- Biomedical Research (2013) Volume 24, Issue 4
Co-infection of Hepatitis C Among HIV-infected Population with Different Risk Groups in Kathmandu, Nepal.
Chet Raj Ojha*, Khagendra KC, Geeta ShakyaNational Public Health Laboratory, Teku, Kathmandu, Nepal
- *Corresponding Author:
- Chet Raj Ojha
Microbiologist HIV unit
National Public Health Laboratory
Teku, Nepal
Accepted Date: May 27 2013
Citation: Ojha CR, Khagendra KC, Shakya G. Co-infection of Hepatitis C Among HIV-infected Population with Different Risk Groups in Kathmandu, Nepal. Biomedical Research 2013; 24 (4): 441-444.
Abstract
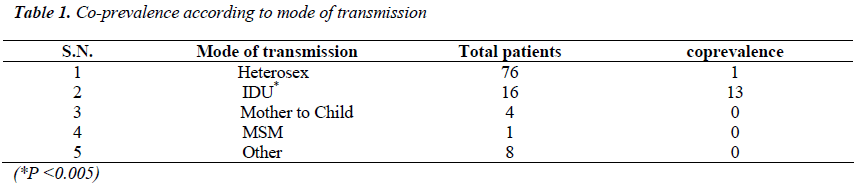
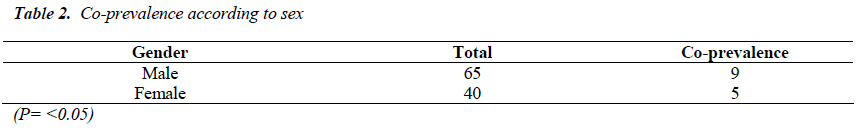
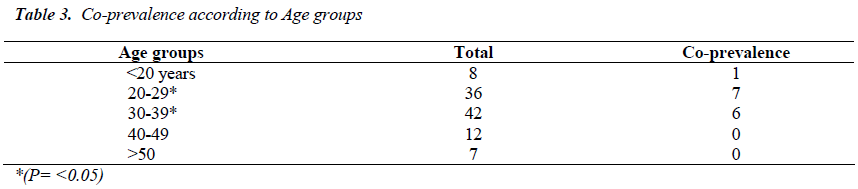
Prevalence of HCV infection has increased in recent decades as a consequence of its incorporation into effective transmission networks, such as blood transfusion and most notably injecting drug users (IDU). Seroprevalence of Co- infection is common due to the common mode of transmissions in both HIV and HCV. It is estimated that 50% to 90% of IDUs with HIV also have HCV infection. This study was intended to identify the prevalence of Hepatitis C among HIV infected people. A descriptive cross-sectional type of study was conducted in National Public Health Laboratory (NPHL) Kathmandu Nepal during the period from November 2011 to May 2012. Total of 678 cases with one or more risk behaviors were tested for anti-HIV1/2 by ELISA method during the study period. Confirmation is done by Western Blotting method. Positive samples (105) were screened for Anti-HCV by ELISA method. Among total 105 HIV positive cases, 13.33% were found to be reactive to Anti HCV antibody. Co-prevalence was found to be higher in age group 20-29 with 24.13 %( 7/29) followed by age group 30-39 with 16.66% (6/36). Co-prevalence among male cases was found to be 13.84% and among female 12.5 %( 5/40). Intravenous drug users were found to be highly co-infected (75%). Heterosexual groups are found to be co-infected with 1.3% (1/76). Coinfection is not found among cases of mother to child transmission group, blood transfused group and men sex with men group. The level of significance was found to be statistically significant with P<0.05 for Intravenous drug user.
Keywords
HCV, HIV, IDUs, Co-infection
Introduction
HIV and HCV show some common biological features like both are RNA viruses and both show a large heterogenicity of their viral genomes producing various genotypes. These viruses also have some differences, like HCV belongs to the Flaviviridae family and HIV to the Retroviridae family. Falviviruses have a single RNA strand whereas retroviruses have double RNA strands. The HIV-RNA, transcripted to DNA by the reverse transcriptase (RT), integrates in the infected cells genome, constituting the integrated provirus; this integration is the cause of the irreversibility of HIV infection. In contrast, the HCV genome does not integrate into the cells genome and the replication of the virus takes place in the liver cells cytoplasm. This non-integration makes it easier to eradicate HCV and hence to cure the infection. These viruses share similar routes of transmission like through blood and blood products, sharing of needles to inject drugs and sexual route [1]. Common mode of transmission of various infections can result in the simultaneous prevalence of these infections in the same human population [2].
