Research Article - Biomedical Research (2017) Volume 28, Issue 12
Comparative study of endoscopic thyroidectomy via a breast approach versus conventional open thyroidectomy in papillary thyroid microcarcinoma patients
Xiaoting Ren1#, Zhenzhen Dai2#, Hongcun Sha3, Jiayan Wu1, Xiaoming Hong3* and Zili Xiu4*
1Medical School of Ningbo University, Zhejiang, PR China
2Department of Pathology, Ningbo Yinzhou People’s Hospital, Zhejiang, PR China
3Department of General Surgery, Ningbo Yinzhou No.2 Hospital, Zhejiang, PR China
4Department of Medical Matters, Ningbo Yinzhou No.2 Hospital, Zhejiang, PR China
#These authors contributed equally to this work
- *Corresponding Authors:
- Xiaoming Hong
Department of General Surgery
Ningbo Yinzhou NO.2 Hospital
PR China - Zili Xiu
Department of Medical Matters
Ningbo Yinzhou No.2 Hospital
PR China
Accepted date: April 21, 2017
Abstract
Background: Thyroid Carcinoma (TC) was the most frequent endocrine system malignant tumor with steadily increasing incidence in the past period of time, especially in young women. The cosmetic result of Endoscopic Thyroid surgery (ET) is superior to conventional Open Thyroid surgery (OT). Evaluation and comparison of the surgical results of ET via a Breast Approach (ETBA) and OT had been made in this study to investigate the usefulness of ETBA in Papillary Thyroid Microcarcinoma (PTMC) in lowrisk female patients.
Methods: From June 2015 to June 2016, a total of 55 female patients who have be proved to have PTMC were enrolled and allocated into two groups on the basis of the different methods of the operation, 20 patients experienced ETBA, 35 patients underwent OT. Many variances were analysed between two groups respectively.
Results: According to the comparison analysis for such as outcomes of perioperative period, postoperative complications, pain after surgery and cosmetic outcomes, the results showed that not only improve cosmetic effect, ETBA go through less pain and dose not add risk of postoperative complications.
Conclusion: ETBA was found to be similar to conventional OT in terms of early surgical outcomes, however, patients could get more satisfactory cosmetic effect without obvious scar in the neck. ETBA can be viewed as an acceptable alternative method in low-risk PTMC in female patients.
Keywords
Endoscopic thyroidectomy via a breast approach, Conventional open thyroidectomy, Papillary thyroid microcarcinoma
Introduction
TC accounts for 5% of thyroid nodules [1], but is the most common malignancies in endocrine system. With a wide range applications of Ultrasonography (US) and ultrasound-guided Fine Needle Aspiration Cytology (FNAC), PTMC had been detected more frequently [2]. According to Lee [3], the thyroid gland is the fourth most common cancer site among females and PTC is 11 times more common in women than in men. The incidence of thyroid carcinoma showed a continued increase during recent years [4].
As we all know, the main treatment for TC is surgical resection now [5]. Excision of the thyroid through a skin crease incision in the anterior neck provides good direct exposure to facilitate safe dissection and a quick operation with low morbidity and minimal mortality [6]. It results in a cervical collar incision on the neck and leaves an obvious scar that compromises a patient's cosmetic appearance [7,8]. As Kim [9] argued that this incision will cause hypaesthesia or paraesthesia. This view was supported by Woo [10] who wrote keloids influence patients’ quality of life. Easily visible neck scars postoperation is an intolerable sequela for some female patients, especially for young women with keloids.
TC has been considered a disease with excellent prognosis. The overall survival rate has remained at 90% to 95% in recent decades [11]. Moreover, TC can remain in the home position and symptomless for long time with the overall survival not be affected. At this time, patients not only pay attention to the cure of the disease, but also to the quality of life after surgery [12]. Therefore, the demand for operation method which will reduce or hidden surgical incision while maintaining best physiological functions and ideal aesthetic effects was increasing.
