Research Article - Biomedical Research (2016) Volume 27, Issue 4
Clinical values of electrocardiogram (ECG) in diagnosing cardiac autonomic dysfunction
Yimeng Wang and Jinyi Xu*
Department of Electrocardiogram Room, Henan Provincial People’s Hospital, Zhengzhou 450000, PR China
- *Corresponding Author:
- Jinyi Xu
Department of Electrocardiogram Room, Henan Provincial People’s Hospital, Zhengzhou, China
Accepted on April 17, 2016
Abstract
This study aims to analyse the clinical efficacies of electrocardiogram (ECG) in diagnosing cardiac autonomic dysfunction (CAD) and to explore the clinical values of this method. A total of 82 CAD patients clinically diagnosed and confirmed were selected for the traditional Chinese medical treatment and psychological intervention. After three courses of treatment, their ECG were monitored, and the diagnostic results before and after the treatment were then compared. Before the treatment, the abnormality rate of the patients ECG diagnosis was 100%; while after the treatment, the rate was reduced to 10.98% (9/82). The intragroup comparison showed that the post-treatment abnormal ECG rate was significantly reduced and exhibited statistically significant difference with that before the treatment (P<0.05). Meanwhile, after the treatment, such clinical symptoms as palpitation, shortness of breath, or precordialgia were significantly improved, and the symptoms in 73 patients totally disappeared. The application of ECG in the clinical diagnosis of CAD was non-invasive and simple, and had high detection rate and accuracy; therefore, it had high clinical values and was suitable for wide promotion.
Keywords
Electrocardiogram, Clinical diagnosis, Cardiac autonomic dysfunction, Clinical value.
Introduction
Cardiac autonomic dysfunction (CAD) is the syndromes of cardiovascular dysfunction caused by the cardiac autonomic function disorders [1,2], though it does not belong to cardiac organic disease, its incidence has been significantly increased in recent years, and the incidence focuses in young adults at the age of 20 ~ 40 years old; the incidence in female is slightly higher than that in male. Because the clinical manifestations of CAD were palpitation, shortness of breath, and precordialgia [3], which were very similar to those of organic cardiac diseases, not only the difficulties of clinical diagnosis were increases, but also the patients would have more psychological burdens because of the doubts about the disease, and these were not conducive to the treatment of CAD [4]. Dynamic electrocardiogram (ECG) could diagnose CAD accurately and simply [4]. In order to accurately diagnose CAD and perform the symptomatic treatment as early as possible, we sampled 82 CAD patients to analyse the diagnostic values of their ECG results, and the study was reported below.
Materials and Methods
General information
A total of 82 CAD patients clinically diagnosed and confirmed in our hospital from January 2013 to January 2015 were selected. All the 82 patients met the following inclusion criteria: 1). had different degrees of palpitation, shortness of breath, and precordialgia, and these symptoms lasted for >150 days [2]; 2). Between 20 and 40 years old; 3). ECG results revealed abnormalities of ST wave band, T wave, and heart rate variability. Meanwhile, through blood routine, urine routine, and hepatonephric function examinations, patients with heart diseases, myocarditis, and diabetes were excluded [3]. Among the 82 qualified patients selected, 35 were males and 47 were females, with the average age as (32.6 ± 3.2) years (Table 1). This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Henan Provincial People’s Hospital. Written informed consent was obtained from all participants.
