Case Report - Journal of Orthopedic Surgery and Rehabilitation (2023) Volume 7, Issue 5
Closed Tear of Both Flexor Tendons of the Middle Finger Following Oriental Hornet (Vespa Orientalis) Sting
Munteanu George Alexandru*, Shhade Mosa, Haim Katzevman, Daniel Dreyfuss, Dan HuttOrthopedic Surgery Division, Unit for Hand Surgery and Microsurgery, Rambam Healthcare Campus, Haifa, Israel
- *Corresponding Author:
- Munteanu George Alexandru
Orthopedic Surgery Division
Unit for Hand Surgery and Microsurgery
Rambam Healthcare Campus, Haifa, Israel
E-mail: alxmunt@gmail.com
Received: 24-Aug-2023, Manuscript No. AAOSR-23-113030; Editor assigned: 28-Aug-2023,PreQC No.AAOSR-23-113030(PQ); Reviewed: 11-sept-2023, QC No.AAOSR-23-113030; Revised: 16-sept-2023, Manuscript No.AAOSR-23-113030(R); Published: 22-sept-2023, DOI: 10.35841/ aaosr-7.5.163
Citation: Alexandru MG, Mosa S, Katzevman H, Dreyfuss D, Hutt D.Closed Tear of Both Flexor Tendons of the Middle Finger Following Oriental Hornet (Vespa Orientalis) Sting. J Ortho Sur Reh.2023;7(5):163
Abstract
This article is meant to raise awareness to the possibility of suffering a flexor tendon rupture after being stung by a hornet, as prevention is always better than dealing with the consequences of an injury. A tear of both flexors, described scarcely in the literature always poses an intriguing conundrum. We will describe a case we have dealt with and to our knowledge is the first of its kind.
Keywords
Flexor tendon tears, Oriental Hornet, Sting, Tendon reconstruction.
Introduction
Each digit, except the thumb, has two flexor tendons - one superficial, attaching to the base of the middle phalanx, and one deep, attaching to the base of the distal phalanx [1].
Avulsion of the Flexor Digitorum Profundus (FDP) is commonly referred to as Jersey Finger, an entity although quite uncommon but described extensively, usually affects the ring finger and involves a mechanism of hyperextension [2,3]. Isolated Flexor Digitorum Superficialis (FDS) tears are considered an even more rare entity [4].
The combined avulsion or tear of both tendons has been described even less, as mentioned in a recent article by Cuggy et al. - 14 cases of rupture of both tendons from their insertion were described since the first series in 1960 and 6 cases were reported of rupture in the mid substance of both tendons. All cases presented involved hyperextension injury or some sort of a blast injury causing these ruptures [5].
The case encountered by us involves tears in the middle finger of FDP (Zone 2) and FDS (Zone 3) which we postulate to have occurred after the patient was stung by a hornet in the hand, leading to a local inflammatory response [6-10], which combined with very mild trauma to the finger led to the complete rupture of both tendons.
Case report
A 61 year old, right hand dominant male presented to our outpatient clinics with complaints of inability to actively flex the middle finger of his right hand for about two weeks. He claimed to have sustained a mild trauma to finger and described it was squeezed between a cart and a wall. He did not pursue medical attention prior to the first visit in our clinic.
Clinical examination revealed an extended middle finger with no active flexion but with full passive flexion. There were no visible bruises but the finger was mildly swollen and tender to palpation on the volar aspect of the middle phalanx. Sensation and vascular tests were normal.
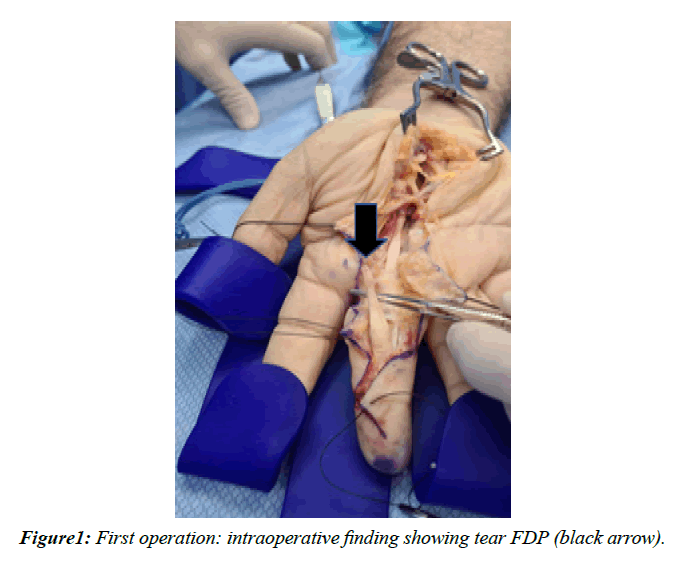
He went on to operation 3 days later. We used a standard Bruner incision, beginning most distally but having to extend it as much as the distal edge of the carpal tunnel due to the following intraoperative findings (Figure 1):
• Complete tear of FDP (ZONE 2) with distal stump found inside the A3P.
• Complete tear of FDS (ZONE 3) with distal stump found distal to the superficial vascular arch
• Proximal stumps found to be extremely friable and the lumbrical almost completely detached from the FDP.
