Research Article - Biomedical Research (2017) Volume 28, Issue 6
Cognition and attitude of bachelor dental students towards HIV/AIDS
Ning Gao1, Kun Fu1, Wei He1, Rui Li1* and Weihua Lou2*1Department of Stomatology, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450052, PR China
2Department of ENT, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450052, PR China
- *Corresponding Authors:
- Weihua Lou
Department of ENT
The First Affiliated Hospital of Zhengzhou University
PR China - Rui Li
Department of Stomatology
The First Affiliated Hospital of Zhengzhou University
PR China
Accepted date: November 05, 2016
Abstract
Background: Effective oral health care is vital for HIV/AIDS positive patients. Dental practitioners should master accurate knowledge and proper attitudes towards HIV-positive patients. This research aimed to investigate the knowledge and attitudes towards HIV/AIDS-related infections in fourth to fifth year bachelor dental students in Henan province.
Methods: A survey was conducted to analyze the knowledge and attitudes of dental students with different clinical practice towards HIV/AIDS-infected patients.
Results: The average scores of HIV/AIDS-related knowledge in the fourth- and fifth-year students was 69.80 ± 9.72 and 79.41 ± 6.30, respectively, showing a significant difference. There were no significant differences in the basic practical knowledge and awareness of HIV/AIDS transmission routes between two groups. However, there were significant differences between two groups, regarding the knowledge on oral lesions, high-risk populations, and transmission in dental settings. Furthermore, students in both groups had very negative or passive attitudes towards AIDS patients, with the fifth-year students possessing a much more positive attitude.
Conclusions: A good knowledge doesn’t mean a positive attitude towards HIV/AIDS. Clinical practice and urgent education are required to improve this condition.
Keywords
HIV/AIDS, Cognition, Attitude, Dental students
Introduction
Phobia toward human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) or fear of AIDS has been a very real problem since the virus was discovered [1]. A majority of people including dentists still regard blood and saliva as the major routes of AIDS transmission and subsequent infection. Thus, even medical doctors try to avoid treating HIV positive patients despite the low possibility of being infected [2,3]. While it has been reported that doctors no longer reject AIDS patients [4,5], the latest researches indicate that dentists still lack sufficient understanding of the HIV/ AIDS virus [6,7]. Nowadays, the survival rate of AIDS patients is higher than ever before, due to the improvement of health care including greatly improved oral and dental hygiene [8]. Consequently, dental students are expected to play a vital role in the future medical treatment of HIV/AIDS patients. Dental students should deepen their knowledge about the HIV/AIDS virus and greatly improve their attitudes toward HIV sufferers [9]. Henan province, one of provinces with the largest population in China, has the highest proportion of HIV/AIDS sufferers. Unfortunately, there is a desperate shortage of dental practitioners due in large part to potential risk for HIV/AIDS infection. This study was to investigate the concerns of dental students about this risk and the knowledge and attitudes towards HIV/AIDS sufferers.
Material and Methods
The survey was conducted in the 4th and 5th year bachelor students majoring in dentistry. They were recruited from the First Affiliated Hospital of Zhengzhou University in Henan province, China. This survey aimed to investigate and evaluate their knowledge and attitudes toward the HIV/AIDS virus and patients suffering from HIV infection/AIDS. Following questions were included in this survey: 1). Questions were designed to assess the theoretical and practical understanding of the HIV/AIDS virus; 2). Questions were designed to investigate the attitudes towards HIV/AIDS patients. This survey employed a self-administered structured questionnaire based on previous studies [9,10], and this study was approved by the Research and Ethical Committee of the First Affiliated Hospital of Zhengzhou University, Henan, China. The questionnaire covered the following aspects: 1) the virus (HIV) and related disease (AIDS); 2) potential routes of transmission; 3) oral lesions associated with HIV infection; 4) risk groups; 5) HIV transmission in the dental setting; 6) personal attitudes regarding the treatment of HIV-positive patients, legal aspects, rights of HIV-positive health personnel to practice, and willingness to treat HIV/AIDS patients.