| S.No. | Gender | Age | Type of abnormality in this monitoring | Symptoms disappeared completely |
|---|---|---|---|---|
| 1 | male | 33 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 2 | male | 37 | Supraventricularextrasystole and emergency ventricular extrasystole | Yes |
| 3 | male | 32 | Complex heart rhythm abnormality | Yes |
| 4 | male | 36 | Multiple ventricular extrasystole | Yes |
| 5 | male | 29 | Multiple ventricular extrasystole | Yes |
| 6 | male | 29 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 7 | male | 36 | Supraventricularextrasystole and emergency ventricular extrasystole | Yes |
| 8 | male | 33 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 9 | male | 32 | Complex heart rhythm abnormality | No |
| 10 | male | 36 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 11 | male | 26 | Multiple ventricular extrasystole | Yes |
| 12 | male | 29 | Multiple ventricular extrasystole | Yes |
| 13 | male | 35 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 14 | male | 36 | Multiple ventricular extrasystole | Yes |
| 15 | male | 35 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 16 | male | 34 | Multiple ventricular extrasystole | No |
| 17 | male | 35 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 18 | male | 32 | Multiple ventricular extrasystole | Yes |
| 19 | male | 29 | Multiple ventricular extrasystole | Yes |
| 20 | male | 28 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 21 | male | 28 | Multiple ventricular extrasystole | No |
| 22 | male | 37 | Complex heart rhythm abnormality | Yes |
| 23 | male | 30 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 24 | male | 35 | Atrioventricular conduction disorder | Yes |
| 25 | male | 36 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 26 | male | 30 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 27 | male | 32 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 28 | male | 33 | Multiple ventricular extrasystole | Yes |
| 29 | male | 28 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 30 | male | 32 | Multiple ventricular extrasystole | Yes |
| 31 | male | 30 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 32 | male | 28 | Multiple ventricular extrasystole | Yes |
| 33 | male | 38 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 34 | male | 36 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 35 | male | 36 | Complex heart rhythm abnormality | Yes |
| 36 | female | 36 | Supraventricularextrasystole andemergency ventricular extrasystole | Yes |
| 37 | female | 28 | Supraventricularextrasystole andemergency ventricular extrasystole | No |
| 38 | female | 29 | Multiple ventricular extrasystole | Yes |
| 39 | female | 36 | Supraventricularextrasystole and emergency ventricular extrasystole | Yes |
| 40 | female | 32 | Multiple ventricular extrasystole | Yes |
| 41 | female | 37 | Normal | Yes |
| 42 | female | 32 | Supraventricularextrasystole and emergency ventricular extrasystole | Yes |
| 43 | female | 28 | Atrioventricular conduction disorder | Yes |
| 44 | female | 29 | Multiple ventricular extrasystole | Yes |
| 45 | female | 28 | Atrioventricular conduction disorder | Yes |
| 46 | female | 36 | Supraventricularextrasystole and emergency ventricular extrasystole | Yes |
| 47 | female | 33 | Supraventricularextrasystole and emergency ventricular extrasystole | Yes |
| 48 | female | 29 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 49 | female | 35 | Complex heart rhythm abnormality | Yes |
| 50 | female | 32 | Normal | Yes |
| 51 | female | 29 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 52 | female | 29 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 53 | female | 35 | Multiple ventricular extrasystole | Yes |
| 54 | female | 35 | Multiple ventricular extrasystole | Yes |
| 55 | female | 37 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 56 | female | 38 | Multiple ventricular extrasystole | Yes |
| 57 | female | 36 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 58 | female | 30 | Multiple ventricular extrasystole | Yes |
| 59 | female | 32 | Multiple ventricular extrasystole | No |
| 60 | female | 36 | Multiple ventricular extrasystole | Yes |
| 61 | female | 35 | Supraventricular extrasystole and emergency ventricular extrasystole | No |
| 62 | female | 30 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 63 | female | 31 | Complex heart rhythm abnormality | Yes |
| 64 | female | 32 | Multiple ventricular extrasystole | Yes |
| 65 | female | 32 | Complex heart rhythm abnormality | Yes |
| 66 | female | 28 | Atrioventricular conduction disorder | Yes |
| 67 | female | 35 | Multiple ventricular extrasystole | Yes |
| 68 | female | 32 | Normal | Yes |
| 69 | female | 26 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 70 | female | 36 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 71 | female | 32 | Multiple ventricular extrasystole | No |
| 72 | female | 34 | Multiple ventricular extrasystole | No |
| 73 | female | 37 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 74 | female | 33 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 75 | female | 28 | Normal | Yes |
| 76 | female | 35 | Multiple ventricular extrasystole | Yes |
| 77 | female | 33 | Multiple ventricular extrasystole | Yes |
| 78 | female | 35 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 79 | female | 36 | Supraventricular extrasystole and emergency ventricular extrasystole | No |
| 80 | female | 30 | Atrioventricular conduction disorder | Yes |
| 81 | female | 32 | Supraventricular extrasystole and emergency ventricular extrasystole | Yes |
| 82 | female | 31 | Normal | Yes |
Table 1. General information of patients and some results in this study.