Rapid development of endoscopic techniques and instruments (such as the technique known as minimally invasive surgery and ultrasonic scalpels) [13] has enabled doctors to perform thyroidectomy with a smaller incision or incision placement at hidden sites away from the neck, resulting in nonevident scars [14]. Each endoscopic approach has distinct merit and drawbacks with regard to the exposure of the surgical field, instrumentation, learning curve to competency, and preservation of critical structures [15]. Although many reports on surgical results of ETBA have appeared, rare prospective study comparing the results of ETBA and OT has been described. We therefore designed a prospective trial to compare the operation outcomes.
Materials and Methods
Patients
Between June 2015 and June 2016, we selected a total of 55 patients with thyroid nodules. The inclusion criteria were as follows: (1) female patients younger than 45 years old; (2) Papillary Thyroid Carcinoma (PTC) of less than 1 cm in tumor size; (3) no definite evidence of local invasion; (4) no evidence of metastatic lymph nodes; (5) no adhesion or fixation of enlarged lymph nodes around the neck compartment.
US and Computed Tomography (CT) scans of the neck were performed before the surgery and FNAC was not routinely performed. All patients underwent preoperative direct laryngoscopy to assess vocal cord motility. The diagnosis of PTMC was confirmed by means of intraoperative frozen section. Finally, enrolled in this study were 20 patients who underwent ETBA were assigned to the endoscopic group and 35 who underwent OT were assigned to the conventional open group.
All patients who were diagnosed as PTMC during operation were experienced thyroid lobectomy with central lymph node dissection. All operations were conducted by a same team of surgeon and carried out after giving informed consent concerning the surgical risks. All patients in ETBA group provided the possibility of conversion to OT.
Methods
Whether ETBA or OT, the preparation of the patient was the same. The patient was placed in a supine position, after general anaesthesia and endotracheal intubation, a pillow was placed beneath the shoulder to extend the head.
OT: Like all traditional open thyroidectomy, a 6-8 cm transverse collar skin incision was made in the middle of the anterior neck 2 cm above the sternal notch, and the lower layer of the platysma was exposed under direct vision. Platysma myocutancous flap dissection was performed to achieve adequate working space from the sternal notch to the level of the thyroid cartilage and to the medial edge of each of the sternocleidomastoid muscles laterally. The midline of the strap muscles was divided vertically, and the thyroid gland was exposed. The wounds were closed with absorbable suture material by a continuous subcutis suture method [16].
ETBA: Total endoscopic thyroidectomy differs greatly from the conventional approaches in that it requires creation of a subcutaneous working space [17]. Ohgami et al. [18] are the first to perform ETBA. They are to be congratulated for their bold attempts at approaching the neck via remote portals: ports are placed in the areola margin of both breasts and in the right parasternal region between the nipples.
We referred to the practice of predecessors [9,14]. A skin incision 1.2 cm in length was made in the right parasternal region at the nipple level. Then the subcutaneous tissue of the anterior chest wall was dissected bluntly through the incision and a 10-mm trocar for endoscopy was inserted. Carbon dioxide gas at a pressure of 6-8 mmHg to inflate the working space. Two 5 mm trocars for the operator were inserted into the upper margin of bilateral areolas. The working space was made widely to the hyoid bone level superiorly, and both the medial side of the anterior border of the sternocleidomastoid muscle laterally with the visual guidance of the endoscope. The space between the ‘‘red’’ platysma or ‘‘yellow’’ fatty tissue and the ‘‘white’’ aponeurosis were the guides to establishing the right plane of dissection [19].
An aspiration drainage tube was placed in thyroid bed through the edge of the separate skin incision in OT and the left mammary areola in ETBA before concluding the operation. All patients were followed up for at least 6 months after surgery.
Statistical analyses
Data was analysed using SPSS version 18.0. Continuous data were compared using t-tests, and categorical data were analysed using chi-square tests. All data are expressed as mean ± SD, proportions or numbers. A P-value<0.05 was considered statistically significant.
Surgical outcome assessment
The following variables, including perioperative parameters (operation time, intraoperative bleeding, amount of drainage, duration of drainage, duration of hospital stay), postoperative complications (transient and permanent hypocalcemia, transient and permanent recurrent laryngeal nerve palsy, hematoma), pain for the neck or anterior chest wall and cosmetic results were compared between the groups.
