Research Article - Biomedical Research (2017) Artificial Intelligent Techniques for Bio Medical Signal Processing: Edition-I
Clinical study of acupuncture of yanglingquan point for the treatment of HFS
Zhou Kelin*, Shen LeiLongkuang Central Hospital of Longkou, Beijing University of Chinese Medicine, Beijing, PR China
- *Corresponding Author:
- Zhou Kelin
Longkuang Central Hospital of Longkou
Beijing University of Chinese Medicine
Beijing, PR China
Accepted date: January 15, 2017
Abstract
Objective: To investigate the therapeutic efficacy of acupuncture of Yanglingquan point for the treatment of hemifacial spasm (HFS).
Methods: A total of 60 patients with HFS collected clinically were randomly assigned to the experimental group and the control group. Acupuncture of Yanglingquan point was performed in the experimental group, while injection of vitamin B12 was conducted at the acupoint in the control group.
Results: The response rates in the experimental group and the control group were 96.7% and 56.7%, respectively, with a significant difference between the two groups.
Keywords
Acupunture, Yanglingquan, HFS.
Introduction
HFS is a common clinical disease as well as one of the recurring diseases clinically [1]. It is manifested as irregular spasm of facial muscles, which usually involves the mouth and cheeks and sometimes the eyelids and corners of eyebrows, etc. Such symptoms as spasm of lateral muscles and difficulties in opening eyes may occur. Some of the HFS treatments are investigated such as botulinum toxin injections [2,3], microvascular decompression [4,5] and carotid artery [6]. Herein we collected 60 patients with HFS admitted as the clinical outpatients from June, 2010 to September, 2015, and they were randomly divided into two groups, with 30 patients in the experimental group and the control group, respectively.
Clinical Data
General data of clinical patients
The 60 patients we collected included 30 males and 30 females aged 23 to 57 years. They had disease duration of 1 month to 2 years, and they were randomly assigned to two groups.
Determination of the degree of spasm: Grade I: Increased blink reflex induced by external stimulus; Grade II: Visible; Grade III: Moderate, significant spasm; Grade IV: Severe, severe spasm, uncontrollable (Tables 1 and 2).
| Site | Grade I | Grade II | Grade III | Grade IV | Total |
|---|---|---|---|---|---|
| Eye spasm | 4 | 9 | 17 | 0 | 30 |
| Facial spasm | 5 | 14 | 11 | 0 | 30 |
| Lateral spasm | 17 | 9 | 4 | 0 | 30 |
| Neck spasm | 0 | 0 | 0 | 0 | 0 |
Table 1: Disease conditions of the experimental group before the treatment.
| Site | Grade I | Grade II | Grade III | Grade IV | Total |
|---|---|---|---|---|---|
| Eye spasm | 7 | 12 | 11 | 0 | 30 |
| Facial spasm | 15 | 13 | 2 | 0 | 30 |
| Lateral spasm | 15 | 9 | 3 | 0 | 27 |
| Neck spasm | 0 | 0 | 0 | 0 | 0 |
Table 2: Disease conditions of the control group before the treatment.
Exclusion criteria of patients
Patients who did not meet the above criteria, who could not receive treatment persistently and who could not promise not to accept any treatment in addition to this one were excluded.
Treatment Methods
Experimental group
Acupoint selection: The contralateral Yanglingquan point of the lesions was used. The Yanglingquan point is located at the depression below the anterior fibular head of the lateral calf, and its anatomical levels are skin, subcutaneous tissue, deep fascia of calf, peroneus longus and peroneus brevis. The lateral sural cutaneous nerves are distributed in the shallow layer, and there are lateral superior genicular arteries and veins in the deep layer.
Operations: The filiform needle (acupuncture needle) manufactured by Beijing Zhongyan Taihe Medical Devices Co., Ltd. was selected and its specification was 0.5-1.0 inch. The patient was placed in the supine position, and the contralateral Yanglingquan point of the lesion was used. After the routine local disinfection, the needle was quickly pierced using hand holding and clamping techniques, and then the twisting and turning as well as lifting and thrusting techniques were performed. When patients have an obvious sensation of qi, the substantial twisting and turning back and forth were conducted for 2-3 times, and then the lifting and thrusting techniques were carried out for 4-6 times, so that patients could have a strong sensation of needling. The intensity should be based on the patient’s tolerability, and the needle was withdrawn 15 minutes after the retaining of the needle. Subsequently, acupuncture was performed once a day, and 7 times constituted a circle. The efficacy was subjected to statistics after two circles.
Control group
Acupoint selection: The Sibai point was used in patients with periorbital spasm, the Dicang point was used in patients with perioral spasm, and the Taichong point was used in patients with eye and facial spasm.