Some evidence suggests that liver disease progression may be particularly aggressive in people who are already HIV positive when they acquire HCV. By preserving or restoring immune function, effective antiretroviral treatment appears to partially hold in check or even reverse some of the detrimental impact of HIV on HCV disease progression and vice versa [3]. People living with HIV who are also coinfected with HCV are at increased risk of serious life threatening complications. It may also results in complication in management of HIV infection [4]. The greater proportion of HIV/HCV coinfected people may progress to cirrhosis (serious liver scarring) and liver disease than those with HCV alone [5].
The study has been conducted in National Public Health Laboratory (NPHL) in order to find the HIV and HCV Co-prevalence among different patient reported to tertiary Health care centre. The study was also aimed to identify the highly risk group for HIV and HCV co infection and thus help in appropriate drug regimen and awareness.
Materials and Methods
A descriptive cross-sectional type of study was conducted in National Public Health Laboratory (NPHL), Teku, and Kathmandu Nepal during the period from 9th of November 2011 to 14th of May 2012. Patients attending at NPHL for Anti-HIV testing and ready to give consent for study were included in the study. Total of 678 patients were tested for anti-HIV by ELISA method during the study period. 105 samples were positive for Anti-HIV and screened for Anti-HCV by ELISA method. Data were analyzed statistically by chi square (χ2) test and P value determination with the help of a computer based program, Statistical Package for Social Science (SPSS) Software version 13.0, MS Excel and MS word 2007. Chi-square test was used to find level of significance.
Results
Among total 678 cases attending NPHL, 105 (15.48%) were anti HIV 1 and 2 reactive. Among total HIV positive cases, 13.33% were found to be reactive to Anti HCV antibody. Co-prevalence was found to be higher in age group 20-29 with 24.13 %( 7/29) followed by age group 30-39 with 16.66% (6/36). Co-prevalence among male cases was found to be 13.84% and among female 12.5 %( 5/40). Intravenous drug users were found to be highly co-infected with (75%). Heterosexual groups are found to be co-infected with 1.3% (1/76). Co-infection is not found among cases with mother to child, Blood transfusion and men sex with men. The level of significance was found to be statistically significant with P<0.05 for Intravenous drug user.
Discussion
A significantly high prevalence of Hepatitis C was found among the people living with HIV AIDS. Coprevalence of HIV/HCV was reported to be higher in male population. This may be attributed to migration in search of work or being foreign employee. Higher prevalence was found to be among age group 20-39 which might be due to being in reproductive age group and being influence by friends and the social stigmas. Also the people with higher co-prevalence were reported in Intravenous drug users.
In a study conducted in central Nepal, the co-infection rate with HCV and HIV among blood donors was 10.8%. All co-infected donors were male [6]. In another study Co-infection rate of HIV among HCV was reported to be 3.59% [2]. A higher rate of co-infections was reported by this current study. This might be due to inclusion of only blood donors by previous studies. The current study was the only study which was conducted among the population other than blood donors.
Studies done in Different part of India show that coinfection of HCV was found to be 3.02% to 22.2% [7,8]. A report from Imphal studied co-infection of HIV and HCV in injecting IV drug users was found 52.4% which is higher than the result obtained in present study [9]. In the study conducted in west Bengal 7.27% were found to be co-infected with HCV. Heterosexual were 80.91% of 110 HIV positive patients, out of which 5.62% were anti-HCV positive respectively. In West Bengal study among the coinfected patients, the predominant risk was IVD's (37.77%), heterosexual (13.3%) and blood transfusion recipients (6.6%). HCV and HIV prevalences were strongly correlated in a study conducted among Asian population [2].
A study conducted in U.S.A shows that, 32.4% were infected with both HIV and HCV, and 67.6% were seropositive only for HIV. In the United States, an estimated 16-25% of HIV positive individuals are coinfected with HCV, as many as 90% of the people who acquired HIV through injection drug use are co-infected with HCV [11,12,13].