Body mass index (BMI): One’s weight in kilograms divided by the square of one’s height in meters. Operation time was defined as the time interval between skin incision and closure. The aspiration drainage tube was removed when volume of drainage became less than 30 ml a day after surgery. Amount of drainage was calculated after the operation to the drain was removed. Hypocalcemia was defined as a serum total calcium level less than 8 mg/dL with hypocalcemic symptoms during the hospitalization. Vocal cord palsy, documented by direct laryngoscopy for all patients with hoarseness after surgery. When hypocalcemia and vocal cord palsy lasting more than 6 months after surgery and there was no evidence of recovery was regarded as permanent. All patients were asked to grade their satisfaction with the cosmetic results and postoperative pain in the neck or anterior chest wall.
Results
There was no case of conversion to OT during the ETBA.
Surgery-related outcomes are presented in Table 1. We choose female patients less than 45 years old, the age distribution of the groups was similar (P=0.997). BMI in two groups was not statistically significant (20.65 ± 0.723 vs. 20.75 ± 0.704, P=0.595). The operation time of open group was shorter than endoscopic group, which was statistically significant (P=0.003). The intraoperative bleeding in two groups was not statistically significant (P=0.792). The volume and duration of postoperative drainage were different between the two groups, these differences were statistically significant (P=3.406 × 10-4 and 1.091 × 10-8, respectively). The duration of hospital stay was also similar between the two groups, which was not statistically significant (P=0.11).
| Endo group (20) | Open group (35) | P-Value | |
|---|---|---|---|
| Age (years) | 36.05 ± 7.536 | 36.06 ± 5.646 | 0.997 |
| BMI | 20.65 ± 0.723 | 20.75 ± 0.704 | 0.595 |
| Operation time (min) | 169 ± 56.489 | 127.74 ± 42.051 | 0.003 |
| Intraoperative bleeding (ml) | 24.25 ± 17.265 | 21.14 ± 13.178 | 0.792 |
| Amount of drainage (ml) | 210.85 ± 19.366 | 93.17 ± 49.113 | 3.406 × 10-4 |
| Duration of drainage (days) | 4.95 ± 1.234 | 2.63 ± 0.490 | 1.091 × 10-8 |
| Duration of hospital stay (days) | 8.65 ± 0.671 | 8.20 ± 0.759 | 0.11 |
| Endo: Endoscopic. | |||
Table 1: Surgery-related outcomes of endoscopic group and open group.
The postoperative complications are listed in Table 2. Two (10%) in endoscopic group and nine (25.7%) in open group experienced a serum total calcium level less than 8 mg/dL or had a symptom of numbness of extremities, which was not statistically significant (P=0.293). The number of patients who experienced voice hoarse were two (10%) and four (11.4%), and P=1.000. Each group has one (5% and 2.9%) occurred hematoma. The two groups show no statistically significant differences in terms of temporary hypocalcemia, vocal cord palsy and hematoma (P=0.293, 1.000 and 0.683, respectively). All patients with complications recovered in postoperative follow-up time. No permanent or other serious procedure-related complications occurred in either group, and clinical outcomes appeared to be good.
| Endo group (20) | Open group (35) | P-value | ||
|---|---|---|---|---|
| Hypocalcemia | Temporary | 2 (10%) | 9 (25.7%) | 0.293 |
| Permanent | 0 | 0 | - | |
| Vocal cord palsy | Temporary | 2 (10%) | 4 (11.4%) | 1 |
| Permanent | 0 | 0 | - | |
| Hematoma | 1 (5%) | 1 (2.9%) | 0.683 | |
| Endo: Endoscopic. | ||||
Table 2: Postoperative complications.
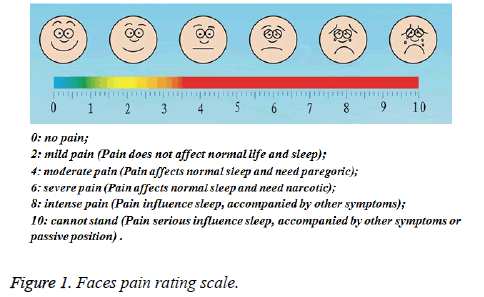
We adopt Faces Pain Rating Scale (showed as Figure 1) to assessment postoperative pain for the neck or anterior chest wall in two groups. Faces Pain Rating Scale is objective and practical, is easy to everyone to understand how to respond to 0 to 10.