There are a total of fifty questions regarding the “HIV/AIDS-related knowledge” in the questionnaire. The answer choices to each close-ended question were designated as either “Yes, No or N/A”.
The answers “No or N/A” were defined as Incorrect response and scored “0” whilst the answer “Yes” as Correct response with a score of 2. As a consequence, the total score of each participant ranged from 0 (all incorrect responses) to 100 (all correct responses). The level of knowledge was categorized into four groups according to the final score: weak, moderate, good and excellent. The “Attitude” was evaluated based on seventeen close-ended questions in the questionnaire, and all of the responses were scaled directly into five groups according to the Likert Scale) [10]. The Likert Scale was developed to measure the extent of attitudes to questions, with which the participants agree. According to the designated questionnaire, the lowest total score was 17, meaning that all respondents strongly disagreed with the questions; highest total score was 85, meaning that all the participants agreed with the issues. The attitudes of recruited students were accordingly divided into three groups according to the final score: Negative (17-49), Passive (50-74), and Positive (75-85). The higher the score, the more tolerant and more positive the attitudes towards AIDS-infected patients are.
Statistical analysis
Statistical analysis was performed with SPSS 17.0 and t-test was employed for comparisons between two groups. A value of P less than 0.05 was considered statistically significant.
Results
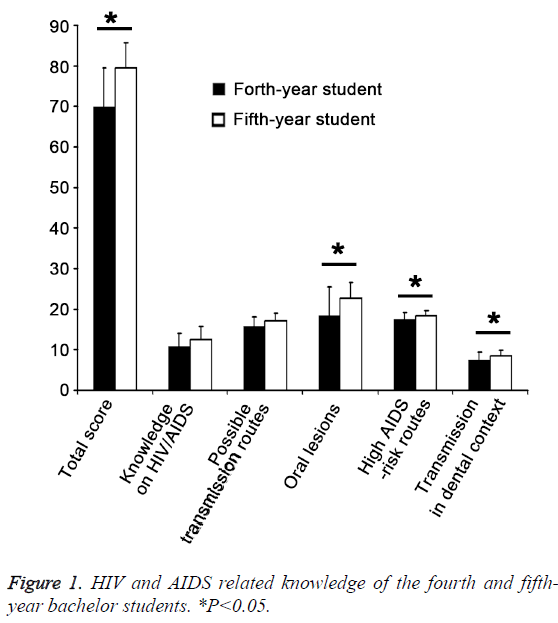
A total of 90 fourth-year students and 95 fifth-year students were recruited into this study. The Return Rate and Completion Rate of the questionnaire were 94% and 92.2%, respectively. The Male/Female ratio was 1:1.90 in fourth-year students and 1:2.16 in fifth-year students. With respect to the knowledge towards AIDS-infected patients, the average score of HIV/ AIDS-related knowledge was 69.80 ± 9.72 (mean ± SD) for fourth-year students and 79.41 ± 6.30 for fifth-year students, showing significant difference between them (P<0.05). The proportion of students with the scores higher than 90, which indicates the excellent knowledge, was 3.33% and 2.11% in fourth- and fifth-year students, respectively (Table 1). There were no significant differences in the basic knowledge and knowledge about transmission routes between two groups (Chi-square Test). However, significant differences were observed in knowledge about oral lesions, high-risk population, and transmission in dental settings (Figure 1).
| The Fourth Year | The Fifth Year | |
|---|---|---|
| Weak (0-69) | 41.1% | 4.21% |
| Moderate (70-79) | 50% | 42.11% |
| Good (80-89) | 5.56% | 51.58% |
| Excellent (90-100) | 3.33% | 2.10% |
Table 1: The levels of cognition of HIV/AIDS-related knowledge based on the calculated scores of the fourth and fifth grade students.
