- Biomedical Research (2014) Volume 25, Issue 2
Comparison of trauma scoring systems for predicting the effectiveness of mortality and morbidity on pediatric patients.
Ali Dur1*, Ertan Sonmez1, Kenan Ahmet Turkdogan1, Cemil Civelek1, Bedia Gulen1, Mehmet Yigit1, Ferudun Koyuncu2, Ozgur Sogut11Bezmialem Vakif University, Department of Emergency Medicine, Istanbul, Turkey
2Beyhekim State Hospital, Emergency Service, Konya, Turkey
- *Corresponding Author:
- Ali DUR
Bezmialem Vakif University
Department of Emergency Medicine
Istanbul, Turkey
Accepted December 17 2013
Abstract
In this study, we aimed to investigate the effectiveness of trauma scoring systems for predicting the sepsis and multiple organ failure in pediatric trauma patients. A total of 330 trauma patients with 112 children and 218 adults admitted to the emergency service of the university hospital which had level 1 trauma center properties between 01.01.2006 and 01.01.2010 were included in the study. Trauma scores such as Injury Severity Score (ISS), New Injury Severity Score (NISS), Glasgow Coma Scale (GCS) and Revised Trauma Score (RTS) were calculated by screening the files and computer records of the patients during clinic visits. The average of ISS, NISS, RTS and GCS scores were statistically significant in pediatric trauma patients in whom mortality was observed than in the patients without mortality observed (p=0.001). The average of ISS, NISS, RTS and GCS scores were statistically significant in adult trauma patients in whom mortality was observed than in the patients without mortality observed (p=0.001). The average of ISS, NISS, RTS and GCS scores were statistically significant in pediatric and adult trauma patients with multi organ failure (MOF) compared to the group without mortality observed (p=0.001). Prediction and accurate triage of the complications play an important role in the management of these trauma patients. In this study, we concluded that physiologic trauma scores could be use for this purpose and were more effective in children.
Keywords
Trauma Scoring System. Sepsis, multiple organ failure, Injury Severity Score), New Injury Severity Score, Glasgow Coma Scale, Revised Trauma Score (RTS)
Introduction
Trauma is a worldwide health problem and the major cause of death and disability, particulary effecting the young population [1]. Despite the measures taken against the traumas, 16.000 people die due to trauma each year, but survival of the cases with severe or multiple trauma have been increasing in conjunction with improvements in the management of health and resuscitation. In patients, the risk of injection and Systemic Inflammatory Response Syndrome (SIRS) were increased depending on the reasons such as degradation of tissue integrity in the period after trauma, hemorrhage, hypoperfusion, decreases in the defense mechanism of the body, the frequent use of blood products and invasive procedures [2].
The complications such as sepsis and multi organ failure (MOF) and problems emerging from these complications are important mortality and socioeconomic problems. Several trauma scoring systems were used to determine the severity of the trauma and to predict the mortality in these cases. These scoring systems were generated as to the physiological and anatomical location or combination of both parameters [3-4].
Some studies suggested that there was a high rate of mortality in trauma patients in rural areas where developed trauma centers are not available and these patients should have been transported appropriately to the primary trauma centers on time [5]. Similar studies also suggested that the mortality has been increased due to insensibility of the trauma severity, delay for starting appropriate resuscitative therapy and not to make required invasive interventios on time.
AIS and ISS are the anatomical scoring systems. AIS is a dictionary which grades trauma from 1 (minor) to 6 (fatal) score. While ISS is calculated, the body allocated into 6 regions (head, neck, face, thorax, abdomen, extremities and other) and the 3 most severely injured body regions have their score squared and added together to produce the ISS score. NISS is calculated as the sum of the squares of the top three AIS scores regardless of the body region.
In this study, type of trauma and trauma scoring systems were investigated in terms of the severity of the trauma, triage of patients during acute phase, requirement for invasive procudures, and predictability of the complications of sepsis and MOF in the late phase.
Material and Methods
Study Design
A total of 330 trauma patients admitted to the emergency service of the university hospital which had level 1 trauma center properties and deemed appropriate of admission to the hospital and emergency intensive care at least 48 hours between 2006 and 2010 were included in this study.
The patients who died in the first 48 hours after trauma or discharged and transferred to the other service or intensive care units and the patients with chronic renal failure, chronic liver disease, congestive heart failure and cancer patients were excluded from the study. Documents and computer records of the patients were analysed in the course of clinic visits and the patients were identified retrospectively for age, sex, mechanism of injury, vital signs, respiratory rate, laboratory findings and concomitant diseases.
Areas of the body affected due to trauma, radiological data, duration of hospital stay, infections at the hospitalization period, organ failures, mechanical ventilation requirement, applied invasive procedures and mortality were investigated. Their trauma scores such as ISS, NISS (New Injury Severity Score), GCS (Glaskow Coma Score) and RTS (Revised Trauma Score) were calculated by screening the files and computer records of the patients during their application to the clinic.
In single traumas ISS score was not excluded, but NISS values were calculated as the sum of the squares of AIS scores at the injuried regions. By using the laboratory and clinic findings of the patients during their follow up, the patients who had SIRS and sepsis criteria during hospitalization were determined according to the definition of 2001 ACCP/SCCM consensus [6].
Patients developed MOF were determined according to criteria of Knaus multi organ failure [7]. From the followup patients with trauma; the group aged 18 and under were determined as pediatric trauma patients and the patients over 18 year of age were determined multiple trauma patients. The effectiveness of trauma scoring systems and the difference between the groups in terms of this effectiveness were investigated.
Statistical Analysis
The statistical analysis of the present study was made by SPSS 15.0 (Chicago, IL) program. Continuous variables are given together with the mean value and standart deviation values. The categorical variables are given together with the number (n) and percentage (%). Pearson’s chi-square and Fisher’s exact test were used for the comparison of the categorical variables between the groups. The ROC analysis was used for the estimates of cut-off related to the variables of ISS, NISS, RTS and GCS. Student t test was used to compare the continuos variables between the groups. In this study, p<0.05 was considered significant.
Results
When the age distribution of the patients included the study was analysed, 112 patients were identified under the age of 18 and 218 patients were identified over the age of 18 as a group of adult. In the pediatric patients group, there were 83(75%) male and 29(25%) female and the median age was found as 8.8 ±5.3 years. In the adult patients group, there were 186 (25.4%) male and 32 (14.6%) female and the median age was found as 40.8±16.5 years.
No statistically significant relationship was found between the MOF and mortality, and between the gender and sepsis for both age groups (p>0.05). When occurence of the traumas were analysed, it’s identified that 105 of the patients for extravehicular accidents, 98 of them for in-vehicle accidents (29.6%) , 56 of them for falls (16.9%) and 35 of them for motorcyle accidents (10.6%), 21 of them for firearm injuries (6.3%) and 15 of them for sharp object injuries (4-5%) were consulted to emergency service.
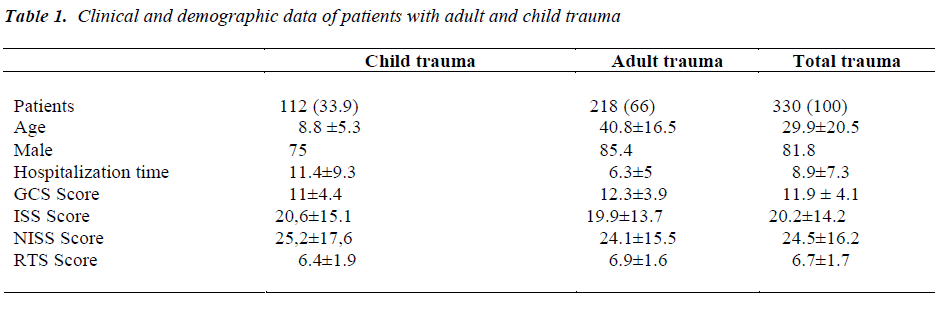
When trauma patients were analyzed according to affected regions; single traumas which had body injury in one body region (no:161) and multiple trauma injuries which had injuries in multiple sites (no:169) were observed to be numerically close to in close proximity to each other. When single and multiple traumas were evaluated together, the most commonly affected areas were identified as head and neck in 220 (66.6%) patients, extremities in 178 (53.9%) patients, thorax in 89(26.9%) patients and abdominal region in 42 (12.7%) patients, respectively. Distribution of the trauma scores in adult and child patients with trauma are shown in the Table 1.