ECG diagnosis
All the patients were performed 24 h dynamic ECG monitoring twice after admission (model: MSLVE02, manufacturer: Guangzhou Yilujiuge Co., China), and were recorded the detailed monitoring results.
Treatment methods
The main treatment was psychotherapy, aiming to eliminate the patient's fear and pressure. Meanwhile, necessary medical treatment was supplemented according to the principles of reinforcing Heart and tranquilization; the traditional Chinese medicine Ganmai dazao decoction was used for the treatment, with 10 days as a course for three courses [5].
Dynamic ECG monitoring
At the end of the three treatment courses, dynamic ECG monitoring was performed three times, and the duration should be >20 h; the ECG monitoring results were recorded.
Observation indexes
The abnormal indexes before the treatment and at the end of the 3rd ECG monitoring were observed to compare the abnormality rates. Meanwhile, the changes of clinical symptoms before and after the treatment were observed and compared.
Statistical analysis
SPASS 17.0 software was used for the data analysis; the
counting data were expressed as% and performed the χ2 test; the measurement data were expressed as mean ± standard
deviation (![]() ± s) and performed the t-test, with P<0.05
considered as statistically significant difference.
± s) and performed the t-test, with P<0.05
considered as statistically significant difference.
Results
Results of 24h dynamic ECG monitoring
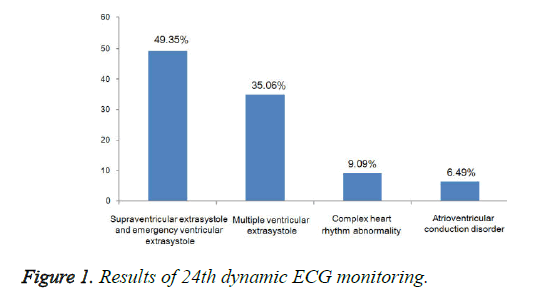
There were 77 cases of cardiac index abnormality in this monitoring, including 32 males and 45 females; there was no statistically significant difference in the detection rate between the genders (P>0.05). Among these cases, 38 cases were supraventricular extrasystole and emergency ventricular extra systole, accounting for 49.35%; 27 cases were multiple ventricular extra systole, accounting for 35.06%; seven cases were complex heart rhythm abnormality, accounting for 9.09%; five cases were atrioventricular conduction disorder, accounting for 6.49% (Table 1, Figure 1).
Abnormality rate of ECG
Before the treatment, all the 82 patients exhibited ECG abnormality, with the abnormality rate as 100%. After the treatment, only nine patients showed abnormal ECG, with the abnormality rate as 10.98%. The intragroup comparison showed that the post-treatment abnormal ECG rate was significantly reduced and exhibited statistically significant difference with that before the treatment (χ2=12.6968, P=0.0004<0.05) (Table 2).
| Before the treatment | After the treatment | Statistical result | |
|---|---|---|---|
| The normality rate | 0% (n=0) | 89.02% (n=73) | χ2=12.6968, P=0.0004 |
| The abnormality rate | 100% (n=82) | 10.98% (n=9) |
Table 2. Abnormality rate of ECG between before the treatment and after the treatment.
Changes of clinical symptoms
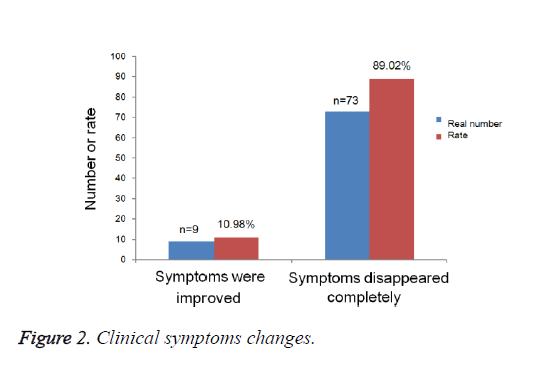
After the treatment, such clinical symptoms as palpitation, shortness of breath, and precordialgia in this study were significantly improved. Of these, the symptoms in 73 patients disappeared completely, and the clinical improvement rate was 89.02% (Table 1, Figure 2).
