- Biomedical Research (2014) Volume 25, Issue 4
Comparison of 25-hydroxy vitamin D3, adiponectin and apolipoprotein A5 levels in subjects with different glucose tolerance and their correlation with blood lipid.
Yan Yang1, Lin Gao1*, De-Jing Wang2, Fu-Rong Li3, Yong-Hui Yan1, Xiao-Ying Wang1, Xin Liao1, Qi Huang1, Han Zhang1, Qi-Rong Chen1, Qian Wang1, Yue Weng1 and Mei-Hui Song11Department of Endocrinology, Affiliated Hospital of Zunyi Medical College, Zunyi 563099, Guizhou, China
2Reproductive Center, Affiliated Hospital of Zunyi Medical College, Zunyi 563000, Guizhou, China
3Department of Immunology, Zunyi Medical College, Zunyi 563000, Guizhou, China
- *Corresponding Author:
- Lin Gao
Department of Endocrinology
Affiliated Hospital of Zunyi Medical College
Zunyi 563099, Guizhou, China
Accepted date: July 17 2014
Abstract
This study aims to compare 25-hydroxy vitamin D3 (25(OH)D3), adiponectin (ADPN) and apolipoprotein A5 (apoA5) levels among subjects with different glucose tolerance and to explore their correlation with lipid metabolism. Subjects were divided into 98 cases of type 2 diabetes mellitus (T2DM group), 87 cases of impaired glucose regulation (IGR group) and 100 cases of normal glucose tolerance (NGT group). 25(OH)D3, adiponectin (ADPN), apolipoprotein A5 (apoA5), hemoglobin A1c (HbA1c) and blood lipid were estimated and analyzed. It was found that the levels of 25(OH)D3, ADPN, apoA5 and high-density lipoprotein cholesterol (HDL-C) in T2DM and IGR groups were lower than that of NGT group, while HbA1c, total cholesterol (TC), triacylglycerol (TG) and LDL-C levels were higher than that of NGT group (P<0.05). Levels of 25(OH)D3, ADPN, apoA5 and HDL-C in T2DM group were lower than that of IGR group. However, HbA1c, TC, TG and LDL-C levels were higher than that of IGR group (P<0.05). Therefore, low plasma levels of 25(OH)D3, ADPN and apoA5 may possibly be the risk factors for impaired glucose tolerance, thus the regulation of 25(OH)D3, ADPN, and apoA5 concentrations could be important in the prevention of dyslipidemia and T2DM.
Keywords
Impaired glucose regulation; 25-hydroxy vitamin D3; Adiponectin; Apolipoprotein A5; Blood lipid
Introduction
Lipotoxicity is one of the important factors for decreased number of pancreatic β-cells and insulin resistance (IR) from normal glucose tolerance (NGT) to impaired glucose tolerance (IGT) and type 2 diabetes mellitus (T2DM), thus diabetes is also known as glycolipid disease that emphasizes the importance of lipotoxicity in the development of T2DM [1]. It has been shown that plasma 25-hydroxy vitamin D 3(25(OH)D3) level can predict hyperglycemia and insulin resistance (IR) [2]. 25(OH)D3 has been extensively focused in the diabetes development process; the researches about the Since correlation among 25(OH)D3, adiponectin (ADPN), apolipoprotein A5 (apoA5) and blood lipid has not yet been reported, we aimed to explore whether there is any correlation among 25(OH)D3, ADPN, apoA5 and blood lipid among people with NGT, IGR, or T2DM. Which might provide important guidance in the prevention and treatment of IGT, T2DM and dyslipidemia.
Materials and Methods
Subjects
Between Jan. 2011 and Nov. 2011, we recruited 306 outpatients from Chongqing Medical University, of which 108 patients (53 males and 55 females) with newly diagnosed T2DM aged (55.6 ± 9.7) years, 97 patients with IGR who were subdivided into 48 IGT patients (24 males and 24 females) aged (53.7 ± 9.2) years and 49 IFG patients (23 males and 26 females) aged (54.2 ± 9.1) years and 101 subjects with NGT (52 males and 49 females) aged (53.5 ± 9.2) years. Patients were subjected to oral glucose tolerance test (OGTT). This study was conducted in accordance with the declaration of Helsinki and with approval from the Ethics Committee of Zunyi Medical College. Written informed consent was obtained from all participants.
