- Biomedical Research (2014) Volume 25, Issue 4
Clinical study of RDW and prognosis in sepsis new borns.
Jianping Chen*, Ling Jin and Tong YangDepartment of Pediatrics, Liuzhou People’ Hospital, Liuzhou, Guangxi 545006, China
- *Corresponding Author:
- Jianping Chen
Department of Pediatrics
Liuzhou People’ Hospital, No. 8Wenchang Road
Liuzhou, Guangxi 545006, China
Accepted date: July 01 2014
Abstract
Aims of the present study were to investigate the relationship between red blood cell volume distribution width (RDW) and severity of the disease with prognosis in sepsis newborns. RDW, clinical features and prognosis in 97 sepsis newborns were analyzed retrospectively. Fifity-eightsepsis newborns showed increase of RDW with the incidence of 59.79%, including 13 cases from sepsis group, 23 cases from severe sepsis group and 22 cases from septic shock group (the same order below), with the incidence of RDW increase of 31.71%, 76.67% and 84.62%, respectively, and the differences were significantly significant (P<0.001). The mortalities of the three groups were 15.38%, 39.13% and 50.00%, respectively, and there were not statistically differences (P>0.05). The incidence of RDW increase in survival group (49.32%) was significantly lower than that in the death group (91.67%). The neonatal critical illness score (NCIS) was negatively correlated with RDW increase in newborns, while the mortality was positively correlated with RDW increase (P<0.001). RDW increase in newborns with severe sepsis and septic shock has a higher incidence, and the level of RDW increase is closely associated with the prognosis.
Keywords
sepsis, shock, red blood cell volume distribution width, newborns, prognosis
Introduction
Red blood cell distribution width (RDW) is a parameter reflecting the heterogeneity of the peripheral red blood volume and is usually expressed withRDW-coefficient of variation (RDW-CV). In clinic, it can be understood whether the size of red blood cell volume is uniform through detection of RDW. The more RDW is, the more uneven the red blood cell size is, and the higher the volume heterogeneity is. Recent studies found that RDW can takenas a “marker” of death in critical patients and can be used independently to predict the risk of death in critical patients [1]. Sepsis is a common critical illness in department of pediatrics and can cause a high lethality. In order to discuss the relationship between RDW and prognosis in sepsis newborns, the relationship between RDW and severity of the condition with prognosis in sepsis newborns who were admitted into our hospital from January 2008 to December 2013 were analyzed retrospectively in the present study, providing a reference for clinical treatment and prognosis evaluation.
Materials and Methods
All sepsis newborns who were admitted into neonatal intensive care unit (NICU) of our hospital from Jan. 2008 to Dec. 2013 were included in the study, and sepsis was diagnosed based on the standard formulated by the International Joint Conference of Pediatric Sepsis [2]. Exclusion criteria: a. the premature infants, b. newborns suffering fromsevere asphyxia at birth, c. those who were being treated with chalybeate. Ninety-seven patients (60 males and 37 females, mean gestational age: 38.97±1.31 weeks) were selected. The primary diseases included respiratory diseases in 52 cases, nervous system disease in 17 cases, cardiovascular disease in 11 cases, digestive system disease in 8 cases, urinary system disease in 3 cases and other diseases in 3 cases.
Ninety-seven sepsis newborns were divided into sepsis group, severe sepsis group (no shock) and septic shock group according to the severity of the disease, the standard formulated by the International Joint Conference of Pediatric Sepsis [2] and the Recommended Program for Treatment of Pediatric Infectious Shock (septic shock) by Chinese Medical Association [3]. There were not statistical differences in the general condition among the three groups, including gender, gestational age, birth weight, Apgar scores at 1 min and 5 min after birth and absence and presence of cesarean delivery. According to RDW values measured on the day in the newbornswho were confirmed to have sepsis (normal value: 13%~18% [4]), the enrolled newborns were divided into normal RDW group (including those in whom RDW was lower than that in normal newborns) and increased RDW group.
SYSMEX-2100 automatic blood cell analyzer was used.
The grading was performed based on the condition: score > 80, 80~71 and ≤70 indicated that the condition is noncritical, critical and extremely critical, respectively (i.e., the lower the score of NCIS is, the more critical the condition is)[5].