Operations: The 1ml syringe and No.5 syringe needle were selected, and 1.0ml (500 μg) of vitamin B12 injection was drawn every time. The syringe was taken out from the package, and the bevel of the needle and the scales of the syringe were kept to the same horizontal level and tightened. A check was performed to see whether the syringe leaked or not. Then the drug was drawn and the air in the syringe was exhausted. The doctor used his forearm to drive his wrist, so that the needle could be pierced into the skin of the patient's acupoint quickly. The patient was placed in a sitting or supine position, and the needle was pierced by 0.5 inch after the injection point was routinely disinfected. After no blood was found during the withdrawing of the needle, 0.5 ml of vitamin B12 injection was slowly injected. The injection was performed every 5-7 days, and 7 consecutive days constituted a circle, and the interval between the two circles is about 3 days. The efficacy was subjected to statistics after two circles.
Therapeutic Outcomes
Criteria of results
Cured: The HFS disappeared.
Effective: The frequency, time, and grade of spasm of the HFS were significantly reduced.
Improved: The frequency, time, and grade of spasm of the HFS were reduced.
Ineffective: No significant changes occurred as compared with conditions before treatment.
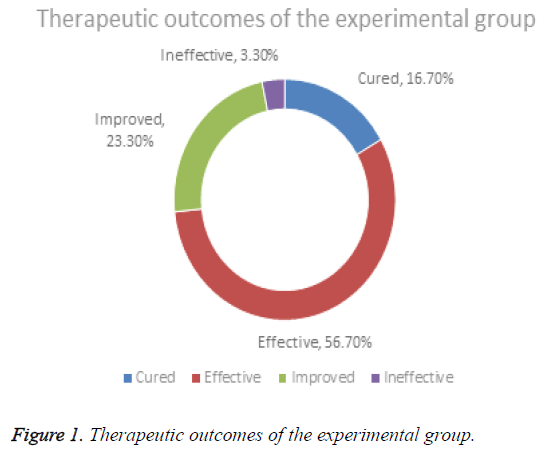
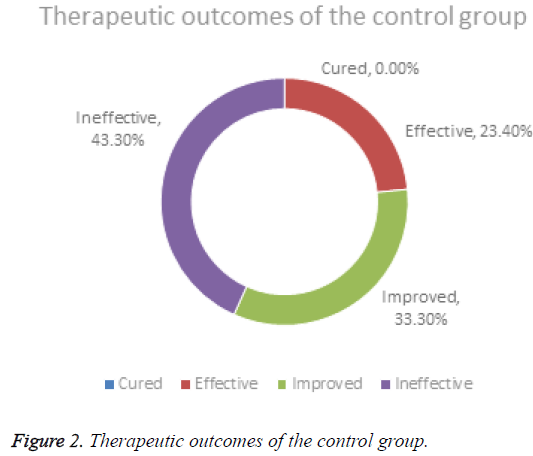
We divided two groups of patients before treatment, the same grade of patients were random selected into two groups, the number of each grade of HFS is almost the same, the difference can be ignored; only can be judged twitch effects were compared between the two groups after treatment. The curative effect evaluation standard from doctors’ objective observation in the degree and the frequency of occurrence of convulsions, combined with their own subjective feelings (Tables 3 and 4 and Figures 1 and 2).
| Efficacy | Cured | Effective | Improved | Ineffective |
|---|---|---|---|---|
| N | 5 | 17 | 7 | 1 |
| Total | 30 | |||
Table 3: Therapeutic outcomes of the experimental group.
| Efficacy | Cured | Effective | Improved | Ineffective |
|---|---|---|---|---|
| N | 0 | 7 | 10 | 13 |
| Total | 30 | |||
Table 4: Therapeutic outcomes of the control group.
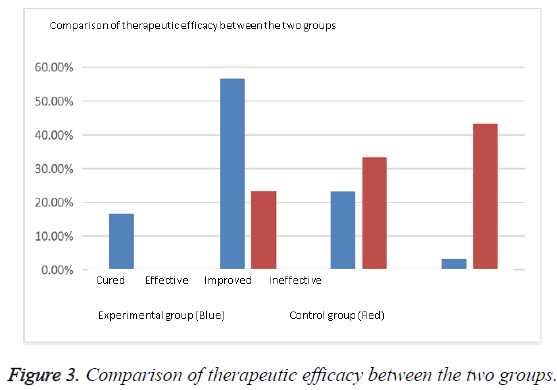
As is shown in Figure 3, the comparisons between the efficacy of acupuncture of contralateral Yanglingquan point and the injection of vitamin B12 at the acupoint showed that the former is much better than the latter (Table 5). The statistical analysis showed a significant difference (P<0.1), and the efficacy of the experimental group was significantly superior to that of the control group. This method shows such advantages as small invasions, high efficacy and uniqueness in methods.
| Group | Experimental group | Control group |
|---|---|---|
| Total (n) | 30 | 30 |
| Cured n (%) | 5 (16.7%) | 0 (0) |
| Effective n (%) | 17 (56.7%) | 7 (23.4%) |
| Improved n (%) | 7 (23.3%) | 10 (33.3%) |
| Ineffective n (%) | 1 (3.3%) | 13 (43.3%) |
| Total response rate | 0.967 | 0.567 |
Table 5: Comparison of therapeutic efficacy between the two groups.