Inclusion and exclusion criteria
Inclusion criteria for T2DM: i) newly diagnosed T2DM according to 1999 World Health Organization (WHO) diagnostic criteria; ii) normal hepatorenal function without severe organic disease or acute diabetic complications; iii) no pregnancy or lactation; iv) no previous diabetes treatment including diet and exercise therapy. Inclusion criteria for IGR: patients consistent with 2010 ADA diagnostic criteria, including people with NGT confirmed by OGTT (fasting plasma glucose (FPG) <5.6 mmol/l and 2hPG <7.8 mmol/l); IGT (FPG <5.6 mmol/l and 7.8 mmol/l ≤2hPG <11.1 mmol/l); IFG (5.6mmol/l ≤FPG <7.0 mmol/l and 2hPG <7.8 mmol/l). No medications on the day of test.
Exclusion criteria
Heart, liver or kidney disease or endocrine disease; administrated the drugs that may influence the glucose or lipid metabolism within one month; history of any inflammation two weeks before the examination.
Detection methods
Access to food and water were restricted 12 h and 8 h, respectively before experiment. Fasting venous blood sample was drawn to measure blood lipid and glucose. OGTT was performed in the morning by orally taking glucose solution (75 g of anhydrous dextrose in 300 ml of water) within 5 min while fasting.
Electrochemiluminescence was used to detect 25(OH) D3 (Kit was from Roche Diagnostics GmbH,NY, USA); plasma ADPN was determined with ELISA Kit from US R&D with sensitivity of 100 pg/ml and measurement range of 100 pg/ml-6 ng/ml; plasma apoA5 was measured with ELISA Kit from US Phoenix Pharmaceuticals, Inc., with sensitivity of 0.85 pg/ml and measurement range of 0.85 pg/ml-61.5 ng/ml, and the inter- and intra-batch variations were ±5.2% (7.4 ng/ml) and ±15.0% (6.7 ng/ml). High performance liquid chromatography (HPLC) was employed to detect HbA1c (the kit was purchased from Beckman coulter Co., Ltd., USa); high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C) were measured with direct method; chemiluminescence was performed to determine fasting insulin (FINS) level; total cholesterol (TC) and triacylglycerol (TG) were detected with enzyme (Kit was from Roche Diagnostics GmbH, NY , USA); FPG was measured with oxidase assay; insulin resistance index (IRI) = FPG × FINS/22.5.
Statistical analysis
Data was analyzed with SPSS16.0 and presented as
( ± s ). Comparison between groups utilized variance
analysis and t-test. Multiple factors were analyzed using stepwise multiple regressions. P < 0.05 was considered
statistically significant.
± s ). Comparison between groups utilized variance
analysis and t-test. Multiple factors were analyzed using stepwise multiple regressions. P < 0.05 was considered