Discussion
The syndromes of cardiovascular dysfunction caused by the autonomic dysfunction while without heart organic disease are named CAD [6,7]. With the accelerated pace of life and the gradually increased pressure, the incidence of ACD is continuously increased and shows the trend towards younger adults; women between 20 and 40 years has become the highrisk population of CAD [8,9]. This study investigated the clinical values of ECG in diagnosing CAD, aiming to lay solid foundations for further clinical diagnostic work.
Because CAD belongs to a kind of psychological illness, so the focus of clinical treatment should be put onto caring the patient's psychological problems. But from the current status of the clinical treatments of CAD, it was usually treated as the diseases of the cardiovascular system, so many doctors just treated the clinical symptoms while did not care about the psychological status of the patients [10-12] or this issue had not caused sufficient attention, so it would easily lead to repeated medical treatment, which not only was a waste of medical resources but also would increase the economic and psychological pressure of the patients.
From the pathogenesis of CAD, fast pace of life, lack of sleep, or too much pressure were important factors towards the occurrence of CAD [13,14]. Under the joint effects of these factors, the body's sympathetic nerve and autonomic nerve might difficultly maintain the balance, so it would be easy to result in the dysfunction. Palpitation, shortness of breath, and precordialgia are the main clinical manifestations of CAD; meanwhile, patients might produce intense and other negative emotions because of pain, which virtually increased the psychological pressure of patients [15]. and would have some impacts on their normal work and lives.
Currently, there is still lack of unified and standard diagnostic criteria towards CAD, and what detection method should be used to confirm this issue is still a big controversy among medical fields. Based on this situation, we mainly used the symptom diagnosis and exclusion diagnosis to confirm the diagnosis. Dynamic ECG monitoring is simple and noninvasive, and could be easily accepted by patients; therefore, it could be used as the diagnostic evidence of CAD. In addition, other examination methods such as patient’s medical history, enzymology, ultrasound, or x-rays could be combined for the comprehensive judgment and correct diagnosis, which could then eliminate patient’s psychological fear of heart disease, improve the mental condition, facilitate physicians to achieve symptomatic treatment, and make the patient recovered as soon as possible [16,17].
Because ECG was the main signal detection way for heart diseases, which could quickly and accurately capture the instantaneous heart rate changes and waveform abnormalities [18,19], it could provide certain basis for the diagnose of CAD. This study investigated the clinical significance of ECG in diagnosing CAD.
The twice 24 h dynamic ECG monitoring towards the 82 patients revealed that a total of 77 patients exhibited abnormal heart rate indexes and waveforms, with a little higher abnormality rate as 93.9%. The abnormality rates in ST wave band or T wave were higher, and most of them appeared when the heart rate increased, so the frequency of the abnormality rate was positively correlated with the heart rate. Meanwhile, comparing the ECG monitoring results before and after the treatment revealed that the post-treatment abnormality rate was significantly reduced than that before the treatment, and the difference was statistically significant (P<0.05). In addition, after the treatment, such clinical symptoms as palpitation, shortness of breath, or precordialgia were significantly improved, and the symptoms in 73 patients totally disappeared; the clinical improvement rate was 89.02%. These results fully demonstrated that the clinical data of dynamic ECG could be used as the diagnostic evidence of CAD, consistent with Corazza et al. [20], indicating that ECG had high clinical values in diagnosing CAD. In summary, the application of ECG in clinically diagnosing CAD was non-invasive and simple, and had high detection rate and accuracy; therefore, it had high clinical values and was suitable for wide promotion.
References
- Bar KJ. Cardiac Autonomic Dysfunction in Patients with Schizophrenia and Their Healthy Relatives - A Small Review. Front Neurol 2015; 6: 139.
- Hess P, Lomonosov AM. Solitary surface acoustic waves and bulk solitons in nanosecond and picosecond laser ultrasonics. Ultrasonics 2010; 50: 167-171.
- Navarrete M, Godinez FA, Villagran-Muniz M. Elastic properties of compacted clay soils by laser ultrasonics. Int J Ther 2013; 34: 1810-1816.
