. While a finding in Ghana showed that 55% of mothers had introduced other foods besides breast-milk with the age of 3-4 months [16].
Malnutrition stays one of the principal public health problems in Ethiopia that causes 53% of infant and child mortality. According to 2011 and 2014 Ethiopian Demographic Health survey (EDHS), 44% and 40% of under- five children were stunted [17,18]. The 2011 EDHS showed that timely initiation of complementary feeding in Ethiopia was 51% [17]. Other recent studies in Ethiopia indicated that the magnitude of timely initiation of complementary feeding was 62.8%, 57.1% and 71.3% [19-21]. Therefore, this study was aimed to determine the magnitude and predictors of complementary feeding timing in Halaba Kulito town, Southern Ethiopia.
Methods
Study Design and Setting
Community-based cross-sectional study was conducted in Halaba Kulito town from May 30 to June 10, 2016. The town is located 90 kilometer (KM) from Hawassa, capital city of Southern Nation, Nationalities and People Region, Ethiopia and 315 KM from Addis Ababa, Ethiopia. The town has 5 urban Kebeles (Kebele: the smallest administrative unit in Ethiopia). The total population of the town is 38,597, with 19,684 (51%) of are females and 5380 are under-five children. In the district, there are two hospitals, nine health centers & seventy nine health posts providing promotive, preventive and curative services [22].
Selection of Study Participants
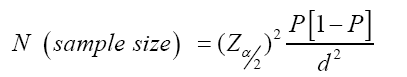
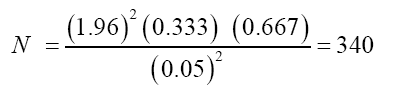
The source populations were all mothers having underfive children and the study populations were all mothers having infants and young children aged 6-23 months old. Sample size was determined using single population proportion formula considering 95% confidence level, 5% margin of error (d) and proportion (p) of timely initiation of complementary feeding taken as 33.3% [23].
Simple random sampling technique was used to select two Kebeles (Murata and Denebafama) from five Kebeles (Denebafama, Murata, Lendaber, Wanjaber and Mehalarada). Study participants were selected by systematic random sampling technique. The total number of children (age 6 to 23 months old) were obtained from family folder records of health extensions workers. The sampling interval was calculated by dividing the total children (1360) by the sample size (340).
Operational Definition
According to the WHO recommendations, the following operational definitions were considered: Complementary feeding is the process of starting additional foods when breast milk alone is no longer sufficient to meet the nutritional requirements of infants. Complementary feeding timing: is introduction of additional supplementary food for young child at sixth months of age along with continued breast feeding.
Data Collection Tool and Procedure
Pre-tested and interviewer-administered structured questionnaire was used to collect quantitative data. The questionnaire was prepared in English language and translated to Amharic language and back to English language. Five registered female nurses were recruited to collect the data. Training was given to data collectors for two days. Two bachelor degree holders with principal investigators supervised the data collection process and checked filled questionnaire for consistency and completeness.
Data Processing and Analysis
After data collection, data were edited and cleaned before analysis, each questionnaire was checked for completeness and code was given. Data were entered into computer using EPI Info version 3.5.3 and the analysis was done using SPSS version 20.0. Frequency, percentage and descriptive summaries were used to describe the study variables. Logistic regression was carried out to identify factors associated with timely initiation of complementary feeding. Variables with p-value ≤ 0.2 in the bivariate analysis were selected as candidate variables for multivariable logistic regression analysis to control the effect of confounders. Adjusted odds ratios with their 95% confidence intervals (CI) and p-value of less than 0.05 were considered to have significant association between the outcome and the explanatory variables. The model fitness was checked using Hosmer and Lemeshow.
Results
Socio-Demographic Characteristics
A total of 320 (94.1%) mothers of children (aged 6-23 months old) were included in the study. The mean ages of mothers and children were 26.57 years (± 5.63, standard deviation (SD)), and 13.65 months (± 5.53 SD), respectively. One hundred two (32%) of mothers were in the age range of 25-29 years. Nearly half, 156 (49%) were followers of Muslim religion and 306 (96%) mothers married with average family size of 4.23 (± 1.36 SD).