statistically significant.
Results
General data - HbA1c and blood lipid
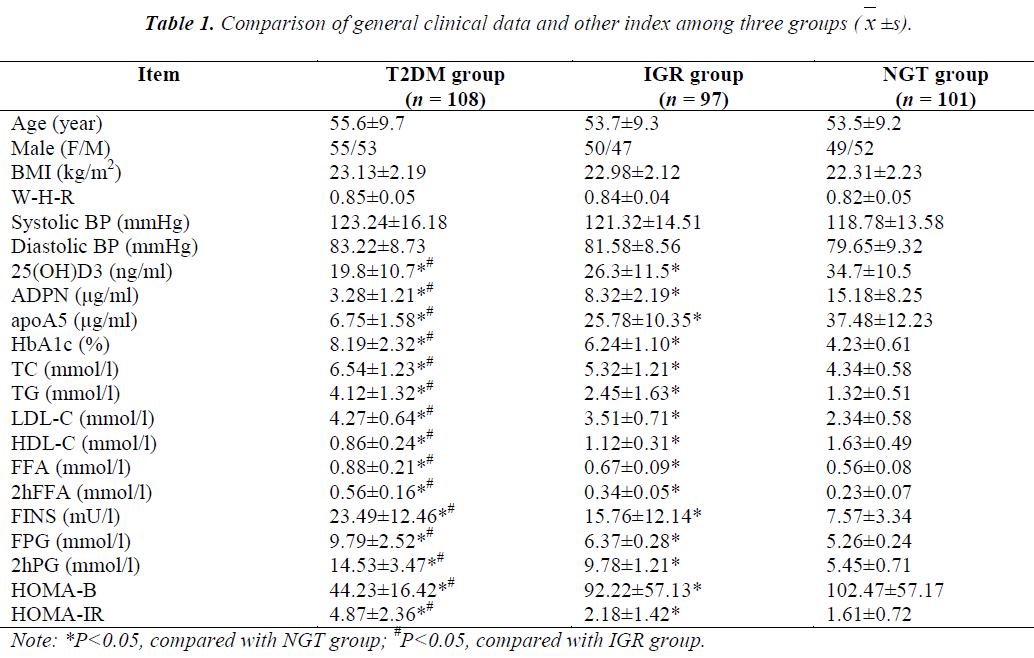
There were no statistical differences in age, gender, body mass index (BMI), waist-to-hip ratio (WHR), systolic and diastolic blood pressure (SBP and DBP) among three groups (P>0.05) so far tested. The differences in 25(OH)D3, ADPN, apoA5, HbA1c, TC, TG, LDL-C, HDL-C, free fatty acid (FFA), 2 h OGTT FFA (2hFFA), FINS, FPG, 2hPG, homeostatic model assessment of β-cell function and IR (HOMA-B and HOMA-IR) were significant (P<0.05). In T2DM and IGR groups, levels of 25(OH)D3, ADPN, apoA5, HDL-C and HOMA-B were lower than that of NGT group, while HbA1c, TC, TG, LDL-C, FFA, 2hFFA, FINS, FPG, 2hPG and HOMA-IR levels were higher than that of NGT group (P<0.05). Levels of 25(OH)D3, ADPN, apoA5, HDL-C and HOMA-B in T2DM group were found to be lower than that of IGR group; HbA1c, TC, TG, LDL-C, FFA, 2hFFA, FINS, FPG, 2hPG and HOMA-IR levels were higher than that of IGR group (P<0.05, Table 1).
Multiple regression analysis
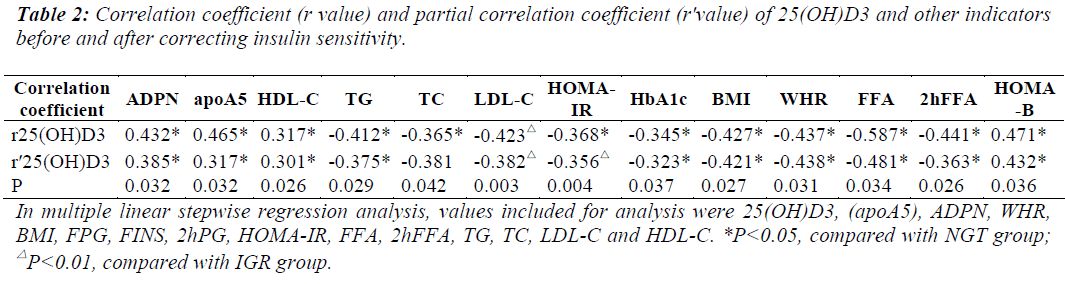
Pearson correlation analysis indicated that 25(OH)D3 did not correlate with gender, age and blood pressure (P>0.05), positively correlated with serum levels of ADPN, apoA5, HOMA-B and HDL-C (correlation coefficient r was 0.432, 0.465, 0.447 and 0.317, P<0.05) and negatively correlated with HbA1c, HOMA-IR, BMI, WHR, TC, TG, LDL-C, FFA, 2hFFA (correlation coefficient r was -0.345, -0.368, -0.427, -0.437, -0.365, - 0.412, -0.423, -0.587 and -0.441, P<0.05). Stepwise multiple regression analysis, with 25(OH)D3 as dependent variable and ADPN, apoA5, HbA1c, HOMA-IR, BMI, WHR, TC, TG, LDL-C, HOMA-B, HDL-C, FFA, 2hFFA as independent variables, showed the independent influencing factors of 25(OH)D3 were ADPN, apoA5, HbA1c, TG, WHR and HOMA-IR (β = 0.534, 0.621, -0.472, -0.526, -0.465, -0.375; P<0.05). After correction of insulin sensitivity, 25(OH)D3 still negatively correlated with HbA1c, HOMA-IR, BMI, WHR, TC, TG, LDL-C, FFA, 2hFFA (correlation coefficient r was -0.323, -0.356, -0.421, -0.438, -0.381, -0.375, - 0.382, -0.481, -0.363, P<0.05) and positively correlated with serum levels of ADPN, apoA5, HOMA-B, HDL-C (correlation coefficient r was 0.385, 0.317, 0.432, 0.301, P<0.05). Stepwise multiple regression analysis displayed the independent influencing factors of 25(OH)D3 were TG, HbA1c, ADPN, apoA5, WHR, HOMA-IR (β = - 0.531, -0.352, 0.576, 0.457, -0.334, -0.268; P<0.05). The multiple regression equation was as follows: Y25(OH)D3 = 71.462 - 25.231XTG - 32.421XHbA1c + 33.543XADPN + 35.524XapoA5 - 36.472 XWHR - 38.467XHOMA-IR (Table 2).