We defined the scores 0 and 2 are the pain that can bearable, the rest of the scores are defined as the pain need to medical intervention.
Table 3 demonstrates postoperative pain for the neck or anterior chest wall in two groups. At first two days after surgery, the severity of pain for the neck or anterior chest wall in open group was higher than in endoscopic group (P=4.169 × 10-4 and 0.001), from third day after operation, the difference between two groups was not statistically significant, and most of the patients reported no severe pain one week after the operation.
| 0 | 2 | 4 | 6 | 8 | 10 | Bearable | Need to intervene | P | ||
|---|---|---|---|---|---|---|---|---|---|---|
| POD 1 | ET | 3 | 9 | 6 | 2 | 0 | 0 | 12 | 8 | 4.169 × 10-4 |
| Days | OT | 2 | 3 | 27 | 3 | 0 | 0 | 5 | 30 | |
| POD 2 | ET | 11 | 6 | 2 | 1 | 0 | 0 | 17 | 3 | 0.001 |
| Days | OT | 8 | 6 | 20 | 1 | 0 | 0 | 14 | 21 | |
| POD 3 | ET | 15 | 3 | 2 | 0 | 0 | 0 | 18 | 2 | 0.558 |
| Days | OT | 17 | 11 | 6 | 1 | 0 | 0 | 28 | 7 | |
| POD 1 | ET | 18 | 2 | 0 | 0 | 0 | 0 | 20 | 0 | NS |
| Week | OT | 33 | 2 | 0 | 0 | 0 | 0 | 35 | 0 | |
| POD: Postoperative Day; NS: Statistically Not Significant. | ||||||||||
Table 3: Postoperative pain for the neck or anterior chest wall in two groups.
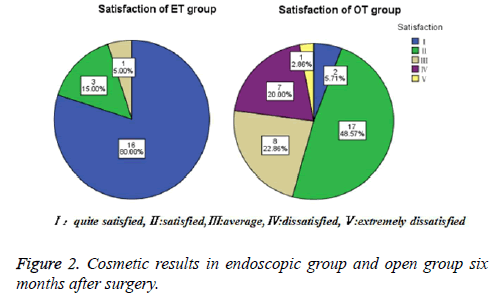
Data on patient satisfaction with cosmetic results are presented in Figure 2.
We define total satisfaction=quite satisfied+satisfied, total satisfaction in endoscopic group and in open group are nineteen (95%) and nineteen (54.3%), the postoperative cosmetic result was more excellent in endoscopic group than in open group (P=0.002).
Discussion
The prevalence of PTC is growing at a faster rate than any other malignancy [20]. To avoid cosmetically undesirable outcomes, various approaches of endoscopic techniques have been developed with the aim of minimizing or eliminating incisional scar formation on the neck.
The first endoscopic neck surgery was initiated for parathyroidectomy by Gagner [21] in 1996, and Huscher [22] performed the first endoscopic thyroidectomy in 1997. ET for benign disease and PTMC, offering an extremely satisfactory cosmetic result, has gained general acceptance in China [23].
Patients with PTMC who received ETBA could achieve similar efficacy, compared with those who received conventional OT. The rates of transient hypoparathyroidism and recurrent laryngeal nerve injury after OT range from 4.3% to 17.7% and 2.2% to 3.7%, respectively [16,24,25]. In this study, the result of transient hypoparathyroidism after ETBA was similar (10%), but the rate of recurrent laryngeal nerve injury was observed in 10% of patients, probably because the lack of enough cases, this was not statistically significant (P=1.000). We obtained a relatively similar complication rate in endoscopic and open group. No permanent complication was discovered. During the short follow-up period, there was no recurrence or metastatic cases in both groups. Because at present develops the surgery number are few, the operation time was longer in endoscopic group than in open group (169 ± 56.489 min versus 127.74 ± 42.051 min, P=0.003). With the proficiency of surgical technique, more case of illness and experience accumulation, the time will be shortening.