Discussion
The pathogenesis of HFS in the current clinical studies is not clear, and there are few treatment options for it. Currently, it is mostly considered to be associated with some special stimuli on the facial nerve pathways, and some patients may be due to the arteriosclerotic expansion of the vertebral-basilar artery system, or the demyelination degeneration after facial neuritis and inflammation of the cerebellopontine angle [7,8]. The commonly used Western medicine therapy nowadays is surgery, while its efficacy was poor. There is also another point of view that the compression of the root exit zone (REZ) of facial nerve by blood vessels is considered to be a common cause of HFS [9,10]. Secondly, space-occupying lesions are also a reason for the development of HFS, namely "secondary HFS," such as cerebellopontine angle tumors, arteriovenous malformation, aneurysm and arachnoid cyst, etc. Other causes include sequelae of facial neuritis, multiple sclerosis and familial causes. The pathogenesis of HFS may be the ectopic excitation of facial nerves or pseudo-synaptic transmissions [11-13].
Currently there are two main hypotheses [14], the "short-circuit hypothesis": The REZ segment was unmyelinated, and was impaired due to the long-term vascular compression. The exposed axons contacted with each other, and ectopic impulses transmitted across the synapses occurred between nerve fibers. 2, the "kindling hypothesis": The REZ segment was subjected to vascular compression, and the pulsatile stimulation of blood vessels was similar to ignition, and therefore, antidromic impulses were generated and induced the increase in the excitability of the facial nerve nucleus and activation of stationary synapses, thereby resulting in HFS. Currently the established cases of HFS induced by REZ of facial nerve under vascular compression account for about 80% to 90% of all cases [15]. Besides, other locations under vascular compression (such as the labyrinthine artery and other mutant aortas, such as the vertebral artery and the basilar artery) form the compression of facial nerves, resulting in HFS [16]. Literature in recent years shows that there are roughly 3 types of vascular compression: single vascular loop compression (which accounts for the largest proportion, roughly 75% to 85%), multi-point compression (7% to 16%), and compression induced by vessels penetrating facial nerves (which accounts for the minimum proportion, 1% to 2%) [17].
The Insights into the Origin of Miscellaneous Diseases records that tendons exist for constricting bones, tripping flesh and stretching skin, and they represent the key of human bodies and benefit their movement. Modern medicine believes that tendons are mainly composed of muscles, fascia, ligaments and other systems and are the general term for the human muscle system. They not only include the substance of tendons, but also the function and structure of tendons. The Yanglingquan point is below the knee. Suwen (Basic Questions) records that tendons are located in the knee and acupoints belong to tendons. So acupoints are closely related to the function and structure of tendons. Analysis according to the TCM theory shows that HFS is an abnormal state of facial muscles, and the Yanglingquan point is the he-sea point of the gallbladder meridians of Foot-Shaoyang. According to Lingshu (Spiritual Pivot), “qi in veins joins at the he-sea point”. He-sea point is the acupoint with the strongest qi in veins, like all rivers joining the sea. Therefore, as the he-sea point of gallbladder meridians, Yanglingquan is the acupoint with the strongest qi in meridians of gallbladder meridians. One gallbladder meridian flows through Fengchi point to the middle of the ear and the front of the ear to the outer canthus. The other gallbladder meridian branches at the outer canthus, goes down to Daying point, joins the triple energizer meridian of Hand- Shaoyang at the eye socket, goes down to the supraclavicular fossa via Jiache point and the neck. It can be seen from it that the circulation sites of the gallbladder meridian includes the position of facial muscles, so gallbladder meridian can be used to treat facial muscle diseases. While the Yanglingquan point is the site with the greatest qi of the gallbladder, so it is the best candidate option for the treatment of lesions at the circulation sites.