Discussion
WHO has predicted that there will be 46 million Chinese diabetic patients in 2025, ranking the second in the world. Chinese Diabetes Society believes that attention to IGR risk group is required to prevent this trend. Many studies have demonstrated that blood concentration of 25(OH)D3 is correlated with T2DM morbidity [3-5] and people with vitamin D deficiency are more susceptible to metabolic syndrome and diabetes [6-8]. In 2001, 1ipotoxicity was reported as primary pathophysiologic factor for diabetes and milestone in research on pathogenesis of diabetes [9]. Dyslipidemia is important in T2DM development as it damages the function of mitochondria in muscle and disturbs the role of insulin in glucose metabolism, resulting in glucose metabolism disorder [10,11]. In NGT-IGRT2DM development, glucotoxicity and lipotoxicity are reciprocal causation and contribute to the occurrence and development of diabetes. However, the relationship among levels of 25(OH)D3, ADPN, apoA5 and blood lipid is rarely reported.
Norman et al [12] have discovered that the pancreatic islets from rats with vitamin D deficiency display decreased insulin synthesis and secretion stimulated by glucose and arginine. Research has shown a significant lower level of vitamin D in patients with T2DM than that of healthy controls [13] and a close correlation between reduction of plasma 25(OH)D3 level, IR, obesity and T2DM [14-17]. The above results were consistent with the results of this study。ADPN mainly regulates glucose and lipid metabolism, increases fatty acid oxidation and isulin sensitivity and correlates with obesity, IR and diabetes [18], and protects pancreatic β-cells. Recent research [19,20] has revealed that plasma apoA5 level negatively correlates with TG, BMI, HOMA-IR and low plasma level of apoA5 is involved in IR-related hypertriglyceridemia. Vaessen et al [21] have reported that overexpression of apoA5 decreases plasma TG level, apoA5 deficiency, increase in TG level in human and murine and apoA5 negatively correlates with TG level. In our study, plasma levels of 25(OH)D3, ADPN and apoA5 gradually decreased and HbA1c, TC, TG, LDL-C levels were gradually increased in NGT-IGR-T2DM development; 25(OH)D3 concentration was positively correlated with serum levels of ADPN, apoA5, HOMAB, HDL-C and negatively correlated with HbA1c, HOMA-IR, BMI, WHR, TC, TG and LDL-C; the independent influencing factors of 25(OH)D3 were ADPN, apoA5, HbA1c, TG, WHR and HOMA-IR. Levels of HbA1c, TC, TG and LDL-C in T2DM group were significantly higher than that of IGR and NGT groups, while 25(OH)D3, ADPN, apoA5 and HDL-C levels were distinctly lower than that of IGR and NGT groups. Therefore, we speculate that 25(OH)D3, ADPN and apoA5 could be early indicators for dyslipidemia at increasing risk for diabetes; decrease in plasma levels of 25(OH)D3, ADPN and apoA5 probably act as high risk factors for IGT.
In conclusion, IGT severity closely correlates with the levels of 25(OH)D3, ADPN, apoA5, HbA1c and dyslipidemia. Reduced plasma level of 25(OH)D3 might cause decrease in ADPN, apoA5 levels and dyslipidemia. Conversely, dyslipidemia decreases plasma 25(OH)D3, ADPN and apoA5 levels and increases HbA1c level to form a vicious circle, thus 25(OH)D3, ADPN, apoA5 levels, glucose and lipid metabolism disorders are reciprocal causation and collectively contribute to the occurrence and development of IGR, T2DM and dyslipidemia. Therefore, maintenance of 25(OH)D3, ADPN and apoA5 levels at control values could essentially prevent IGR and T2DM development. However, further studies are required to explore the underlying mechanism.
Acknowledgements
This study was supported by Guizhou Provincial Science and Technology Project {No: Qiankehe [2013] 19}; Starting Fund of Dcotor of Zunyi Medical College, ([2012] F- 574); Scientific Research Starting Fund of young people, Affiliated Hospital of Zunyi Medical College [Yuanzi (2010) 3; Outstanding Scientific and Educational Personnel Special Funds of Guizhou Provincial Governor (Qianshengzhuanhezi (2008) No. 110); Guizhou Provincial Science and Technology Cooperation Project (Qiankehequyuhe [2010] No. 7004).
References
- Klop B, Elte JW, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients 2013; 5: 1218-1240.
- Forouhi NG, Luan J, Cooper A, et al. Baseline serum 25-hydroxy vitamin d is predictive of future glycemic status and insulin resistance: the Medical Research Council Ely Prospective Study 1990-2000. Diabetes 2008; 57: 2619-2625.
- Yin Y, Yu Z, Xia M, et al. Vitamin D attenuates high fat diet-induced hepatic steatosis in rats by modulating lipid metabolism. Eur J Clin Invest 2012; 42: 1189-1196.
- Lebrun V, Molendi-Coste O, Lanthier N, et al. Impact of PPAR-α induction on glucose homoeostasis in alcohol-fed mice. Clin Sci (Lond) 2013; 125: 501-511.
- Kostoglou-Athanassiou I, Athanassiou P, Gkountouvas A, Kaldrymides P. Vitamin D and glycemic control in diabetes mellitus type 2. Ther Adv Endocrinol Metab 2013; 4: 122-128.
- Ford ES, Ajani UA, McGuire LC, Liu S. Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care 2005; 28: 1228-1230.
- Nwosu BU, Stavre ZG, Maranda L, et al. Hepatic dysfunction is associated with vitamin D deficiency and poor glycemic control in diabetes mellitus. J Pediatr Endocrinol Metab 2012; 25: 181-186.
- Poel YH, Hummel P, Lips P, et al. Vitamin D and gestational diabetes:a systematic review and meta-analysis. Eur J Inter Med 2012; 23: 465-469.
- Moon YA, Liang G, Xie X, et al. The Scap/SREBP pathway is essential for developing diabetic fatty liver and carbohydrate-induced hypertriglyceridemia in animals. Cell Metab 2012; 15: 240-246.
- Hirabara SM, Curi R, Maechler P. Saturated fatty acidinduced insulin resistance is associated with mitochondrial dysfunction in skeletal muscle cells. J Cell Physiol 2010; 222: 187-194.
- Feher M, Greener M, Munro N. Persistent hypertriglyceridemia in statin-treated patients with type 2 diabetes mellitus. Diabetes Metab Syndr Obes 2013; 6: 11-15.
- Norman AW, Frankel JB, Heldt AM, Grodsky GM. Vitamin D deficiency inhibits pancreatic secretion of insulin. Science 1980; 209: 823-825.
- Kostoglou-Athanassiou I, Athanassiou P, Gkountouvas A, Kaldrymides P. Vitamin D and glycemic control in diabetes mellitus type 2. Ther Adv Endocrinol Metab 2013; 4: 122-128.
- Cimbek A, Gürsoy G, Kirnap NG, et al. Relation of obesity with serum 25 hydroxy vitamin D3 levels in type 2 diabetic patients. J Res Med Sci 2012; 17: 1119-1123.
- Gandhe MB, Jain K, Gandhe SM. Evaluation of 25(OH) Vitamin D3 with Reference to Magnesium Status and Insulin Resistance in T2DM. J Clin Diagn Res 2013; 7: 2438-2441.
- Jorde R, Grimnes G. Vitamin D and metabolic health with special reference to the effect of vitamin D on serum lipids. Prog Lipid Res 2011; 50: 303-312.
- Al-Timimi DJ, Ali AF. Serum 25(OH) D in Diabetes Mellitus Type 2: Relation to Glycaemic Control. J Clin Diaqn Res 2013; 7: 2686-2688.
- Skrabal CA, Czaja J, Honz K, et al. Adiponectin-its potential to predict and prevent coronary artery disease. Thorac Cardiovasc Surg 2011; 59: 201-206.
- Huang XS, Zhao SP, Hu M, et al. Decreased apolipoprotein A5 is implicated in insulin resistance-related hypertriglyceridemia in obesity. Atherosclerosis 2010; 210: 563-568.
- Ramakrishnan L, Sachdev HS, Sharma M, et al. Relationship of APOA5, PPARγ and HL gene variants with serial changes in childhood body mass index and coronary artery disease risk factors in young adulthood. Lipids Health Dis 2011; 10: 68.
- Vaessen SF, Dallinga-Thie GM, Ross CJ, et al. Plasma apolipoprotein AV levels in mice are positively associated with plasma triglyceride levels. J Lipid Res 2009; 50: 880-884.