• Extensive tenosynovitis along the course of both tendons with a lump of uncertain nature on top of the median nerve proximal to its exits from the carpal tunnel which was sent to pathology along with the distal stumps of both tendons.
As primary repair was not possible, we have decided to perform a 2-stage tendon reconstruction. We sutured a silicon rod to the shortened FDP distal stump and the skin was closed with interrupted nylon 4-0 sutures.
Postoperatively, upon further questioning and after describing the intraoperative findings, the patient recalled being stung by a hornet a few days before the above-mentioned trauma to the hand. This finding may explain the pathological results of the tissue sent which indicated extensive inflammatory reaction seen in the tissue sample sent.
The patient was referred to occupational therapy to begin treatment 3 days postoperatively.
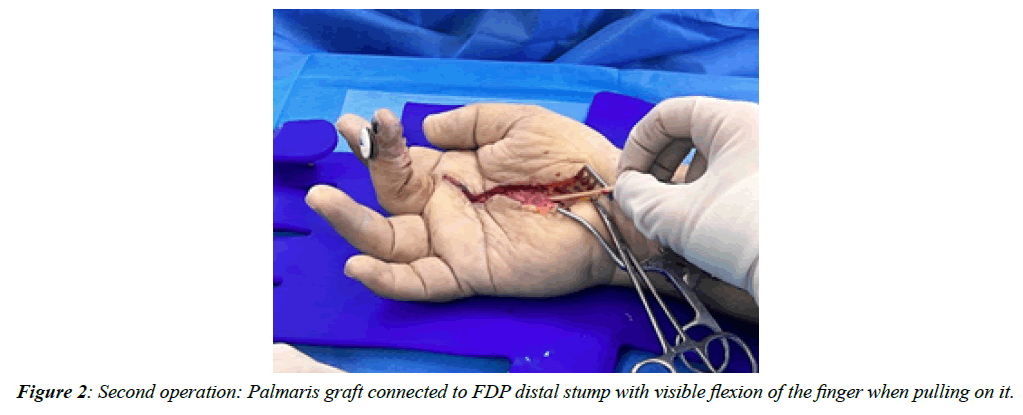
Following an uneventful period of around 3 months of intensive therapy the patient was examined in our clinic and was found to have good range of passive motion. He was then admitted and underwent the second stage of tendon reconstruction (Figure 2) using a Palmaris longus tendon graft which he now uses to flex his finger quite nicely.
Clinical Message
Tear of both flexor tendons resulting from extensive tenosynovitis that is secondary to acute inflammatory response may well have been prevented by splinting and/or means of reducing inflammation (Naiads, hand elevation, cooling). As it was not, we were still able to reconstruct one flexor tendon using the commonly described technique of 2 stage tendon repair.
Conclusion
This is a rare case of both flexor avulsions. The very low energy and unusual mechanism of injury described by the patient rose suspicion when first examined in our clinic and it is our belief that the main culprit in this matter are the toxins released by the hornet sting causing extensive tenosynovitis and weakening of the tendons to the point they rupture by very mild trauma. This in turn should be kept in mind when dealing with such injuries as it is possible that a few days of splinting in a safe position along with a course of anti-inflammatory medications may have prevented this awful tendon injury from the beginning.
Source of Finance- NIL
Consent-Patient consented to using his pictures
Competing Interests- Authors declare that there is no any competing interest.
Acknowledgements- NIL.
References
- Allan CH. Flexor tendons: Anatomy and surgical approaches. Hand Clin. 2005;21(2):151-7.
- Ruchelsman DE, Christoforou D, Wasserman B, et al. Avulsion injuries of the flexor digitorum Profundus tendon. J Am Acad Orthop Surg. 2011;19(3):152-62.
- Schöffl V, Heid A, Küpper T. Tendon injuries of the hand. World J Orthop. 2012;3(6):62.
- Schnebel BE, Flesher D, Garcia-Moral CA. Isolated traumatic avulsion of the flexor digitorum sublimes: A case report. Am J Sports Med. 1989;17(5):692-4.
- Cuggy C, Woods JF, Carr E, et al. Closed Traumatic Avulsion of Both Flexor Digitorum Tendons: An Addition to the Leddy and Packer Classification and Review of the Literature. J Hand Surg Am. 2022.
- Sawyer JR, Kellum EL, Creek AT, et al. Acute compartment syndrome of the hand after a wasp sting: A case report. J Pediatr Orthop B. 2010;19(1):82-5.
- Ruwanpathirana P, Priyankara D. Clinical manifestations of wasp stings: A case report and a review of literature. Trop Med Health. 2022;50(1):1-5.
- Moein P, Zand R. Cerebral infarction as a rare complication of wasp sting. J Vasc Interv Radiol. 2017; 9(4):13.
- Kumar V, Nada R, Kumar S, et al. Acute kidney injury due to acute cortical necrosis following a single wasp sting. Ren Fail. 2013;35(1):170-2.
- Petratos DV, Galanakos SP, Stavropoulos NA, et al. Late compartment syndrome of the hand due to wasp sting in a child. J Surg Orthop Adv. 2011;20(3):202-5.
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref