Research Article - Current Pediatric Research (2021) Volume 25, Issue 9
Clinical evaluation for bronchoscopic management in pediatric patients suspected to have foreign body inhalation.
Fawaz Mahmood Mustaf Alfaqe*, Bassam Khaleel Al-Abbasi
Department of Surgery, College of Medicine, Ninevah University, Mosul, Iraq
- Corresponding Author:
- Fawaz Mahmood Mustaf Alfaqe
Department of Surgery
Ninevah University
Mosul
Iraq
Tel: +964 771-291-3336
E-mail: drnihadkhalawe@gmail.com
Accepted date: 15thSeptember, 2021
Abstract
Background: Tracheobronchial foreign body aspiration in pediatric is a life-threatening condition, the early diagnosis and treatment are crucial to prevent complications. Patients and Methods: 51 patients younger than 14 years, were studied in Al-Khanssa teaching hospital, according to their age, sex, time of presentation, history of foreign body aspiration, clinical, radiological as well as bronchoscopic findings. Results: In 51 patients (27 males, 24 females), mean age 4.3 years, largest portion presented within first 24 hour of FB aspiration (43%), positive history was noted in 84.3%, with PPV of 95.5%, NPV of 85.7%, most common clinical presentations were dyspnea (68.6%) and cough (64.7%),most common finding in clinical examination was rhonchi (47.1%), the consolidation was the most common CXR findings(35.3%), negative CXR noted in 29.4%, most commonly encountered FB is organic materials (54.9%), mainly food, Right Main Bronchus (RMB) is the most common site of FB impaction (35.3%) followed by Left Main Bronchus (LMB) (31.4%), then trachea (9.8%), Rigid Bronchoscopy (RB) was done urgently in most of the cases (78%), additional procedures are needed in limited number of cases and they included esophagoscopy and thoracotomy, no mortality or morbidity were recorded after RB. Conclusion: Positive history of inhalation is most important indicator of TFBA, clinical findings can aware doctor for possibility of TFBA especially in toddlers, however none of clinical findings are specific, the most specific Chest X-Ray finding (CXR) is detection of radiopaque FB, however this is uncommon finding, hence most common aspirated FB are organic radiolucent materials, negative CXR cannot exclude TFBA, especially when history and clinical findings are suggestive, the rigid bronchoscopy, remains the gold standard in the management of TFBA.
Keywords
Foreign body, Tracheobronchial foreign body aspiration, X-ray finding of chocking, Pediatric foreign body aspiration, Bronchoscopic aspiration.
Introduction
Tracheobronchial Foreign Body Aspiration (TFBA) in pediatric is a dangerous, life-threatening condition seen commonly in emergency department resulting in significant morbidity and mortality [1-5]. It is a common occurrence in preschool children especially at age of less than three years where it is associated with high morbidity and mortality [6,7]. The fact that the younger children are at high risk of aspiration because less airway protection reflex, poor chewing ability, lack of molars dentition, crying, laughing or playing with siblings while eating, in addition to negligence the boys are more prone to TFBA than girls.
The location is anywhere from the pharynx to the bronchi, but more commonly seen in right main bronchus and in a minority of cases FB has been shown changing its location [8]. In general FB are classified into either organic (such as teeth and plants) or non-organic substances (such as metals and plastics that seen in small parts of toys and beads), FB are also classified according to their shape into sharp and blunt objects. Symptoms produced by inhaled FB related to shape, size, location, duration and the type of FB, the organic FB causes more severe mucosal inflammation than inorganic materials which are less irritant to the mucosa and thus are very frequently asymptomatic and may be diagnosed incidentally
The diagnosis begins with a history of witnessed aspiration, physical examination and may be supported by radiological examination, the problem raised with an uncertain or negative history of FB aspiration. Physical findings seen in TFBA such as cough, wheeze, respiratory distress, noisy breathing are nonspecific [9], as well radiological findings, where most common Chest X-Ray (CXR) findings that are air trapping, signs of infection, atelectasis, or radiopaque foreign bodies, can be seen in a patient without TFBA. On the other hand, patients with confirmed TFBA may not be present with any abnormality at CXR. Rigid Bronchoscopy (RB) examination remains definitive diagnostic approach with treatment modality of choice if required, however RB is associated with significant risks and complications and potential long-term effects associated with general anesthetic in children there is no well-defined indications for bronchoscopy in TFBA [10].
In our institution, problem arises if we have a negative or unclear history of inhalation, and if physical and radiological findings are all negative, the decision should be made whether to take the risk of exposing them to bronchoscopy or not? This study is designed to look for physical, radiological signs, as well as presence or absence of witnessed FB inhalation, to look for correlation between evaluated criteria and findings in bronchoscopy.
Patients and Methods
A prospective study held in Al-khansaa teaching hospital, Mosul, Ninevah governorate/IRAQ, from August 2018 to April 2019. The participants include 51 patients (27 male and 24 female) aged 14 years old or younger, that are admitted for suspected FB inhalation, exclusion criteria include patients who have an inhaled FB that found to be located above level of glottis, and those who are more than 14 years old, or those in whom the CXR is not obtained, after their admission to surgical ward, each patient were evaluated according to the followings:
•Age and gender.
•Time of presentation after suspected inhalation.
•Presence or absence of a history of witnessed inhalation.
•Clinical presentation including dyspnea, cough, choking, wheezes, recurrent chest infection, cyanosis, strido, etc.
•Finding in the physical exam, with a concentration on chest auscultation findings, like bilateral/unilateral rhonchi, diminished air entry, crepitation, etc.
•Radiological evaluation by CXR, including, consolidation, obstructive emphysema, collapse, pneumothorax, radiopaque FB etc.
•Type of FB.
•Exact site of FB in the airway.
•Rigid Bronchoscopy (RB) findings and complication were all monitored and recorded.
•After admission and evaluation, the patients were resuscitated by O2, nebulization, IV line, IV antibiotics and intravenous dexamethasone.
•Rigid bronchoscopy was done for 50 patients (one patient refused), written informed consent to perform bronchoscopy was provided by all patients, caregivers before the procedure, all bronchoscopy done under GA with short-acting muscles relaxant using rigid bronchoscopy, With or without video scope
Postoperatively patients were admitted for 1-3 days for follow up, there were no recorded complications at time of anesthesia, bronchoscopy, and early postoperative days, and no mortalities were recorded among these cases as well.
Statistical analysis
Statistics is done by using Two-sided Fisher exact to calculate sensitivity, specificity, and Positive Predictive Values as well Negative Predictive Values (PPV, NPV) of variables. P values <0.05 were considered significant. The IBM SPSS statistics 22 was used to perform the statistical analysis.
Results
Age and sex
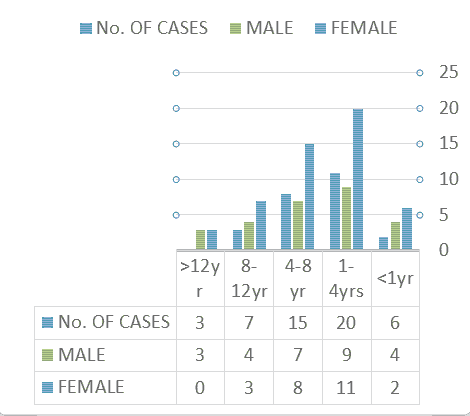
In total of 51 patients (27 male and 24 female), (mean age 4.4 years, median 3.1 year, range from 7 months to 13.5 years), age and sex distribution is displayed in Figure 1.
Time of presentation
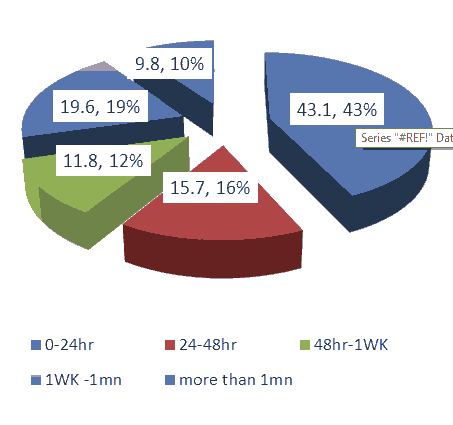
The time of presentation is ranging from less than one hour up to 7 months as shown in the Figure 2 below.
History of witnessed FB inhalation
In Table 1 among all the examined cases, the prevalence of FB inhalation is 84.31%, The PPV of the history of witnessed inhalation is 95.45%, (42 from the total 44 patients), The NPV is 85.71%, (7 patients who had no witnessed FB inhalation, 5 found to have FB by RB and one patient refused RB).
| History/FB | Positive FB | Negative FB | Total |
|---|---|---|---|
| Positive Hx | 42 | 2 | 44 |
| Negative HX | 1 | 6 | 7 |
| Total | 43 | 8 | 51 |
Table 1. History of witnessed FB inhalation.
Clinical presentation
Most of the cases are present with more than one symptom, dyspnea, cough, and choking are the most common presenting symptoms, 80.4% of patients have one or more of these symptoms and in different combinations, Table 2, shows the frequencies of the presenting symptoms.
| Presentation | No | % |
|---|---|---|
| Dyspnea | 35 | 68.6 |
| Cough | 33 | 64.7 |
| Choking | 23 | 45.1 |
| Local wheezes | 14 | 27.5 |
| Recurrent chest infection | 8 | 15.7 |
| Cyanosis | 7 | 13.7 |
| Strider | 3 | 5.9 |
| others* | 4 | 7.8 |
Table 2. Frequencies of the clinical presenting symptoms. *: Fever, apnea, whistling, halitosis, accidental findings.
Clinical examination
The most common finding in the clinical examination is rhonchi (unilateral/bilateral) (47.1%), other finding is listed in Table 3.
CXR findings
Consolidation is the most common CXR finding in the examined cases (35.3%) other findings are listed according to the frequency, below in Table 3.
| Auscultation findings | No. | % | CXR Findings | No. | % |
|---|---|---|---|---|---|
| Bilateral/unilateral rhonchi | 24 | 47.1 | Consolidation | 18 | 35.3 |
| Diminish air entry | 22 | 43.1 | Normal | 15 | 29.4 |
| Crepitation | 14 | 27.5 | Obstructive emphysema | 9 | 17.6 |
| Bilateral No air entry | 1 | 2 | radio-opaque FB | 9 | 17.6 |
| Normal | 7 | 13.7 | Collapse | 3 | 5.9 |
| Pneumothorax | 1 | 2 |
Table 3. Clinical finding and CXR finding.
Types of FB
The most common encountered FB is organic materials (54.9%) vs. (45.1%)
| Type of FB | No | % | Site | No. | % |
|---|---|---|---|---|---|
| Sun flower seed | 15 | 34.9 | RMB | 18 | 35.3 |
| Watermelon seed | 6 | 14 | LMB | 16 | 31.4 |
| Peanut | 6 | 14 | Trachea | 5 | 9.8 |
| Needles/pin | (5) 4(LMB) 1(RMB) | 11.6 | Larynx | 3 | 5.9 |
| Pen plastic cup | 2 | 4.7 | Bilateral | 1 | 2 |
| Bead | 2 | 4.7 | Total | 43 | 84.3 |
| Pistachio | 1 | 2.3 | |||
| Globe light | 1 | 2.3 | |||
| Screw | 1 | 2.3 | |||
| Cabbage leaf | 1 | 2.3 | |||
| Coin | 1 | 2.3 | |||
| Could wires | 1 same pt. | 2.3 | |||
| Stone* | 1(same pt.) | 2.3 | |||
| Toy whistle | 1 | 2.3 | |||
| Total | 44(43 pts.) | 100 |
Table 4. Site and type of FB.
In Table 4 non-organic FB, different types of extracted FB are listed below according to frequencies.
Site of FB: The most common site of FB impaction is at the Right Main Bronchus (RMB) (35.3%), the sites of FB impaction are listed at Table 4.
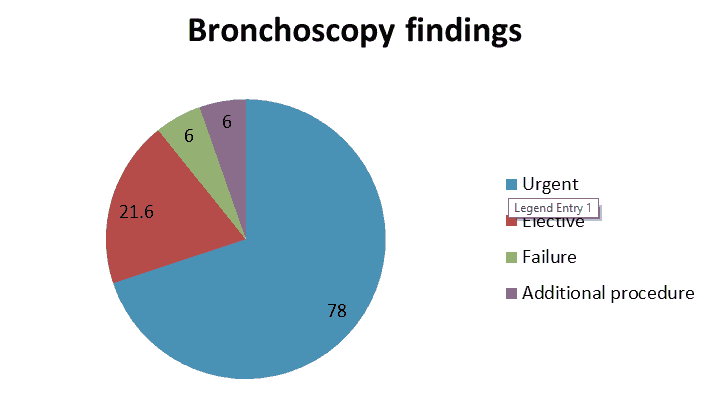
Rigid Bronchoscopy (RB): In 78% of cases (39 cases), the RB done urgently, while 21.6% of the cases (11 cases) it is done electively with a failure rate of 3% (3 cases, 2 of them they were in need of reevaluation by RB and one of them needed thoracotomy and esophagoscope) (Figure 3).