- Brander A, Viikinkoski P, Tuuhea J, Voutilainen L, Kivisaari L. Clinical versus ultrasound examination of the thyroid gland in common clinical practice. J Clin Ultrasound 1992; 20: 37-42.
- Erickson RA, Tretjak Z. Clinical utility of endoscopic ultrasound and endscopic ultrasound-guided fine needle aspiration in retroperitoneal neoplasms. Am J Gastroenterol 2000; 95: 1188-1194.
- Slyper AH. Clinical review 168: What vascular ultrasound testing has revealed about paediatric atherogenesis, and a potential clinical role for ultrasound in paediatric risk assessment. J Clin Endocrinol Metab 2004; 89: 3089-3095.
- Sheiner E, Shoham-Vardi I, Abramowicz JS. What do clinical users know regarding safety of ultrasound during pregnancy? J Ultrasound Med 2007; 26: 319-325.
- Smith HM, Duncan CM, Hebl JR. Clinical utility of low-volume ultrasound-guided interscalene blockade: contraindications reconsidered. J Ultrasound Med 2009; 28: 1251-1258.
- Chen K, Lee HS, Chandrakasan AP, Sodini CG. Ultrasonic Imaging Transceiver Design for CMUT: A Three-Level 30-Vpp Pulse-Shaping Pulser with Improved Efficiency and a Noise-Optimized Receiver. IEEE J Solid-State Circuits 2013; 48: 2734-2745.
- Roitner H, Bauer-Marschallinger J, Berer T, Burgholzer P. Experimental evaluation of time domain models for ultrasound attenuation losses in photoacoustic imaging. J Acoust Soc Am 2012; 131: 3763-3774.
- Adler DD, Carson PL, Rubin JM, Quinn-Reid D. Doppler ultrasound color flow imaging in the study of breast cancer: preliminary findings. Ultrasound Med Biol 1990; 16: 553-559.
- Fukami T, Emoto M, Tamura R. Sonographic findings of transvaginal color Doppler ultrasound in ectopic pregnancy. J Ultrasound Med 2006; 33: 37-42.
- Albrecht H, Stroszczynski C, Felix R, Hünerbein M. Real Time 3D (4D) Ultrasound-Guided Percutaneous Biopsy of Solid Tumours. Ultraschall Med 2006; 27: 324-328.
- Liu CX, Gao XS, Xiong LL, Ge HY, He XY, Li T, Zhang HJ, Bai HZ, Lin Q, Zhang M, Zhao J, Xiong W, Bai Y, Asaumi J. A preclinical in vivo investigation of high-intensity focused ultrasound combined with radiotherapy. Ultrasound Med Biol 2011; 37: 66-77.
- Peng C, Yang K, Xiang P, Zhang C, Zou L, Wu X, Gao Y, Kang Z, He K, Liu J, Cheng M, Wang J, Chen L. Effect of transplantation with autologous bone marrow stem cells on acute myocardial infarction. Int J Cardiol 2013; 162: 158-165.
- Keeling AN, Carr JC, Choudhury L. Right ventricular hypertrophy and scarring in mutation positive hypertrophic cardiomyopathy. Eur Heart J 2010; 31: 381.
- Hahn H, Macdonald E, Steinbom M. Sonographic detection of normal appendix in children and adolescents. Ultraschall Med 2008; 29: 281-285.
- Ricci P, Cantisani V, Ballesio L, Pagliara E, Sallusti E, Drudi FM, Trippa F, Calascibetta F, Erturk SM, Modesti M, Passariello R. Benign and malignant breast lesions: efficacy of real time contrast-enhanced ultrasound vs. magnetic resonance imaging. Ultraschall Med 2007; 28: 57-62.
- Madjar H, Becker S, Doubek K, Horchler T, Mendoza M, Moisidis-Tesch C, Näther B, Niebling K, Pröls U, Schardt AR, Ulrich S, Zahn U. Impact of breast ultrasound screening in gynecological practice. Ultraschall Med 2010; 31: 289-295.
- Corazza I, Barletta G, Guaraldi P, Cecere A, Calandra-Buonaura G, Altini E, Zannoli R, Cortelli P. A new integrated instrumental approach to autonomic nervous system assessment. Comput Methods Programs Biomed 2014; 117: 267-276.