Only 126 (40%) of mothers attended primary education and 106 (33 %) of their partners/husbands attended secondary and above school. Almost seven among ten mothers, 228 (71%) were house wife by occupation and half, 159 (50%), of their counterpart were merchant. Three among ten, 99 (31 %) mothers had income between 1001 and 2000 Ethiopian birr (≈ 46 USD – 93 USD) per month (Table 1).
| Variables | Category | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Maternal age | 15-19 | 26 | 8.1 |
| 20-24 | 91 | 28.4 | |
| 25-29 | 102 | 31.9 | |
| 30-34 | 64 | 20.0 | |
| ≥ 35 | 37 | 11.6 | |
| Religion | Muslim | 156 | 48.8 |
| Orthodox | 95 | 29.7 | |
| Protestant | 69 | 21.6 | |
| Ethnicity | Halaba | 121 | 37.8 |
| Kembata | 65 | 20.3 | |
| Siliti | 45 | 14.1 | |
| Guraghe | 48 | 15. | |
| Amhara | 41 | 12.8 | |
| Marital status | Single | 14 | 4.4 |
| Married | 306 | 95.6 | |
| Family size | ≤ 4 | 203 | 63.4 |
| >4 | 117 | 36.6 | |
| Maternal education | Unable to read and write | 63 | 19.7 |
| Read and write | 81 | 25.3 | |
| Primary education | 126 | 39.4 | |
| Secondary and above | 50 | 15.6 | |
| Parental education | Unable to read and write | 35 | 10.9 |
| Read and write | 48 | 15.0 | |
| Primary education | 131 | 40.9 | |
| Secondary and above | 106 | 33.1 | |
| Maternal occupation | Governmental employed | 33 | 10.3 |
| Housewife | 228 | 71.3 | |
| Daily laborer | 26 | 8.1 | |
| Merchant | 32 | 10.0 | |
| Paternal occupation | Governmental employed | 88 | 27.5 |
| Daily laborer | 73 | 22.8 | |
| Merchant | 159 | 49.7 | |
| Monthly income | <1000 birr | 80 | 25.0 |
| 1001-2000 birr | 99 | 30.9 | |
| 2001-3000 birr | 65 | 20.3 | |
| >3001 birr | 76 | 23.8 |
Table 1: Socio demographic and economic characteristics of study subjects in Halaba Kulito town, Southern Ethiopia, 2016
Reproductive History
One hundred six (33%) study participants had their first time pregnancy in the age range 20-24 years with mean age of 24.4 (SD ± 5.58) years old. Nearly three among five, 194 (60.6%) of mothers gave birth greater or equal to two children with average pregnancy of two (SD ± 1.19). One hundred twenty three (38.4%) mothers visited health facility four times in all trimester for antenatal care visit. Two hundred forty four (76%) mothers gave birth at health facility (Table 2).
| Variables | Category | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Age at first pregnancy | 15-19 | 71 | 22.2 |
| 20-24 | 106 | 33.1 | |
| 25-29 | 92 | 28.8 | |
| ≥ 30 | 51 | 15.9 | |
| Sex of child | Male | 163 | 50.9 |
| Female | 157 | 49.1 | |
| Age of child in month | 6-10 | 109 | 34.1 |
| 11-15 | 92 | 28.8 | |
| 16-20 | 77 | 24.1 | |
| ≥ 20 | 42 | 13.1 | |
| Number of parity | 1 | 126 | 39.4 |
| ≥ 2 | 194 | 60.6 | |
| ANC follow up | First visit | 7 | 2.2 |
| Second visit | 33 | 10.3 | |
| Third visit | 154 | 48.4 | |
| Fourth Visit | 123 | 38.4 | |
| Place of delivery | HC | 244 | 76.3 |
| Hospital | 47 | 14.7 | |
| Home | 29 | 9.1 | |
| Had complementary feeding information | Yes | 311 | 97.2 |
| No | 9 | 2.8 | |
| Source of Complementary feeding information | Husband | 19 | 5.9 |
| Grand mother | 15 | 4.7 | |
| Health extension worker | 286 | 89.4 | |
| Type of complementary food introduced | Liquid | 110 | 34.4 |
| Semi solid | 48 | 15.0 | |
| Solid | 40 | 12.5 | |
| Mixed( solid and liquid) | 122 | 38.1 | |
| Frequency of complementary feeding during sickness | Same before | 121 | 37.8 |
| More than before | 101 | 31.6 | |
| Less than before | 98 | 30.6 |
Table 2: Reproductive history and complementary feeding related characteristics of study participants in Halaba Kulito town, Southern Ethiopia, 2016
Complementary Feeding Timing
One hundred eighty five (57.8%) mothers of children (aged 6-23 months) initiated complementary feeding timely. Ninety eight (30.6%) mothers fed their children less than before due to illness. Three hundred eleven (97%) mothers were informed about timing of complementary feeding. Nine in ten, 286 (89.2%) mothers obtained information about complementary feeding timing from health extension workers. One hundred ten (34.4%) mothers introduced liquid foods for their babies as complementary food (Table 2).