ETBA has the advantages of less pain and favorable cosmesis. According to our results, postoperative pain score of ‘bearable’ at 1 d, 2 d, 3 d and 7 d were 12, 17, 18 and 20 patients respectively in endoscopic group, and 5, 14, 28, 35 respectively in open group. At first two days, the differences were statistically significant (P=4.169 × 10-4 and 0.001 respectively), after one week, all patients could ‘bearable’ the pain for the neck or anterior chest wall. Meanwhile, only one case was ‘average’ with the cosmetic result in endoscopic group, but in open group, 8 cases were ‘average’ and 7 were ‘dissatisfied’ and 1 was ‘extremely dissatisfied’ with the cosmetic result. The total satisfaction were 19 and 19 in two groups respectively, which was statistically significant (P=0.002). ETBA provide a safe excision of the thyroid pathology with the absence of a scar in the neck. The shorter a single incision is, the less it disturbs the integrity of the anatomic structure. After ETBA, the incisions can not only be hidden with everyday clothing but also reduced. ETBA satisfied patients’ request for improved postoperative quality of life, which was especially important in patients who wished to keep their surgical history private [19,26].
With an endoscope to magnify the surgical field and the approach described here, we easily identified and preserved the recurrent laryngeal nerve and parathyroid glands. With the widespread adoption of ET and the development of new surgical techniques and instruments, the application criteria for ET will be extensive [27].
Although there is room for improvement in terms of shortening the operation time and accumulating more cases, the preliminary results of this study are encouraging. ETBA patients showed significantly greater improvement in emotional function and physical function.
Conclusion
In a word, ETBA is a technically feasible and safe procedure with outcomes similar to those of conventional OT when considering short-term adverse events. It has the advantage of better cosmetic results than OT. ETBA is an effective alternative method for selected patients with PTMC. We are optimistic about the future expansion of its applicability. Our future study will focus on dissemination of ETBA and meets the needs of more patients.
Acknowledgement
The authors thank Project Funds: General Studies Program of Medicine and Health Care in Zhejiang Province (2015KYA205.Clinical Research of the Treatment of T1a Period Papillary Thyroid Carcinoma in Low-risk Female Patients using Endoscopic Thyroidectomy via a Breast Approach).
References
- Shen X, Miao ZM, Lu W, Gu DL, Yang D, Shen H, Geng F. Clinical experience with modified Miccolis endoscopic thyroidectomy for treatment of thyroid carcinoma in 86 cases. Eur J Med Res 2013; 18: 51-55.
- Wu B, Ding Z, Fan Y, Deng X, Guo B, Kang J, Zhong C, Yang Z, Zheng Q. Video-assisted selective lateral neck dissection for papillary thyroid carcinoma. Langenbecks Arch Surg 2013; 398: 395-401.
- Lee HS, Chai YJ, Kim SJ, Choi JY, Lee KE. Influence of body habitus on the surgical outcomes of bilateral axillo-breast approach robotic thyroidectomy in papillary thyroid carcinoma patients. Ann Surg Treat Res 2016; 91: 1-7.
- Lee MC, Mo JA, Choi IJ, Lee BC, Lee GH. New endoscopic thyroidectomy via a unilateral axillo-breast approach with gas insufflation: Preliminary report. Head Neck 2013; 3: 471-476.
- Bae JS, Park WC, Song BJ, Jung SS, Kim JS. Endoscopic thyroidectomy and sentinel lymph node biopsy via an anterior chest approach for papillary thyroid cancer. Surg Today 2009; 39: 178-181.
- Tan CT, Cheah WK, Delbridge L. Scarless (in the neck) endoscopic thyroidectomy (SET): an evidence-based review of published techniques. World J Surg 2008; 32: 1349-1357.
- Zhang W, Dang C, Shan C, Liu S, Jiang Z, Wang B, Qiu M. Use of a mini-instrument in endoscopic thyroidectomy via a breast approach to improve cosmetic outcomes. Biosci Trends 2014; 8: 280-285.
