Research Article - Biomedical Research (2017) Volume 28, Issue 16
Clinical application of platelet-rich plasma for the treatment of refractory sinus wounds
Junjie Xia#, Zhiming Ni# and Hong Ye*
Department of Orthopaedic, 117th Hospital of PLA, Hangzhou, Zhejiang, PR China
#These two authors contributed equally to this paper
Accepted date: July 18, 2017
Abstract
Objective: To evaluate the clinical efficacy of Platelet-Rich Plasma (PRP) in the treatment of refractory sinus wounds.
Methods: Twelve patients with refractory sinus wounds were recruited for this study. Among them, the sinus wounds in eight patients were caused by fracture fixation and in four patients were caused by trauma. The PRP was locally injected following wound debridement. The strength of pain and wound healing were observed after treatment.
Results: In the 12 cases that were treated with PRP, 7 cases exhibited significant pain relief, 6 cases were partly healed and 6 cases were completed healed.
Conclusions: The local injection of PRP which is simple and safe has shown significant healing efficiency and pain relief in the treatment of refractory sinus wounds.
Keywords
Platelet-rich plasma, Sinus wound, Wound healing
Introduction
In the treatment of orthopaedic trauma, the Vacuum-Sealing- Drainage (VSD) technique is widely recognized for repairing soft tissues with favourable therapeutic efficiency, however, it has obvious limitations in the treatment of chronic sinus wounds. Traditional therapy combines antibiotics with dressing changes for the treatment of sinus wounds, however, often leads to long course and poor wound healing. In the current study, we try to repair the sinus wound through local injection of PRP and the particulars are as follows.
Methods
General information
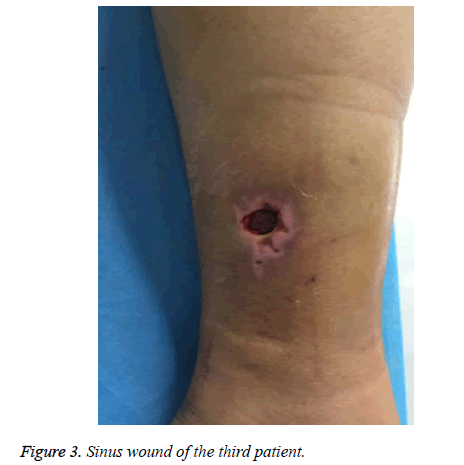
The study includes 12 cases, 7 cases are male and 5 cases are female with an average age of 54 (37~68 y old). In addition, the sinuses in 8 cases were caused by wound infection after fracture fixation with an average treatment course of 5 months (3~10 months), and the sinuses in the other 4 cases were caused by trauma-mediated soft tissue contusion with an average treatment course of 3 months (2~6 months). During treatment, 12 patients received X-ray examination and no osteomyelitis was found. Before PRP injection, the patients were treated by antibiotics and dressing changes and all of them had different degrees of pain. According to the Faces Rating Scale-Revised (FRS-R) scores [1], 3 cases had mild pain, 7 cases had moderate pain, and 2 cases had severe pain as shown in Table 1.