Predictors of Complementary Feeding Timing
In the multivariable logistic regression analysis, age at first pregnancy, maternal education, maternal and paternal occupations were significantly associated with complementary feeding timing.
Mothers who got their first pregnancy in the age group 25-29 years were six times more likely to initiate complementary feeding timely compared to mothers in the age group 15-19 years (AOR=5.82, CI; 2.45, 13.81).
Mothers who attended secondary and above education were four times more likely to start complementary feeding timely compared with mothers who cannot read and write (AOR= 4.18, CI;1.02, 17.20).
It was also observed that the probability of introducing complementary feeding timely decreased by 80% among house wife mothers compared with governmental employed mothers (AOR=0.20, CI; 0.4, 1.18). The study also observed that initiation of complementary feeding timely was lower by 90% among mothers whose partners were daily laborer than governmental employed (AOR=0.10, CI; 0.01, 0.82) (Table 3).
| Variables | Complementary Feeding Timing | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| No | Yes | |||
| Age at first pregnancy | ||||
| 15-19 | 37 | 34 | 1 | 1 |
| 20-24 | 46 | 60 | 1.42(0.78, 2.59) | 2.74(1.26, 5.97)* |
| 25-29 | 33 | 59 | 1.95(1.04, 3.66) | 5.82(2.45, 13.81)* |
| ≥ 30 | 19 | 32 | 1.83(0.88, 3.82) | 3.70(1.38, 9.93)* |
| Maternal education | ||||
| Unable to read and write | 41 | 22 | 1 | 1 |
| Read and write | 39 | 42 | 2.0(1.02, 3.95) | 2.25(0.93, 5.49 |
| Primary education | 50 | 76 | 2.83(1.51, 5.31) | 1.80(0.75, 4.35) |
| Secondary and above | 5 | 45 | 16.77(5.82,48.38) | 4.18(1.02, 17.20)* |
| Paternal education | ||||
| Unable to read and write | 22 | 13 | 0.14(0.59, 0.32) | 3.061(0.68, 13.79) |
| Read and write | 26 | 22 | 0.20().09, 0.42) | 0.88(0.28, 2.79) |
| Primary education | 67 | 64 | 0.22(0.12, 0.40) | 0.96(0.38, 2.42) |
| Secondary and above | 20 | 86 | 1 | 1 |
| Maternal occupation | ||||
| Governmental employed | 12 | 21 | 1 | 1 |
| Housewife | 101 | 127 | 0.09(0.021, 0.39) | 0.20(0.4, 1.18) |
| Daily laborer | 16 | 10 | 0.02(0.003, 0.10) | 0.10(0.01, 0.82)* |
| Merchant | 7 | 25 | 0.027(0.05, 1.39) | 0.49(0.07, 3.51)* |
| Paternal Occupation | ||||
| Governmental employed | 15 | 73 | 1 | 1 |
| Daily laborer | 62 | 11 | 0.02(0.01, 0.05) | 0.01(0.004, 0.05)* |
| Merchant | 58 | 101 | 0.15(0.06, 0.38) | 0.16(0.06, 0.42)* |
| Place of delivery | ||||
| Health Center | 98 | 146 | 4.68(1.93, 11.38) | 2.36(0.67, 8.31) |
| Hospital | 15 | 32 | 6.71(2.35, 19.13) | 2.79(0.66, 11.86) |
| Home | 22 | 7 | 1 | 1 |
Note: P-value of Hosmer and Lemeshow was found to be 0.966 and * indicates the significant factors with complementary feeding timing.
Table 3: Multivariable logistic regression model predicting complementary feeding timing in Halaba Kulito town, Southern Ethiopia, 2016
Discussion
In the present study, it was pointed out that the magnitude of complementary feeding timing was 57.8%. This finding was comparatively lower than WHO recommendation for timely initiation of complementary feeding which is greater than or equal 80% [24]. The magnitude of complementary feeding timing of this study was also lower than the study done in Bangladesh (71%) [25], Sir Lanka (84%) [26] and Nepal (70%) [27]. The difference noticed in this research might be due to low socio-economic status, poor infant and young child feeding practices and low health care access in Ethiopia.
On the other hand, the magnitude of complementary feeding timing was almost similar with the finding in Northern Ethiopia (62.8%) and Eastern Ethiopia (60.5%) [19,28] but higher than the national prevalence (51%) and a finding in Axum; Ethiopia (52.8%) [17,29].