Ten questions were designated for the evaluation of knowledge related to HIV and AIDS. The mean scores were 10.73 ± 3.38 and 12.57 ± 3.20 in fourth- and fifth-year students, respectively, indicating that most respondents had about six correct answers to ten questions regarding the basic information about the virus and disease. No statistically significant difference in the knowledge on HIV/AIDS was found between two groups (P<0.05). An unexpected phenomenon was observed in this study that a vast majority of students had gained a correct understanding of the routes towards HIV/AIDS transmission, and the average score was 15.80 ± 2.34 and 17.20 ± 1.88 for fourth- and fifth- year students, respectively. There was no significant difference in the knowledge on possible routes towards AIDS transmission between fourth- and fifth-year students (P=0.484), indicating that the fourth- and fifth-year dental students have similar knowledge about this aspect. The potential routes for HIV/ AIDS transmission included (a) blood transmission (blood transfusion or organ donation from infected individuals); (b) Mother-to-Child Transmission/MTCT (breast-feeding of HIV-infected mother) and (c) Sexual transmission. There are also some other but not easily perceived routes including the cross-utilization of injection needles and surgical devices with HIVpositive patients.
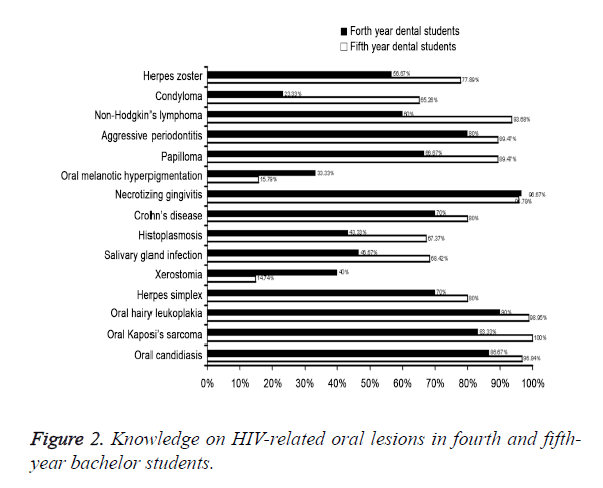
However, there were some misunderstandings regarding unsupported routes for HIV/AIDS transmission among these students as in public without a medical education background. For example, some students even regarded the mosquito bite and mucus or nasal fluid from HIV-infected individuals as the potential routes for HIV/AIDS transmission. Fifteen questions were designed for the oral lesions related to HIV/AIDS. The scores of all answers averaged at 18.33 ± 7.25 and 22.67 ± 3.80 for fourth- and fifth-year students, respectively. Most of students could appropriately build up the relationship between HIV/AIDS and some oral lesions such as oral hairy leukoplakia, Kaposi sarcoma and oral candidiasis. Even though the fifth-year students got a significantly higher score as compared to fourth-year students (P<0.05), none in both groups answered all the questions correctly (Figure 2).
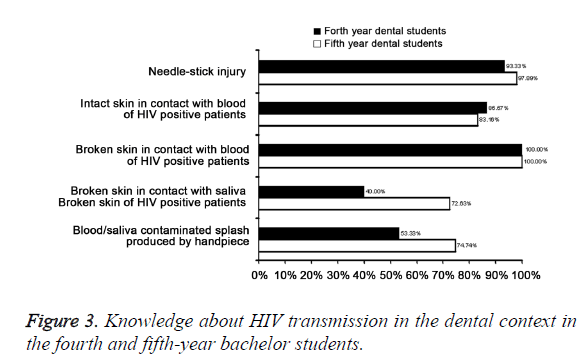
The populations susceptible to AIDS were classified into Intravenous Drug Users/IVDUs, patients who regularly require blood transfusion or blood products, and individuals who have high-risk sexual activities including buggers, prostitutes and those having no fixed sexual partners. The students at the fourth and fifth year of bachelor study had the average score in terms of this issue of 17.47 ± 1.79 and 18.40 ± 1.36, respectively, and significant difference was observed between them (P<0.05) in their understanding of high AIDS-risk populations. Five questions were designed for the knowledge about HIV transmission in the dental context. The fourth- and the fifth-year bachelor students had the average score in this issue of 7.47 ± 2.01 and 8.54 ± 1.39, respectively, indicating that these students have a good understanding in this aspect of their professional knowledge (Figure 3). Moreover, there was a significant difference in the knowledge about HIV transmission in the dental context between two groups (P<0.05). The results showed that the overall mean attitude score was 56.70 ± 7.57 and 61.25 ± 6.32 for the fourth- and the fifth-year students, respectively, and significant difference was observed in the attitudes toward HIV/AIDS patients between two groups. The proportion of students with positive attitude among the fourth- and fifth- year students was only 2.22% and 2.11%, respectively, which indicates most of students have a negative or passive attitude to these HIV/AIDS patients.