- Kitagawa W, Shimizu K, Akasu H, Tanaka S. Endoscopic neck surgery with lymph node dissection for papillary carcinoma of the thyroid using a totally gasless anterior neck skin lifting method. J Am Coll Surg 2003; 196: 990-994.
- Kim YS, Joo KH, Park SC, Kim KH, Ahn CH. Endoscopic thyroid surgery via a breast approach: a single institutions experiences. BMC Surg 2014; 14: 49.
- Woo SH. Endoscopic-assisted total thyroidectomy via lateral keloid scar incision. Clin Exp Otorhinolaryngol 2014; 7: 338-341.
- Yang M, Shen D, Sakamoto N. Population-based study evaluating and predicting the probability of death resulting from thyroid cancer and other causes among patients with thyroid cancer. J Clin Oncol 2013; 31: 468-474.
- Choi JY, Lee KE, Chung KW, Kim SW, Choe JH, Koo DH, Kim SJ, Lee J, Chung YS, Oh SK, Youn YK. Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc 2012; 26: 948-955.
- Lv B, Zhang B, Zeng QD. Total endoscopic thyroidectomy with Intraoperative laryngeal nerve monitoring. Int J Endocrinol 2016; 2016: 7381792-7381796.
- Li ZY, Wang P, Wang Y, Xu SM, Cao LP. Endoscopic thyroidectomy via breast approach for patients with Graves disease. World J Surg 2010; 34: 2228-2232.
- Lee MC, Park H, Choi IJ, Lee BC, Lee GH. Comparative study of a gasless transaxillary approach versus a bilateral axillo-breast approach for endoscopic thyroidectomy in a single institute. Head Neck 2014; 336: 702-708.
- Jeong JJ, Kang SW, Yun JS, Sung TY, Lee SC, Lee YS, Nam KH, Chang HS, Chung WY, Park CS. Comparative study of endoscopic thyroidectomy versus conventional open thyroidectomy in Papillary Thyroid Microcarcinoma (PTMC) patients. J Surg Oncol 2009; 100: 477-480.
- Sasaki A, Nakajima J, Ikeda K, Otsuka K, Koeda K. Endoscopic thyroidectomy by the breast approach: a single institutions 9-year experience. World J Surg 2008; 32: 381-385.
- Ohgami M, Ishii S, Arisawa Y. Ohmori T, Noga K, Furukawa T, Kitajima M. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 2000; 10: 1-4.
- Jiang ZG, Zhang W, Jiang DZ, Zheng XM, Shen HL, Shan CX, Liu S, Qiu M. Clinical benefits of scarless endoscopic thyroidectomy: an experts experience. World J Surg 2011; 3: 553-557.
- Hughes DT, Haymart MR, Miller BS, Gauger PG, Doherty GM. The most commonly occurring papillary thyroid cancer in the United States is now a microcarcinoma in a patient older than 45 years. Thyoid 2011; 21: 231-236.
- Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg 1996; 83: 875.
- Hüscher CS, Chiodini S, Napolitano C, Recher A. Endoscopic right thyroid lobectomy. Surg Endosc 1997; 11: 877.
- Tan Z, Gu J, Han Q, Wang W, Wang K. Comparison of conventional open thyroidectomy and endoscopic thyroidectomy via breast approach for papillary thyroid carcinoma. Int J Endocrinol 2015; 2015: 239610.
- Cao F, Xie B, Cui B, Xu D. Endoscopic vs. conventional thyroidectomy for the treatment of benign thyroid tumors: A retrospective study of a 4-year experience. Exp Ther Med 2011; 2: 661-666.
- Chung YS, Choe JH, Kang KH, Kim SW, Chung KW. Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg 2007; 31: 2302-2306.
- Yan H, Wang Y, Wang P, Xie Q, Zhao Q. Scarless (in the neck) endoscopic thyroidectomy (SET) with ipsilateral levels II, III, and IV dissection via breast approach for papillary thyroid carcinoma: a preliminary report. Surg Endosc 2015; 29: 2158-2163.
- Yoo H, Chae BJ, Park HS, Kim KH, Kim SH, Song BJ, Jung SS, Bae JS. Comparison of surgical outcomes between endoscopic and robotic thyroidectomy. J Surg Oncol 2012; 105: 705-708.