| Patient number | Age (year) | Gender | Wound position | Wound size (length × width × depth cm3) | Treatment course (month) | Pain level |
|---|---|---|---|---|---|---|
| 1 | 37 | male | The middle-lower inside of left crus | 3 × 2 × 4 | 2 | severe |
| 2 | 42 | male | The lower front side of Left crus | 3 × 1.5 × 1 | 3 | moderate |
| 3 | 43 | female | The distal inside of right crus | 1 × 1 × 4 | 1 | moderate |
| 4 | 48 | male | The middle-lower anterolateral side of left crus | 2.5 × 2 × 1 | 5 | mild |
| 5 | 48 | male | The posterolateral side of left forearm | 2 × 1.6 × 4 | 6 | moderate |
| 6 | 50 | female | The middle-lower lateral side of left crus | 1.5 × 1 × 2.8 | 5 | mild |
| 7 | 52 | male | The left inner ankle | 1.8 × 1.3 × 2.5 | 3 | moderate |
| 8 | 60 | male | The middle-upper lateral side of right crus | 3 × 2 × 4 | 3 | moderate |
| 9 | 65 | female | The distal anterolateral side of left crus | 3 × 1.7 × 1.5 | 10 | mild |
| 10 | 67 | female | The middle-lower inside of left crus | 4 × 3.5 × 5.5 | 6 | severe |
| 11 | 68 | male | The middle anterolateral side of left crus | 4 × 3 × 2 | 4 | moderate |
| 12 | 68 | female | The right external ankle | 2 × 1 × 1.2 | 4 | moderate |
Table 1: Patient’s general information
Treatment and observation
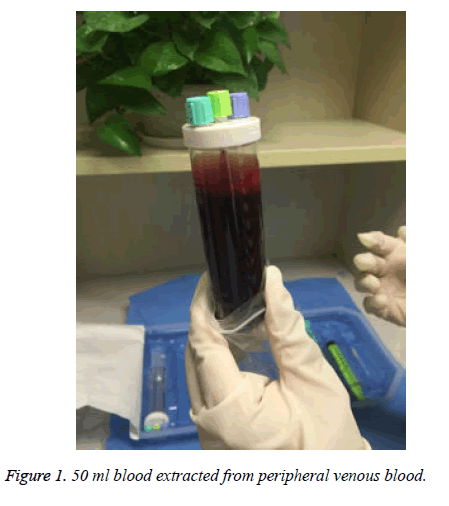
The preparation and usage of PRP: The centrifugation was performed on WG-FZLXJ-I centrifuge and PRP was prepared by commercial kit under aseptic operation. Firstly, 45 mL blood was withdraw from patient’s peripheral venous by using the 50 mL syringes which contained 5 mL sodium citrate solution for anticoagulation, shaked properly and injected into the centrifuge tube.
Centrifuged the samples according to the Landesberg method [2] for 10 min at 200 g and the whole blood was divided into three layers, the top layer is the supernatant, the under layer is the erythrocyte, and the middle layer in light yellow is the PRP layer. The erythrocyte layer was removed by syringe with 3-5 mm left in the tube. The remaining sample was mixed well and centrifuged again for 10 min at 200 g. 3/4 supernatant was discarded and the PRP was extracted by syringe.
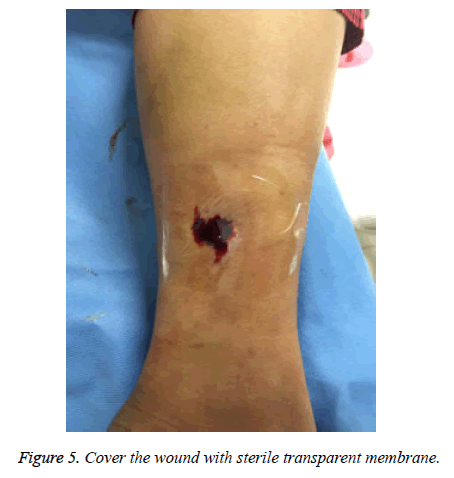
Normally, 5 mL PRP can be produced each time. The wound was injected with PRP until the sinus was filled up, and covered with sterile transparent membrane. After 7 to 10 d, the membrane was removed and the operation can be repeated again if necessary. The 12 patients in this study were treated with antibiotics and the wounds were debrided with no obvious purulent secretion before using PRP.
Observation
The pain degree was determined by the FRS-R scores and the wound healing was monitored after the PRP treatment.
Results
Pain grading
There are 9 patients with moderate or severe pain. After the PRP treatment, 7 patients showed significant pain relief in 1-2 d, and 5 patients had no obvious pain relief.
Wound healing
The following are the criteria of wound healing. Cured: the wound is healed and covered by epithelial tissue; Effective: the wound has no secretion with shrinking ulcer surface, the granulation tissue grows well, and the epithelial tissue begins to cover the wound; Invalid: there is no granulation tissue growth or shrinkage in the wound. Among the 12 patients under PRP treatment in this study, 6 patients were cured and the other 6 patients also showed effective responses. The pain grades and wound healing of patients are summarized in Table 2. Figures 1-6 show the treatment process and wound healing of the third patient.
| Patient number | Treatment time (month) | The number of PRP operations | Pain grade | Wound healing |
|---|---|---|---|---|
| 1 | 2 | 2 | mild | cure |
| 2 | 3 | 2 | mild | cure |
| 3 | 1 | 1 | moderate | cure |
| 4 | 5 | 1 | mild | cure |
| 5 | 6 | 3 | moderate | effective |
| 6 | 5 | 2 | mild | cure |
| 7 | 3 | 3 | mild | effective |
| 8 | 3 | 4 | mild | effective |
| 9 | 10 | 2 | mild | cure |
| 10 | 6 | 4 | moderate | effective |
| 11 | 4 | 3 | mild | effective |
| 12 | 4 | 2 | mild | effective |
Table 2: Pain grade and wound healing after the PRP treatment.
Discussion
Wound healing is a complex process which depends on the coordination of cytothesis, inflammatory cells, extracellular matrix and growth factors to rebuild the damaged soft tissue [3].
There are three main results of wound healing: healed, scar healing, chronic ulcer. During the whole process of tissue healing, the growth factors from platelet play an important role [4,5]. PRP is produced through blood centrifugation which is a mixture and contains rich platelet and growth factors.
The growth factors include Platelet-Derived Growth Factor (PDGF), transforming growth factor (TGF-ß), Fibroblast Growth Factor (FGF), Vascular Endothelial Growth Factor (VEGF), Insulin-like Growth Factor 1 (IGF 1) and Epidermal Growth Factor (EGF) [6].
Local application of these growth factors can activate the inactive macrophages which can release the cytokines such as TGF, EGF in the wound and speed the process of wound healing [7].
The PRP contains a large amount of fibrin which acts a good support for wound healing and stimulates soft tissue regeneration; VEGF is able to stimulate angiogenesis and enhance early wound healing; EGF can accelerate the skin growth, relieve local wound swelling and pain, and reduce postoperative wound exudation.
The PRP demonstrates excellent repairing effects in both acute and chronic refractory wounds. In recent years, PRP technology has been widely used in the treatment of refractory wounds [8,9], soft tissue injury and bone non-union [10-12].
Studies have shown that the injection of PRP into knee joint could improve the restoration of knee joint cartilage and achieved favourable therapeutic effects in the treatment of senile gonarthritis [13,14].
All of the 12 clinical cases in this study are refractory sinus wounds. Among them, 7 cases with moderate or severe pain showed significant pain relief after PRP treatment. The remaining 5 cases had mild pain before PRP treatment and thus lack comparison. These results suggest that PRP is able to significantly relieve pain in wound healing. Carter et al. [15] have reported that PRP contains a large number of white cells and mononuclear cells which can suppress the local inflammation of wounds and ease the pain. Zhang et al. [16] also reported similar results. In our current study, the efficiency of wound healing by the application of PRP is 100%. Several similar results have also been reported [8,17-19] which further confirm the significant therapeutic efficiency of PRP.
The PRP is produced through the centrifugation of blood from patients. Therefore, PRP is very safe with high histocompatibility. In addition, the preparation of PRP is simple. However, the most important thing is, compared with the VSD therapy for the treatment of sinus wounds, the liquid PRP can be directly injected into the sinus and contact the sinus surface adequately regardless of the wound depth which makes full use of the contained cytokines. Generally, the PRP exhibits notable therapeutic effects for the treatment of refractory sinus wounds which provides a novel and effective way for similar wound healing in clinical treatment.