Discussion
A growing number of AIDS-related patients who suffer from different degrees of oral damage requires appropriate medical care [11,12]. As a consequence, dentists are responsible for providing professional oral health care to these patients. The dental students will be the main force in this field, but they need to possess adequate HIV/AIDS-related knowledge and appropriate attitudes towards their patients [13]. Previous studies have found that attitudes towards a disease are directly proportional to the disease-related knowledge [14,15]. However, our study revealed that most of dental students had a negative position towards AIDS patients although they had rich AIDS-related knowledge. The reason for this partly lies in some misunderstandings among students [16,17]. The concept of “HIV-antibody carriers” means that the patients have already been affected by HIV. However, some students regard it as being capable of immunity against AIDS. Similarly, a proportion of dental students regard mosquito bite, public bath and toilet exposure as possible routes for AIDS transmission, despite the fact that there is evidence to suggest that this is highly unlikely in each case [18]. The National Centers for Disease Control (CDC) has determined that the HIV virus cannot reproduce or survive in biting and bloodsucking insects like mosquitoes. This makes HIV different from other microorganisms that can be transmitted through mosquitoes. However, about 91.58% of dental students in this survey regarded infants of HIV/AIDS mothers as a risk group for HIV/AIDS. There is placental transmission in these infants, and breastfeeding is also another route of transmission after birth [19].
Dental students are undoubtedly familiar with the common symptoms of HIV/AIDS especially the oral manifestations. Furthermore, they are considered to have better basic knowledge in comparison to dental students in countries which have generalized HIV epidemics. As many as forty oral manifestations of HIV/AIDS have been reported. The existing problem is that dental students are mostly aware of the major oral manifestations strongly associated with HIV/AIDS including Kaposi sarcoma, oral candidiasis and oral hairy leukoplakia. However, not every HIV/AIDS patient always presents these classic oral manifestations. Other oral lesions, which are not closely related to HIV/AIDS, also need to be emphasized during examinations. These uncommon manifestations include oral melanotic hyperpigmentation, non- Hodgkin’s lymphoma and salivary gland disease. Further education highlighting the difference between HIV and non HIV related oral manifestations will be helpful for a more accurate diagnosis and help to alleviate some of the fear that students experience and reduce their reluctance to provide treatment to affected patients. Other opportunities to improve AIDS-related knowledge include barbering procedures, which must be more comprehensively studied as a part of the curriculum as they have a higher risk of AIDS transmission. Currently these procedures are excluded from the high AIDS-risk areas. Additionally, dental students are easy to ignore the possibility of HIV transmission by aerosol inhaled from hand pieces, a situation which must be addressed.
In terms of the students’ attitudes, as reflected in the survey responses, a vast majority of dental students still expressed negative or passive attitudes toward HIV/AIDS patients, which is not parallel to their level of knowledge about HIV/AIDS in this survey. Similarly, in an Iran study, only 1% had positive attitudes, which means professional attitudes regarding treatment still need significant improvement, despite the high level of knowledge in practice [10]. The fact that increased professional knowledge does not immediately accord acceptance to HIV/AIDS patients, has also been proven by other studies [3,10] Cardio-Pulmonary Resuscitation (CPR) is considered as an opportunity for HIV transmission in one third of surveyed students. Consequently, they are unwilling to carry out the mouth-to-mouth artificial respiration, even though studies have shown that such an action carries a low risk for HIV/AIDS transmission [20]. There may be an improvement in their attitude after the initiation of clinical work. Thus, it is necessary to find more measures to effectively improve the attitudes of dental students toward ADIS-related patients as shown in previous studies [21] and this study.