SPSS 15.0 was adopted for statistical analysis. The obtained measurement data in line with the normal distribution were expressed as mean ± standard deviation, and the skewed distribution was described with the median (interquartile range). Analysis of variance was used for comparison of mean value of the measurement data in line with the normal distribution among groups, and t test was employed for comparison of mean value between two groups. χ2 testwas used for intergroup compassion of count data. Linear correlation analysis was adopted for test of the relationship between PCIS score and RDW, and rank correlation analysis was employed for test of the relationship between RDW and mortality. Two-sided test was also used, and α=0.05 was the standard for test of significance. P<0.05 was considered statistically significant.
Results
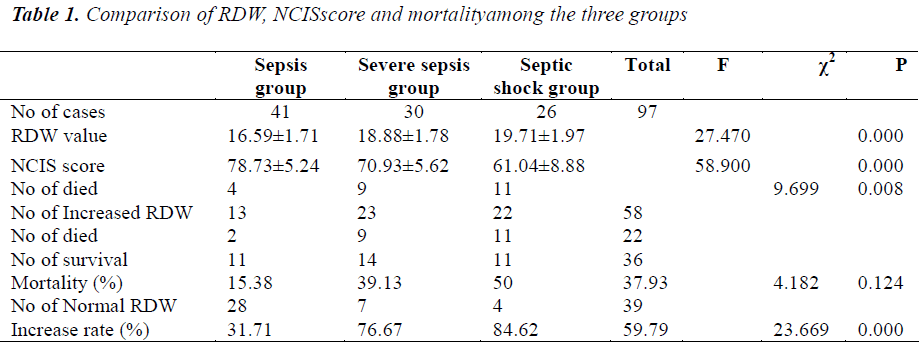
A total of 97 newborns were enrolled in the study, including 41 cases from sepsis group, 30 cases from severe sepsis group and 26 cases from septic shock group. In all the cases, 73 cases survived and 24 cases died. Fifty-eight newborns showed RDW increase and accounted for 59.79% (58/97). There were statistical differences in RDW among sepsis, severe sepsis and septic shock group (P=0.000). Moreover, a statistical difference also existed in RDW between sepsis and severe sepsis group, severe sepsis and septic shock group as well as sepsis and septic shock group (P=0.000). See Table 1.
Comparison of the incidence of RDW increase and the mortality: among 97 sepsis newborns, 58 cases exhibited RDW increase, accounting for 59.79%;23 of 30 newborns with severe sepsis had RDW increase, accounting for 76.67%; 22 of 26 newborns with septic shock showed RDW increase, accounting for 84.62%. The incidences of RDW increase were significantly different among the sepsis, severe sepsis and septic shock group (χ2=23.669, P=0.000). See Table 1. The mortalities in newborns with RDW increase from sepsis, severe sepsis and septic shock group were 15.38% (2/13), 39.13% (9/23) and 50.00% (11/22), respectively, and the results showed that the difference was not statistically significant (χ2=4.182, P>0.05)(See Table 1).
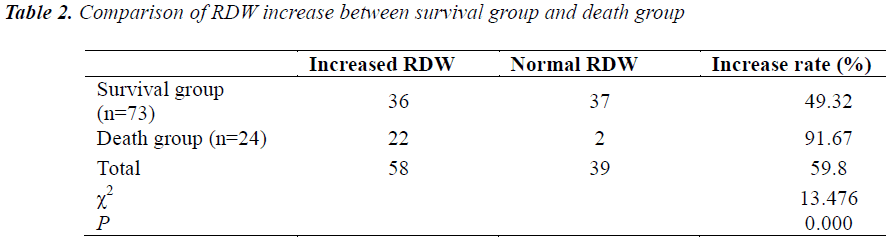
RDW increase and prognosis: among 97 newborns with sepsis/severe sepsis/septic shock, 73 cases survived, of whom, 36 cases showed RDW increase (49.32%), and 24 cases died, of whom, 22 cases had RDW increase (91.67%). There were statistical differences in RDW increase between the two groups (χ2=13.476, P=0.000)(See Table 2). Rank correlation analysis was performed for test of the relationship between RDW and mortality, and the results found that the mortality was positively correlated with RDW values (r=0.343, P=0.001).