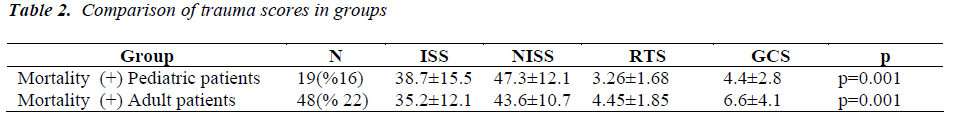
In children and adult trauma patients in whom mortality was observed, the mean ISS, NISS, RTS and GCS scores were statistically significant compared to the group in which mortality was not observed (p:0.001) (Table 2). In children and adult trauma patients in whom MOF was observed, the mean ISS, NISS, RTS and GCS scores were statistically significant compared to the group in which mortality was not observed (p:0.001) (Table 2). When the results were evaluated, it was observed that worsen trauma scores for both adult and child trauma patients increased the rates of mortality and development of MOF (p<0.005).
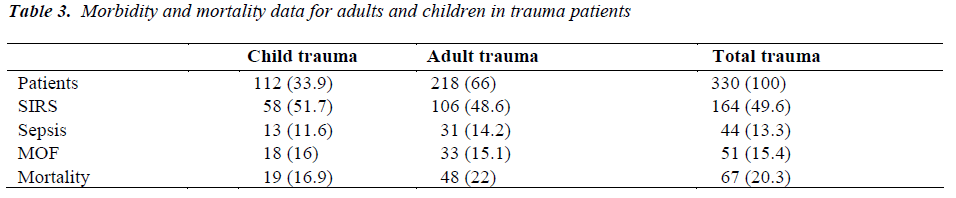
Trauma scores were worser in both pediatric and adult trauma group, therefore MOF, sepsis and mortality rates were found to be increased. Sepsis, MOF and the incidence of mortality in comparison with the child and adult trauma groups were shown in Table 3 and there was no statistically significant difference between both the groups (p<0.05). Mortality rates in children trauma patients developed sepsis and MOF were 38.5% and 44.4%, respectively and the results were found statistically significant in high probability values (p<0.05). However, mortality rates in adult trauma patients developed sepsis and MOF were 38.7% and 57,6%, respectively and the results were found statistically significant in high probability values(p<0.05).
Discussion
Trauma is the most common cause of morbidity and mortality among the young population. The most common cause of early mortality occurs by vital organ injuries and bleeding. MOF and sepsis are the principal causes of late post-traumatic deaths. Because of the unique characteristics of child injuries, it is important that emergency physicians and surgerons must have a broad knowledge base and possess the skills of many specialists for a careful trauma management (8).
In approach to trauma at the acute injury period, basic trauma algorithm are applied as adults. But in some types of traumatic events for children, a higher success rate close to %90 was achieved in the conservative treatment instead of surgery. Because adult body proportions are different from children, the amount of energy per unit area is higher after trauma. Also the bone structures of children are more flexible and less calcific than adults [9]. For this reason, thorax, abdominal organs and spinal cord injures together with minor bone fracture and/or without fracture may be more common in child traumas.
In similar traumas, these differences in children’s body structure may create different organ damage and bone fractures than adults. Therefore, the severity of trauma scores in children was not different compared to adults, and the effectiveness in the prediction of the development of post-traumatic sepsis and MOF was the main topic examined in this study.
In paralel with increase in the innovation for management and resuscitation of trauma patients in the last 50 years, a large number of trauma scoring systems classified as anatomical, physiological and neurological have been developed [10]. Among these scoring systems, GCS, ISS, NISS and RTS are the most frequently used and investigated system for trauma patients [9,10]. However, these studies generally focused on mortality and morbidity in the acute phase, and limited number of studies have been conducted on the the effectiveness in the prediction of the development of sepsis and MOF. Sepsis is rarely seen in children than adults and mortality is 10% lower than in adults [11]. In addition, a high incidence of multiorgan failure have been reported in intensive care patients after sepsis [12]. In our study, GCS, ISS, NISS and RTS were observed as a sufficent parameter alone for both adult and child traumas in predicting mortality and duration of hospital stay.
GCS and RTS scores of the pediatric patients were lower and found statistically more significant compared to the adult patients. The reason of this difference could be due to the higher values of the respiratory rate among the parameters used in the calculation of RTS and the lower levels of arterial blood pressure in children. However, it was shown that the vital signs were more deterioted after trauma and trauma severity was more severe in children.