Muscles along the gallbladder meridian of Foot-Shaoyang are characterized by “intersection of meridians”. So the contralateral acupoint should be selected upon acupoint selection. The mechanism of “intersection of meridians” is not clearly defined in the academic world. We studied relevant literature and now analyzes in combination with previous discussions: Take the left gallbladder meridian of Foot- Shaoyang for example; it starts from the fourth toe of the left foot and “connects with the lateral malleolus”; its trunk passes through the middle part outside the left lower limb, “goes up to via the small rib below the costal region” from the left side of the truncus, “goes up and comes out from the axilla and passes through the supraclavicular fossa”, goes along the back of the left ear, goes up to the left frontal angle, “joins at Dianshang point” with the right gallbladder meridian of Foot-Shaoyang running on the right side, goes down to the “chin” (the soft parts on two sides below the chin and above the Adam's apple), and returns and goes up to gather at the right (the cheekbone below the eye). The trunk continues to “goes up to the right frontal angle and intersects the Qiao meridian”. This is called “intersection of the left meridian with the right one”; the branch gathers at the right “outer canthus” and is the “outer meridian” of the right eye. As the left gallbladder meridian of Foot-Shaoyang intersects via Dianding and is distributed to parts including the right frontal angle and eyes, so under pathologic condition, “the left meridian intersects the right meridian, so the right eye can’t open”, or “the right frontal angle is injured, so the left foot can’t move normally”. On the contrary, the circulation distribution of the right gallbladder meridian of Foot-Shaoyang is called “intersection of the right meridian with the left one”, so under pathologic condition, “the right meridian intersects the left meridian, so the left eye can’t open”, or “the left frontal angle is injured, so the right foot can’t move normally”. In the treatment of patients, “intersection of meridians” is considered, so the contralateral acupoint should be selected upon acupoint selection. According to circulation of the gallbladder meridians of Foot- Shaoyang, acupuncture in the contralateral acupoint can treat diseases of head and facial muscles on this side, so as to achieve the effect of cure with one needle.
References
- Wang YN, Zhong J, Zhu J, Dou NN, Xia L, Visocchi M, Li ST. Microvascular decompression in patients with coexistent trigeminal neuralgia, hemifacial spasm and glossopharyngeal neuralgia. Acta Neurochirurgica 2014; 156: 1167-1171.
- Sorgun MH, Yilmaz R, Akin YA, Mercan FN, Akbostanci MC. Botulinum toxin injections for the treatment of hemifacial spasm over 16 years. J Clin Neurosci 2015; 22: 1319-1325.
- Barbosa ER, Takada LT, Gonçalves LR, Costa RM, Silveira-Moriyama L. Botulinum toxin type A in the treatment of hemifacial spasm: an 11-year experience. Arq Neuropsiquiatr 2010; 68: 502-505.
- Møller AR. Pathogenesis and Treatment of Hemifacial Spasm. In Microvascular Decompression Surgery. Springer Netherlands 2016.
- Wang X, Thirumala PD, Shah A, Gardner P, Habeych M, Crammond DJ, Horowitz M. Effect of previous botulinum neurotoxin treatment on microvascular decompression for hemifacial spasm. Neurosurgical Focus 2013; 34: E3.
- Takeda R, Ookawara M, Fushihara G, Kobayashi M, Fujimaki T. Successful Treatment of Hemifacial Spasm Caused by an Ectatic Vertebral Artery Accompanying Agenesis of the Carotid Artery. Surgery J 2016; 2: e105-e107.
- Youtian L, Yuping B, Qi F. Clinical study of acupuncture of Houxi point for the treatment of HFS.Acupuncture Res 1999; 2: 90-92.
- Yuquan S. Practical Neurology. 2nd Edition, Shanghai: Shanghai Scientific & Technical Publishers, 2000.
- Zhong J, Li ST, Zhu J, Guan HX. Is entire nerve root decompression necessary for hemifacial spasm? Int J Surg 2011; 9: 254-257.
- Campos-Benitez M, Kaufmann AM. Neurovascular compression findings in hemifacial spasm. J Neurosurg 2008; 109: 416-420.
- Yi S, Renmin Y, Jingxian H. Practical traditional Chinese medicine and Western medicine neurology. Beijing: People's Medical Publishing House, 2011.
- Jiang W, Jianping J, Liying C. Neurology. Beijing: People's Medical Publishing House, 2005.
- Qi H, Wang Z. Research advances in causes and therapies of HFS. Nervous Dis Mental Health 2006; 8: 399.
- Chuan J. Research advances in causes and pathogenesis of HFS. J Int Neurol Neurosurgery 2012; 39: 63.
- Sindou M, Fischer C, Derraz S, Keravel Y, Palfi S. Microsurgical vascular decompression in the treatment of facial hemispasm. A retrospective study of a series of 65 cases and review of the literature. Neurochirurgie 1996; 42: 17-28.
- Chung SS, Chang JW, Kim SH. Microvascular decompression of the f- acial nerve for the treatment of hemifacial spasm: preoperative magnetic resonance imaging related to clinical outcomes. Acta Neurochir 2000;142: 901-907.
- Li CS. Varied patterns of postoperative course of disappearance of hemifacial spasm after microvascular decompression. Acta Neurochir 2005; 147: 617-620.