Sero-prevalence of HIV according to sex category was found to be higher in male and among age group 20-39 years. Male among this age group might have been shown higher prevalence due to being in reproductive age group, migration in search of work or being foreign employee. To prevent this impact strict testing system should be done for immigrants and drugs regimen should be taken properly.
Where there is a scarcity of information on HIV/ HCV prevalence, particularly in developing countries like Nepal, our study on the prevalence of HCV among HIV-infected individuals is sure to provide a useful insight to researchers working on HIV/HCV co-infection. Finally, further studies of HIV/HCV co-infection are needed to explore in more detail of the genotypes of HCV, current prevention strategies and the therapeutic management of this condition.
Acknowlegement
We would like to express gratitude to Bishnu Upadhyay, Ms. Kamala Upreti, Ms.Tibrata Sharma and all the respected staffs of NPHL for helping and making this work easier. We are also thankful to all the subjects of the study, volunteers of Teku hospital and lab staffs. We Acknowledge Prof. Shambhu Pant of Nepal Army Institute of Health Science for providing softwares and guiding in data analysis.
References
- Khaja MN, Ponamgi SPD, Rahamathulla S, Kumar YN, Chandra M, Lakshmi N, Habibullah CM. Prevalence of Hepatitis C Virus (HCV) Coinfection in HIV Infected Individuals in South India and Characterization of HCV genotypes. Indian Journal of Medical Microbiology 2009; 27(1): 12-16.
- Shrestha AS, Ghimire P, Tiwari BR, Rajkarnikar M. Co-infection rate of HIV, HBV and Syphilis among HCV Sero positive identified blood donors in Kathmandu, Nepal. Infection Ecology and Epidemiology 2012; 2: 66-70.
- Highleyman L. HIV/HCV Coinfection: A New Era of Treatment. BETA. ALL/WINTER 2011; 30-47.
- Centre for Disease controls and prevention. HIV and Viral Hepatitis. 2009 http://www.cdc.gov/hiv/resources/factsheets/PDF/HIV-Viral-Hepatitisacc.pdf
- Bonacini M, Puoti M. Hepatitis C in patients with human immunodeficiency virus infection: Diagnosis, natural history, meta-analysis of sexual and vertical transmission and therapeutic issues. Arch Intern Med 2000; 160: 3365-3373.
- Karki S, Ghimire P, Tiwari BR, Shrestha AC, Gautam A, Rajkarnikar M. Sero prevalence of HIV and Hepatitis C coinfection among blood donors in Kathmandu valley, Nepal. Southeast Asian J Trop med Public 2009; 40: 66-70.
- Hussain T, Sharma KS, Kulshreshtha KK, Yadav VS. HIV and other co-infections among drug users attending the Integrated Counselling & Testing Centre (ICTC) at Agra, India. HIV & AIDS Review 2009; 11: 49-53.
- Anbazhagan GK, Krishnamoorthy S, Thiyagarajan T. Seroprevalence of HCV and its co-infection with HBV and HIV among liver disease patients of South Tamil Nadu. World J Hepatol 2010; 27: 42-48
- Devi K, Singh NB, Singh HL, Singh YM. Coinfection by human immunodeficiency virus, hepatitis B virus and hepatitis C virus in injecting drug users. J Commun Dis 2009; 37: 73-77.
- Brewer DD and Khan AA. HCV and HIV prevalence strongly correlated in Asian communities with reservoirs of HIV in high-risk groups. J Infect Dev Ctries 2010; 4: 442-447.
- Sherman KE, Rouster SD, Chung RT. Hepatitis C virus prevalence among patients infected with human immunodeficiency virus: a cross-sectional analysis of the US adult AIDS Clinical Trials Group. Clin Infect Dis. 2002; 34: 831-837.
- Tedaldi EM, Hullsiek KH, Malvestutto CD, Arduino RC, Fisher VP Gaglio J, Jenny-Avital ER, McGowan JP and Perez G. Prevalence and characteristics of hepatitis C virus coinfection in a human immunodeficiency virus clinical trials group: the Terry Beirn Community Programs for Clinical Research on AIDS. Clin. Infect. Dis 2003; 36: 1313–1317
- Thomas DL. Hepatitis C and human immunodeficiency virus infection. Hepatology 2002; 36: S201-209.