Discussion
Foreign Body (FB) aspiration is common life-threatening emergency regarded as most common cause of intraluminal airway abnormalities in pediatric, and still a cause of mortality especially in preschool age [11]. Delayed or missed diagnosis of TFBA can result in complications ranging from chronic wheezing to life-threatening airway obstruction [12]. In our study the Highest incidence of FB inhalation noted at age group of 1-4 years (39.2%), other studies also show young age group is more prone to FB inhalation, with age range differs but mainly range between 1-6 years [13,14]. The mean age however, in our study is significantly higher than other studies (P-value=0.001, 0.001 respectively). This is related to the tendency of the children to explore new objects by their mouth and nose. The females 8 years and older in our study noted to inhale needle scarf pins, girls should be warned not to hold pin between their teeth while making their scarf especially during talking or laughing, thereby avoid the risk of inhalation, same noted by other studies [1,7,15].
In our study males are more prone to inhale FB than females; same noted by other studies however with smaller sex difference male represents (52.9%) in the current study. The TFBA is easier to diagnose clinically if presented with acute symptoms as choking and coughing, the complication of TFBA is shown to be less for the patients that arrive to the hospital earlier. In our study, the peak time of presentation is within 1st 24 hours of inhalation (43.1%), same noted by other studies, the early presentation is associated with acute symptoms, while the late presentation that still noted till 7th month after FB inhalation (9.8%) associated with more chronic symptoms, uncertain history of inhalation and a symptoms free periods [16]. A positive history of FB inhalation is markedly different between the studies from for example 33.3% only in Sahdan et al., 47% in Puja et al. In our study positive history is seen in (97.6%) this may reflects good observation as well alertness of the families to the risk of FB inhalation in our locality, the history of inhalation shows PPV, NPV, sensitivity as well specificity of (95.45%, 85.71%, 97.67%, 75.00%) respectively, from the given data its shown that the history of FB inhalation is an important factor in the diagnosis of FB inhalation [14,13].
In our study, it's found that patients who present with positive FB aspiration and acute symptoms tend to be diagnosed early, the same found by Sahdan et al. dyspnea cough and choking are the most common presenting symptoms in our study (68.6%, 64.7%, 45.1% respectively), similarly symptoms reported by other studies but with different orders (choking then cough and dyspnea, choking wheeze or cough 3, cough dyspnea and fever choking, wheeze and decreased breath sound all the above-given symptoms are nonspecific, the child presented with these symptoms may be treated as for example a case of asthma, recurrent pneumonia or trachiobronchiolitis, this will cause delay of diagnosis [17]. The most common finding in the clinical examination is rhonchi (unilateral/bilateral), followed by decreased air entry, (47.1%, and 43.1% respectively).
These compared to unilaterally reduced breath sounds(91.7%), followed by tachypneic (83.3%) at Sahdan et al. normal CXR in FB inhalation varies in different studies, in our study normal CXR is seen in 29.4%, compared to 21.6% Sahdan et al. 35.6% Sattar et al. 46% in Dar et al. The CXR findings shows PPV, NPV, sensitivity and specificity of (91.7%, 33.33%, 76.7%, 62.5% respectively), compared to 66.6% and 50% (sensitivity and specificity of CXR at Sattar et al. In our study negative CXR, cannot exclude FB inhalation especially with positive history as well clinical findings, the most common CXR finding. In current study is consolidation (35.3%) vs. obstructive emphysema in other studies. In our study, none of the CXR findings (except FB detection) is specific to FB inhalation, Detection of FB by CXR in bio microscopically positive cases found in 9 cases (17.6%) with PPV and specificity of 100%, however low NPV as well sensitivity (19%, 20.9% respectively). This finding is agreed by Dar et al. how stated that radiopaque FB is the most definitive sign in CXR.
The most common encountered FB is organic materials, mainly food seeds (67.4%) and this is shown also by other studies. In our study the most common site of FB impaction is at the Right Main Bronchus (RMB) (35.3%), followed by Left Main Bronchus (LMB) (31.4%), same reported by other studies [18]. In our study we reported a case of bilateral bronchial FB inhalation (two pieces of the peanut), the first FB is extracted from RMB, then the patient is reevaluated, the second FB was then extracted from LMB, the similar rare case is reported by Zhao et al. [19]. In our study, the prevalence of FB detected by RB among all studied cases is 84.3%, nearly similar results achieved by other studies. In 78% of cases (39 cases), the RB has done urgently, in 21.6% of the cases (11 cases), it is done electively with a failure rate of 3% (3 cases, 2 of them they need reevaluation by RB and one of them need thoracotomy) and esophagoscope. All the FB are removed after all with few Complications that are either due to the nature of foreign body itself or due to the removal procedures, the cases in whom the RB where negative for FB referred to the pediatricians, for further evaluation and management, no serious complications or mortality has been detected among the examined cases [20].