Only 18.95% of dental students in this study considered that they were entitled to reject the treatment to HIV/AIDS patients, which was different to the findings from a Kuwait study on students and a Brazilian study on dental professors [22]. Actually, dentists are obligated to provide their professional and effective treatment to all patients. In the meanwhile, a large part of students suggested that each patient should be treated as being potentially infectious, but infection control precautions are required to be undertaken with every patient treated [23]. This is because some HIV/AIDS patients conceal to declare their illness in order to avoid the possibility of being rejected for their dental care [3]. This comparative survey revealed there were significant differences in both knowledge structure and attitudes between fourth- and fifth-year bachelor dental students. The dental students in the fourth year of bachelor study expressed an inexplicable sense of fear due to the lack of clinical practice. There is a big improvement in the attitude of the fifth-year dental students towards AIDS along with a better integration of theoretical knowledge and practical experience. It is also beneficial for an improved understanding and proper treatment of HIV/AIDS related patients.
Taken together, this study indicates that a large majority of the fourth- and fifth-year bachelor dental students are unable to move past a negative attitude towards HIV/AIDS. This indicates that there is still misunderstanding about HIV/AIDS and it is necessary to improve this situation with better educational methods. This study also suggests that the misunderstanding and improper attitudes towards this disease and those who are affected by it need be changed and corrected [24,25]. Perhaps, through increasing the knowledge in relation to actual HIV/AIDS transmission routes and reinforcing the appropriate attitudes towards HIV/AIDS sufferers, the current negative attitude and discrimination will be significantly improved.
Limitations
In the present study, only the fourth and fifth year dental students were recruited from Zhengzhou University in Henan province, China. Thus, the results from this study cannot generalize in entire dental students. To gain a more comprehensive and complete understanding of student’s knowledge and attitudes, studies with large sample size are needed to investigate these issues in dental students from different grades. Only can a proper assessment of what needs to be done to improve these situations be fully undertaken.
Acknowledgement
This study was supported by the Nature Science Foundation of China (China, 81300843).
References
- Crossley ML. An investigation of dentists' knowledge, attitudes and practices towards HIV+ and patients with other blood-borne viruses in South Cheshire, UK. Br Dent J 2004; 196: 749-754.
- Borsum KM, Gjermo PE. Relationship between knowledge and attitudes regarding HIV/AIDS among dental school employees and students. Eur J Dent Educ 2004; 8: 105-110.
- Brailo V, Pelivan I, Skaricic J, Vuletic M, Dulcic N, Cerjan-Letica G. Treating patients with HIV and Hepatitis B and C infections: Croatian dental students' knowledge, attitudes, and risk perceptions. J Dent Educ 2011; 75: 1115-1126.
- Ryalat ST, Sawair FA, Shayyab MH, Amin WM. The knowledge and attitude about HIV/AIDS among Jordanian dental students: (Clinical versus preclinical students) at the University of Jordan. BMC Res Notes 2011; 4: 191.
- Fotedar S, Sharma KR, Sogi GM, Fotedar V, Chauhan A. Knowledge and attitudes about HIV/AIDS of students in H.P. Government Dental College and Hospital, Shimla, India. J Dent Educ 2013; 77: 1218-1224.
- Park JC, Choi SH, Kim YT, Kim SJ, Kang HJ, Lee JH, Shin SC, Cha YJ. Knowledge and attitudes of Korean dentists towards human immunodeficiency virus/acquired immune deficiency syndrome. J Periodontal Implant Sci 2011; 41: 3-9.
- Astrom AN, Nasir EF. Predicting intention to treat HIV-infected patients among Tanzanian and Sudanese medical and dental students using the theory of planned behaviour--a cross sectional study. BMC Health Serv Res 2009; 9: 213.