References
- Mi KL, Liang B, Zhang YZ. Orthopedic pain grading and scoring. J Practical Orthopaedics 2013; 3: 232-234.
- Landesberg R, Roy M, Glickman RS. Quantification of growth factor levels using a simplified method of platelet-rich plasma gel preparation. J Oral Maxillofac Surg 2000; 58: 297-300.
- Lv RJ, Liu MJ. The platelet-rich plasma (PRP) technology and its application. China Med Devices Informat 2013; 10: 50-55.
- Behm B, Babilas P, Landthaler M, Schreml S. Cytokines, chemokines and growth factors in wound healing. J Eur Acad Dermatol Venereol 2012; 26: 812-820.
- Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen 2008; 16: 585-601.
- Galliera E, Corsi MM, Banfi G. Platelet rich plasma therapy: inflammatory molecules involved in tissue healing. J Biol Regul Homeost Agents 2012; 26: S35-S42.
- Wang ZG. Molecular biology research in wound healing. Chinese J Traumatol 2000; 6: 6-7.
- Kim SA, Ryu HW, Lee KS, Cho JW. Application of platelet-rich plasma accelerates the wound healing process in acute and chronic ulcers through rapid migration and upregulation of cyclin A and CDK4 in HaCaT cells. Mol Med Rep 2013; 7: 476-480.
- Liu ZW. The clinical application of platelet-rich plasma (PRP) in wound healing of deep second degree burn. Tianjin Med J 2014.
- Memeo A, Verdoni F, De Bartolomeo O, Albisetti W, Pedretti L. A new way to treat forearm post-traumatic non-union in young patients with intramedullary nailing and platelet-rich plasma. Injury 2014; 45: 418-423.
- Huang J. The application of platelet-rich plasma (PRP) in bone nonunion in 19 clinical cases. Zhejiang J Integrat Traditional Chinese West Med 2015.
- Yilmaz S, Kabadayi C, Ipci SD, Cakar G, Kuru B. Treatment of intrabony periodontal defects with platelet-rich plasma versus platelet-poor plasma combined with a bovine-derived xenograft: a controlled clinical trial. J Periodontol 2011; 82: 837-844.
- van Hout WM, Mink van der Molen AB, Breugem CC, Koole R, Van Cann EM. Reconstruction of the alveolar cleft: can growth factor-aided tissue engineering replace autologous bone grafting? A literature review and systematic review of results obtained with bone morphogenetic protein-2. Clin Oral Investig 2011; 15: 297-303.
- Wu CC, Chen WH, Zao B, Lai PL, Lin TC, Lo HY, Shieh YH, Wu CH, Deng WP. Regenerative potentials of platelet-rich plasma enhanced by collagen in retrieving pro-inflammatory cytokine-inhibited chondrogenesis. Biomaterials 2011; 32: 5847-5854.
- Carter CA, Jolly DG, Worden CE, Hendren DG, Kane CJ. Platelet-rich plasma gel promotes differentiation and regeneration during equine wound healing. Exp Mol Pathol 2003; 74: 244-255.
- Zhang HH, Zhan ZG. The development of platelet-rich plasma (PRP) and its application in wound healing. Chinese J Curr Adv General Surg 2013; 16: 309-311.
- Chen JM. The application of platelet-rich plasma (PRP) in treating chronic refractory wounds. Lingnan Modern Clin Surg 2013.
- He YP. Analysis the therapeutic efficiency of platelet-rich plasma (PRP) for the treatment of pressure ulcer. China Rural Health 2014.
- Woo SH, Jeong HS, Kim JP, Koh EH, Lee SU, Jin SM, Kim DH, Sohn JH, Lee SH. Favorable vocal fold wound healing induced by platelet-rich plasma injection. Clin Exp Otorhinolaryngol 2014; 7: 47-52.