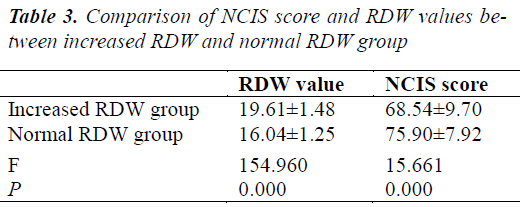
RDW and severity of the disease: RDW value of RDW increase group (19.61±1.48) was higher than that of normal RDW group (16.04±1.25), and there was a statistical difference (F=15.661, P=0.000). NCIS score of RDW increase group (68.54±9.70) was lower than that of normal RDW group (75.90±7.92), and there was a statistical difference (F=15.661, P=0.000) (See Table 3).Correlation analysis was adopted for test of the relationship between RDW and NCIS score, and the results showed that RDW values were negatively correlated with NCIS scores (r=-0.568, P=0.000).
Discussion
Sepsis is an infection-induced systemic inflammatory response syndrome and can further progress to severe sepsis, septic shock and multiple organ dysfunction syndrome or multiple organ failure. It is a common critical illness in department of pediatrics and one of the main causes of death in critical children. Epidemiologic data in USA showed that the mortality of children with severe sepsis was 10.3%, which can be up to 12.8% in children suffering from underlying diseases [6]. Early identification and timely treatment of sepsis in children is particularly critical in reducing the mortality. New studies found that RDW increase can be used as an important and independent predictive factor of the incidence of deaths caused by various diseases. Meanwhile, RDW values can reflect the degree of overall inflammation and oxidative stress[1,7]. Luo et al. at home found that RDW can predict the prognosis of critical patients [8]. Although the exact mechanism of the correlation between RDW and mortality of sepsis children is unclear, it may involve the changes of red cell balance caused by the body’s inflammatory response and oxidative stress [9]. Increased RDW may comprehensively reflect the following pathophysiological mechanisms in occurrence and development of sepsis: a) inflammation may cause an increase of neurohormone and endocrine hormone in the body including noradrenaline, angiotensin ı and other angiotensins level and renal ischemia. These neurotransmitters can stimulate red blood cell proliferation through promoting the generation of erythrogenin (EPO) to result in RDW increase [10]. b) Inflammatory factors may affect marrow hemopoietic function and iron metabolism in the body [11] to cause RDW increase [12]. c) RDW increase may indicate instable cytomembrane which may cause multiple organ dysfunctions to make the patients’ condition deteriorate, thus leading to poor prognosis and increased mortality. Studies found that, the materials providing the nutrition to the body and cell, such as blood cholesterol, albumin and others, are also lack while RDW increases. Therefore, increased RDW may reflect the cell membrane instability due to the lack of cholesterol and other substances in the body [13,14]. d) Severe sepsis /septic shock may be combined with multiple organ dysfunction. The study by Lippi et al. [15] showed that glomerular filtration rate (GFR) decreased progressively with increasing of RDW, and gastrointestinal dysfunction and liver function impairment may cause dysfunction of digestion and absorption to induce megaloblastic anemia or microcytic hypochromic anemia. Therefore, increase of RDW may reflect unevenness of red cell size due to liver function impairment- induced lack of hematopoietic elements (e.g., iron, folic acid, vitamin B12) in the body. A single or combined effect of the adverse factors above both can cause RDW increase, and RDW increase in sepsis newborns is likely caused by the combined action of several adverse factors.
From the data of this study,the incidence of RDW increase in sepsis newborns was 59.79% and was increasing with increase of the severity of the disease, and the incidence of RDW increase in severe sepsis newborns was 31.71% while this value in newborns with septic shock was up to 84.62%. Although the difference in the mortality of the newborns with RDW increase among the three groups was not statistically significant, the mortality of newborns with RDW increase in septic shock group was up to 50.00% which was higher than that in sepsis group (15.38%). RDW in newborns of the death group was significantly higher than that of the survival group, and the incidence of RDW increase was also higher than that of the survival group. NCIS score in newborns with RDW increase was lower than that in newborns with normal RDW.The higher RDW value was and the lower NCIS score was, the more serious the disease was and the worse the prognosis was, that is, a negative correlation existed between them. Some studies found NCIS score was one of the risk factors of death in sepsis newborns [16,17]. Therefore, NCIS score combined with RDW values of newborns can be taken as an important indicator of the prognosis in sepsis newborns.