The present magnitude was also better than the findings in West Bengal; India (55.1%), Taiwan (50%), and Nairobi (less than 10%) [30-32]. The higher prevalence in this study probably health extension workers in Ethiopia provide continuous health information dissemination to the community about complementary feeding timing.
It was figured out that complementary feeding timing was higher among mothers who completed secondary education compared with mothers who cannot read and write. This finding is agreed with studies in Ghana, Eastern Ethiopia, Nairobi Kenya, Northern Ethiopia and Tanzania, respectively [16,28,32-34]. This might be explained by the fact that there is no question that educated mothers can provide better care for themselves and for their infants than those with no education. Education also provides better health knowledge, attitude, and practice towards timely introduction of complementary feeding.
The study also revealed that complementary feeding timing was increased among governmental employed mothers and their counterparts/husbands/ compared to daily laborers. This finding was consistent with a study in other areas [16,19,35]. This might be happened since employed women and their partners have ceaseless income and able to provide appropriate commentary feeding to their young infants in timely manner.
It was noticed that timely initiation of complementary feeding was more likely to occur among mothers who got pregnancy in the age group 20-24 and 25-29 years old compared to mothers below age 20 years old. This finding was in line with other studies [16,35]. This could be explained as elder mothers not only own better knowledge of pregnancy and child bearing, ready psychologically and physically but also they have better understanding and experience concerning timely initiation of complementary feeding.
Conclusion
Nearly three among five mothers timely initiated complementary feeding. Women education, creating and promoting income generating activities and health information dissemination strategies, on benefits of avoiding early pregnancy, through mass media and health extension workers need to be considered.
Limitations
When interpreting the findings of this study, scholars need to consider the following limitations. First, the cross sectional nature of the design made unable to arrive at the causal relation between the predictors and timely complementary feeding timing. Second, as the study is based on a sample of children with duration of age 6 to 23 months old, there might be recall bias among mothers. Third, practices of complementary feeding and its frequency were not taken in to account.
Ethical Approval and Consent to Participate
Ethical clearance was obtained from the ethical clearance Institutional Review Board of Hawassa University, College of Medicine and Health Sciences. Permission letter was taken from study area health administrators to conduct the research. For study participants below age 18, informed verbal and written consent was taken from their mothers/care takers after explaining the purpose of the study.
Availability of Data and Materials
All the data (questionnaire and SPSS data) were protected and available in a secured place at Hawassa University; College of Medicine and Health Sciences and can be obtained from the corresponding author upon reasonable request.
Funding
This research work was funded by Hawassa University, College of Medicine and Health Sciences, Ethiopia. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Authors’ Contribution
DTH conceived the study, monitored the data collection process, analyzed the data and wrote the manuscript. DJT, TAA, FBB participated in designing the study, supervising data collection process and writing the manuscript. All authors read and approved the final manuscript.
Acknowledgement
We are thankful to Halaba Kulito town health office for facilitating the data collection process. We would also extend our gratitude to the study subjects without their consent and the provision of the demanded information; this research work would not have been come into existence.
References
- World Health Organization: Complementary Feeding: Summary of Guiding Principles. Report of the Global Consultation, 10–13 December 2001.Geneva, Switzerland: World Health Organization; 2002.
- World Health Organization. Global strategy for infant and young child feeding. Geneva, WHO. 2003.
- World Health Organization. Complementary feeding - Report of the global consultation Summary of Guiding principles Geneva. 2001.
- Aggarwal A, Verma S, Faridi MMA, et al. Complementary feeding reasons for inappropriateness in timing, quantity and consistency. Indian J Pediatr 2008; 75: 49-53.
- Okwori E, Onu R, Onagwa GI, et al. Infant feeding practices and the effect of early complementary feeding on child nutritional status in Makada, Sabon Gari Local Government Area, Kaduna State, Nigeria. Nigerian Journal of Nutritional Sciences 2011: 32.
- Bhutta ZA, Ahmed T, Black RE, et al., Maternal and child under nutrition study group. What works? Interventions for maternal and child under nutrition and survival. Lancet 2008; 371:417-440.
- UNICEF. Infant and young child feeding, nutrition section program. June 2012. New York.
- International Baby Food Action Network (IBFAN). Report On the situation of infant and young child feeding in Liberia. The convention on the rights of the child, session 61, September-October 2012. 2012. Geneva. IBFAN-GIFA.
- WHO, UNICEF. Indicators for Assessing Infant and Young Child Feeding Practices. Part I: Definitions, 2008.
- Pan American Health Organization. Guiding Principles for Complementary Feeding of the Breastfed Child. Geneva, Switzerland: Pan American Health Organization, Washington, DC, USA. WHO. 2003.