Conclusion
Pediatric FB inhalation is a serious life-threatening condition, mainly in the young age group, the early diagnosis is crucial to prevent complications like pneumonia, lung abscess or even death. FB once suspected should be removed as early as possible, High clinical suspicion is required, the diagnosis depends mainly on history, clinical and radiological basis, among the three, clear history of inhalation of FB is the most important, especially in the young age group and when associated with acute symptoms as well as clinical and radiological findings, all the CXR findings except FB detection, are nonspecific, negative CXR cannot exclude FB inhalation, rigid bronchoscopy is mandatory in case of high suspicion, no major complication are associated with procedure in the current study.
Availability of Data and Materials
The data and material used in this study are available on reasonable request from corresponding author.
Abbreviations
FB: Foreign Body; NPV: Negative Predictive Value; TFBA: Tracheobronchial Foreign Body Aspiration; PPV: Positive Predictive Value; SPSS: Statistical Package for Social Sciences.
References
- Cohen S, Avital A, Godfrey S, et al. Suspected foreign body inhalation in children: what are the indications for bronchoscopy?. J pediatr 2009; 155(2): 276-80.
- Sahin A, Meteroglu F, Eren S, et al. Inhalation of foreign bodies in children: experience of 22 years. J Trauma Acute Care Surg 2013; 74(2): 658-663.
- Kwok MM, Wong A, Paddle P, et al. Clinico-radiological predictors of positive rigid bronchoscopy findings in children with suspected tracheobronchial foreign body aspiration. AJO 2018; 1(2).
- Dar NH, Patigaroo SA, Hussain T. Foreign body inhalation in children: clinical presentations and x-ray chest findings. Int J Med Sci Public Health 2016; 5(11): 2274-2278.
- Mallick MS. Tracheobronchial foreign body aspiration in children: A continuing diagnostic challenge. Afr J Paediatr Surg 2014; 11(3): 225-228.
- Oliveira CF, Almeida JF, Troster EJ, et al. Complications of tracheobronchial foreign body aspiration in children: report of 5 cases and review of the literature. Rev Hosp Clin Fac Med Sao Paulo 2002; 57(3): 108-111.
- Orji FT, Akpeh JO. Tracheobronchial foreign body aspiration in children: how reliable are clinical and radiological signs in the diagnosis?. ClinOtolaryngol 2010; 35(6): 479-485.
- Denny SA, Hodges NL, Smith GA. Choking in the Pediatric Population. Am J Lifestyle Med 2016; 9(6): 438-441.
- Swanson KL. Airway foreign bodies: what's new?. Semin Respir Crit Care Med 2004; 25(4): 405-411.
- Singh H, Parakh A. Tracheobronchial foreign body aspiration in children. Clin Pediatr 2014; 53(5): 415-419.
- Reilly J, Thompson J, MacArthur C, et al. Pediatric aerodigestive foreign body injuries are complications related to timeliness of diagnosis. Laryngoscope 1997; 107(1): 17–20.
- Sattar A, Ahmad I, Javed AM, et al. Diagnostic accuracy of chest x-ray in tracheobronchial foreign body aspiration in paediatric patients. J Ayub Med Coll Abbottabad 2011;23(4): 103-105.
- Puja D, Arun KR, Ashok B, et al. Foreign Body Aspiration in Paediatric Airway. Int J Med 2017;6(3): 17-21.
- Sahadan DZ, Zainudin NM, Kassim A, et al. Case series of foreign body aspiration in Paediatric Institute, Hospital Kuala Lumpur. Med J Malaysia 2011; 66(5): 484-486.
- Hamad AM, Elmistekawy EM, Ragab SM. Headscarf pin, a sharp foreign body aspiration with particular clinical characteristics. Eur Arch Otorhinolaryngol 2010; 267(12): 1957-1962.
- Soysal O, Kuzucu A, Ulutas H. Tracheobronchial foreign body aspiration: a continuing challenge. Otolaryngol Head Neck Surg 2006; 135(2): 223-226.
- Lea E, Nawaf H, Yoav T, et al. Diagnostic evaluation of foreign body aspiration in children: a prospective study. J Pediatric Surg 2005; 40(7): 1122-1127.
- Lluna J, Olabarri M, Domenech A, et al. Recommendations for the prevention of foreign body aspiration. An Pediatr 2017; 86(1): 50.
- Zhao Z, Gao Q, Song P. A rare case of bilateral bronchial foreign body. Pak J Med Sci 2015; 31(2): 477-479.
- Rasha NA, Bassam K, AlAbbasi Nashwan M. et al. Foreign body aspiration in children: Radiological evaluation of preoperative chest X-Ray. Ann Trop Med Public Health 2021; 24(4): 341-353.