- Reif S, Pence BW, Hall I, Hu X, Whetten K, Wilson E. HIV Diagnoses, Prevalence and Outcomes in Nine Southern States. J Community Health 2015; 40: 642-651.
- Hamershock RA, Rajabiun S, Fox JE, Mofidi M, Abel SN, York JA, Kunzel C, Sanogo M, Mayfield TG. Dental students' HIV/AIDS-related knowledge, attitudes, and intentions: impact of the U.S. Health Resources and Services Administration's community-based dental partnership program. J Dent Educ 2014; 78: 1106-1117.
- Sadeghi M, Hakimi H. Iranian dental students' knowledge of and attitudes towards HIV/AIDS patients. J Dent Educ 2009; 73: 740-745.
- Rajabiun S, Fox JE, McCluskey A, Guevara E, Verdecias N, Jeanty Y, DeMayo M, Mofidi M. Patient perspectives on improving oral health-care practices among people living with HIV/AIDS. Public Health Rep 2012; 127: 73-81.
- Jeanty Y, Cardenas G, Fox JE, Pereyra M, Diaz C, Bednarsh H, Reznik DA, Abel SN, Bachman SS, Metsch LR. Correlates of unmet dental care need among HIV-positive people since being diagnosed with HIV. Public Health Rep 2012; 127: 17-24.
- Seacat JD, Litt MD, Daniels AS. Dental students treating patients living with HIV/AIDS: the influence of attitudes and HIV knowledge. J Dent Educ 2009; 73: 437-444.
- Kuthy RA, Heller KE, Riniker KJ, McQuistan MR, Qian F. Students' opinions about treating vulnerable populations immediately after completing community-based clinical experiences. J Dent Educ 2007; 71: 646-654.
- Volvovsky M, Vodopyanov D, Inglehart MR. Dental students and faculty members' attitudes towards care for underserved patients and community service: do community-based dental education and voluntary service-learning matter? J Dent Educ 2014; 78: 1127-1138.
- Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc 2013; 16: 18734.
- Corrigan PW, Larson J, Sells M, Niessen N, Watson AC. Will filmed presentations of education and contact diminish mental illness stigma? Community Ment Health J 2007; 43: 171-181.
- Oberoi SS, Marya CM, Sharma N, Mohanty V, Marwah M, Oberoi A. Knowledge and attitude of Indian clinical dental students towards the dental treatment of patients with human immunodeficiency virus (HIV)/acquired immune-deficiency syndrome (AIDS). Int Dent J 2014; 64: 324-332.
- Sollai S, Noguera-Julian A, Galli L, Fortuny C, Deya A, de Martino M, Chiappini E. Strategies for the prevention of mother to child transmission in Western countries: an update. Pediatr Infect Dis J 2015; 34: S14-30.
- 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric basic life support. Pediatrics 2006; 117: e989-1004.
- Blignaut E. The role of the dental profession in the AIDS epidemic. J Dent Assoc S Afr 1994; 49: 133-135.
- Ellepola AN, Joseph BK, Sundaram DB, Sharma PN. Knowledge and attitudes towards HIV/AIDS amongst Kuwait University dental students. Eur J Dent Educ 2011; 15: 165-171.
- Cleveland JL, Bonito AJ, Corley TJ, Foster M, Barker L, Gordon Brown G, Lenfestey N, Lux L. Advancing infection control in dental care settings: factors associated with dentists' implementation of guidelines from the Centers for Disease Control and Prevention. J Am Dent Assoc 2012; 143: 1127-1138.
- Pagliari AV, Garbin CA, Garbin AJ. HIV attitudes and practices among professors in a Brazilian dental school. J Dent Educ 2004; 68: 1278-1285.
- Li R, Dong W, He W, Liu Y. Chinese dental students' knowledge and attitudes toward HIV/AIDS. Journal of Dental Sciences 2016; 11: 72-78.