- Black RE, Allen LH, Bhutta ZA, et al. Maternal and Child Under nutrition: Global and Regional Exposures and Health Consequences. Lancet 2008; 371: 243-260.
- Alive & thrive. Complementary feeding practices. 2009.
- Liubai L, Sujun L, Ali M, et al. Feeding practice of infants and their correlates in urban areas of Beijing china. Pediatric international 2005; 45: 400-406.
- Dakshayani B, Gangadhar MR. Breast Feeding Practices among the Hakkipikkis: A Tribal population of Mysore district, Karnataka. Ethno-Med 2008; 2: 127-129.
- Rao S, Swathi PM, Unnikrishnan B, et al. complementary feeding practices among mothers of children aged six months to two years in coastal south India. Australasian Med J 2011; 4: 252-257.
- Solomon Sika-Bright. Socio-cultural factors influencing infant feeding practices of mothers attending welfare clinic in Cape Coast. Department of Sociology and Anthropology University of Cape Coast, Ghana. January 2010.
- Central Statistical Agency (Ethiopia) and ICF International 2012. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Agency and ICF International.
- Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF.
- Shumey A, Demissie M, Berhane Y. Timely initiation of complementary feeding and associated factors among children aged 6 to 12 months in Northern Ethiopia: an institution-based cross-sectional study. BMC Public Health 2013, 13:1050.
- Tamiru D, Aragu D, Belachew T. Survey on the introduction of complementary foods to infants within the first six months and associated factors in rural communities of Jimma Arejo. Int J Nutri Food Sci 2013; 2: 77-84.
- Setegn T, Belachew T, Gerbaba M, et al. Factors associated with exclusive breastfeeding practices among m-others in Goba district, South East Ethiopia: A cross-sectional study. Int Breastfeed J 2012.
- Special district health office annual report. 2016.
- Sapkota S, Shrestha S. Complementary Feeding Practices among the Caretakers of the Young Children at Kathmandu. Journal of Chitwan Medical College 2014; 3: 25-29.
- World Health Organization: Infant and young child feeding. A tool for assessing national practices, policies and programs. Geneva 2003.
- Kabir I, Khanam M, Agho KE, et al. Determinants of inappropriate complementary feeding practices in infant and young children in Bangladesh. Secondary data analysis of Demographic Health Survey 2007. Maternal and Child Nutrition 2012; 8: 11-27.
- Senarath U, Godakandage SS, Jayawickrama H, et al. Determinants of inappropriate complementary feeding practices in young children in Sri Lanka. Secondary data analysis of Demographic and Health Survey 2006-2007. Maternal and Child Nutrition 2012; 8: 60-77.
- Joshi N, Agho KE, Dibley MJ, et al. Determinants of inappropriate complementary feeding practices in young children in Nepal. Secondary data analysis of Demographic and Health Survey 2006. Matern Child Nutr 2012; 8: 45-59.
- Agumasie S, Gezahegn T, Alemayehu B. Complementary feeding practices of mothers and associated factors in Hiwot Fana Specialized Hospital, Eastern Ethiopia. Pan African Medical Journal 2014; 18:143.
- Yemane S, Awoke T, Gebreslassie M. Timely initiation of complementary feeding practice and associated factors among mothers of children aged from 6 to 24 months in Axum Town, North Ethiopia. International Journal of Nutrition and Food Sciences 2014; 3: 438-442.
- Sinhababu A, Mukhopadhyay DK, Panja TK, et al. Infant- and young child-feeding practices in Bankura District, West Bengal, India. J Health PopulNutr 2010; 28: 294-299.
- Lin JR, Tzeng MS, Kao MD, et al. Practice to introduce complementary foods to infants in Taiwan – changes from 1997 to2008. Asia Pac J ClinNutr 2011; 20: 337-345.
- Kimani-Murage EW, Madise NJ, Fotso JC, et al. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health 2011; 11: 396.
- Mekbib E, Shumey A, Ferede S, et al. Magnitude and factors associated with appropriate complementary feeding among mothers having children 6-23 months-of-age in Northern Ethiopia; A community-based cross-sectional study. Journal of Food and Nutrition Sciences 2014; 2: 36-42.
- Victor R, Baines SK, Agho KE, et al. Factors associated with inappropriate complementary feeding practices among children aged 6-23 months in Tanzania. Matern Child Nutr 2012; 10: 545-561.
- Ogbo FA, Page A, Idoko J, et al. Trends in complementary feeding indicators in Nigeria, 2003-2013. BMJ Open 2015; 5: e008467.