RDW may become a new indicator for prognostic evaluation and risk stratification in sepsis newborns due to simple and easy detection, required lower expense, easilyrepeated measurement and convenient monitoring of outcome [18]. In addition, an in-depth discussion of the relationship between RDW and sepsis can make us have a better exploration of the relevant physiopathologic mechanism from a new aspect, to look for the new treatment methods which can block the progressive development of sepsis into severe sepsis/septic shock, thus further reducing further the mortality of such newborns. Thus, RDW may be used an ideal predictive value for evaluation of sepsis risk and prognosis and used to evaluate the prognosis of sepsis newborns. Therefore, it is worthy of clinical application and has an extremely clinical application value.
References
- Hunziker S, Stevens J, Howell MD. Red cell distribution width and mortality in newly hospitalized patients. Am J Med 2012; 125: 283-291.
- Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 2005; 6: 2-8.
- Group of Emergency Medicine CPS, Chinese Medical Association, Group of Pediatrics CSoEM, Chinese Medical Association, Pediatrics EBoCJo. Recommended protocol for diagnosis and treatment of septic shock in children. J Clin Pedi 2006; 44: 596-598.
- Huang SL. Handbook of Pediatric Hematology. Beijing: People's Medical Publishing House, 2000.
- Song GW. Journal of Emergency Medicine. Chin J Emer Med 2003; 12: 359-360.
- Watson RS, Carcillo JA. Scope and epidemiology of pediatric sepsis. Pediatr Crit Care Med 2005; 6: S3-5.
- Bazick HS, Chang D, Mahadevappa K, Gibbons FK, Christopher KB. Red cell distribution width and allcause mortality in critically ill patients*. Critical care medicine 2011; 39: 1913-1921.
- Luo YJ, Zhou CY, Lou CL. Evaluation value of red cell volume distribution width on the prognosis of the critical patients. Chin J Crit Care Med 2012; 32: 355-357.
- Perlstein TS, Weuve J, Pfeffer MA, Beckman JA. Red blood cell distribution width and mortality risk in a community-based prospective cohort. Archives of Internal Medicine 2009; 169: 588-594.
- Špinarová L, Toman J, Pospı́šilová J, Souĉek M, Kára T, Štejfa M. Humoral response in patients with chronic heart failure. International journal of cardiology 1998; 65: 227-232.
- Chiari MM, Bagnoli R, De Luca P, Monti M, Rampoldi E, Cunietti E. Influence of acute inflammation on iron and nutritional status indexes in older inpatients. Journal of the American Geriatrics Society 1995; 43:767-771.
- Förhécz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohászka Z, Jánoskuti L. Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. American heart journal 2009; 158: 659-666.
- Chen P-C, Sung F-C, Chien K-L, Hsu H-C, Su T-C, Lee Y-T. Red blood cell distribution width and risk of cardiovascular events and mortality in a community cohort in Taiwan. American journal of epidemiology 2010; 171: 214-220.
- Pascual-Figal DA, Bonaque JC, Redondo B, Caro C, Manzano-Fernandez S, Sanchez-Mas J, et al. Red blood cell distribution width predicts long-term outcome regardless of anaemia status in acute heart failure patients. Eur J Heart Fail 2009; 11: 840-846.
- Lippi G, Targher G, Montagnana M, Salvagno GL, Zoppini G, Guidi GC. Relationship between red blood cell distribution width and kidney function tests in a large cohort of unselected outpatients. Scandinavian Journal of Clinical & Laboratory Investigation 2008; 68: 745-748.
- Liu J, Qian SY. A single-center investigation of the morbidity of pediatric sepsis and severe sepsis. J Clin Pedi 2010; 28: 26-29.
- Niu ZM, Li YH. Survival analysis of 205 children with sepsis. J Clin Pedi 2012; 30: 18-21.
- Garofoli F, Ciardelli L, Mazzucchelli I, Borghesi A, Angelini M, Bollani L, et al. The red cell distribution width (RDW): Value and role in preterm, IUGR (intrauterine growth restricted), full-term infants. Hematology 2013;