In the present study, the incidence of sepsis was found to be slightly lower in children traumas. A statistical significance difference was found between the GCS, ISS, NISS and RTS scores and the development of sepsis and MOF in both adult and children patients. The results obtained from this study showed that the scores of RTS and GCS of pediatric trauma patients developed sepsis were lower than adult patients developed sepsis. No statistical significance difference was found between pediatric and adult patients developed sepsis in terms of the ISS and NISS scores. In a study of 450 cases with regard to the incidence of sepsis after trauma, the development rate of sepsis was found as 14.4% and the mortality rate in trauma patients developed sepsis was higher [13]. We found that the sepsis incidence in our study was similar to the study which was not classified the trauma patients as adult or child.
In another study investigating sepsis in trauma patients, incidence of sepsis has been found as 2% and in that study, sepsis was increased the mortality [14]. Because the patients who were discharged from the first two days were not excluded from this study, rate of sepsis might have been found a relatively lower. In the same study, the RTS and ISS scores were significantly correlated with the development of sepsis in trauma patients [14]. Our results were compatible with this study and additionally, GCS and NISS scores were also shown to be effective in predicting the development of sepsis. In recent studies, MOF has developed in 5% to 25% trauma patients at the intensive care units, and it was suggested that mortality of these patients was increased by six-fold [15]. In the present study, the GCS, ISS, NISS and RTS scores were observed to be effective for predicting MOF in child and adult trauma patients similar to sepsis.
When the trauma patients developed MOF were compared, RTS and GCS scores of children were found in a stronger relation than in adults. As in sepsis, no significance difference was found between children and adult patients developed MOF in terms of ISS and NISS scores. In child traumas, the rate of MOF was found in similar rates with adults and significantly increased the mortality rate in both groups.
In conclusion, the physiological trauma scoring systems for predicting sepsis and MOF in children’s trauma were found to be more effective, but the anatomical trauma scoring systems were found to be equally effective in both groups. To decide whether pediatric trauma patients are more resistant against complications such as sepsis and MOF then adults, there is a need to study large number of children trauma patients.
Acknowledgements
The authors would like to thank to the Refik Saydam Hygiene Center of Ankara, Turkey for testing the serum samples, and our colleagues from the Turkish Ministry of Health for their contributions.
Conflict of interest
No conflict of interest and no funding source to declare.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki for Human Research, and was approved by the institutional ethics committee.
References
- Krug EG, Sharma GK, Lozano R. The Global Burden of Injuries. Am J Public Health 2000; 90: 523-526.
- Xu YX, Ayala A, Chaudry IH. Prolonged immuno- depression after trauma and hemorrhagic shock. J Trauma 1998; 44: 335- 341.
- Butcher N, Balogh ZJ. The definition of polytrauma: the need for international consensus. Injury 2009; 40 Suppl 4: S12-22.
- Veenema KR, Rodewald LE. Stabilization of rural multiple-trauma patients at level III emergency departments before transfer to a level I regional trauma center. Ann Emerg Med 1995; 25: 175-181.
- Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003; 31: 1250-1256.
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. Prognosis in acute organ-system failure. Ann Surg 1985; 202: 685-693.
- Guice KS, Cassidy LD, Oldham KT. Traumatic injury and children: a national assessment. J Trauma 2007; 63(6 Suppl): S68-80; discussion S81-86.
- Avarello JT, Cantor RM. Pediatric major trauma: an approach to evaluation and management. Emerg Med Clin North Am 2007; 25: 803-836.
- Chawda MN, Hildebrand F, Pape HC, Giannoudis PV. Predicting outcome after multiple trauma: which scoring system? Injury 2004; 35: 347-358.
- Angus DC, Linde-Zwirble WT, Lidicker JM et al.Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29: 1303-1310.
- Martin GS, Mannino DM, Eaton S et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003; 348: 1546-1554.
- Muckart DJ, Bhagwanjee S: American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med 1997; 25: 1789-1795.
- Osborn TM, Tracy JK, Dunne JR, Pasquale M, Napolitano LM. Epidemiology of sepsis in patients with traumatic injury. Crit Care Med 2004; 32: 2234-2240.
- Ulvik A, Kvale R, Wentzel-Larsen T, Flaatten H: Multiple organ failure after trauma affects even long- term survival and functional status. Crit Care 2007; 11: R95.
- Durham RM, Moran JJ, Mazuski JE, Shapiro MJ, Baue AE, Flint LM. Multiple organ failure in trauma patients. J Trauma 2003; 55: 608-616.