Research Article - Biomedical Research (2017) Artificial Intelligent Techniques for Bio Medical Signal Processing: Edition-I
Clinical application of bone decompressing needle in knee osteoarthritis
Wanli Yan1, Zhifeng Liang2, Faliang Lin3*1Department of Rehabilitation, Yantai Hospital of Traditional Chinese Medicine, Yantai, PR China
2Emergency Department, the Second People’s Hospital of Dongying, Dongying?PR China
3Department of Rehabilitation, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, PR China
- *Corresponding Author:
- Faliang Lin
Department of Rehabilitation
The Affiliated Yantai Yuhuangding Hospital of Qingdao University, PR China
Accepted date: March 08, 2017
Abstract
Objectives: Anterior knee pain is an important problem for patients with Osteoarthritis (OA) of knee, and there is urgent demand for surgery treatment in these patients. The aim of this study was to explore the effects of core decompression in the treatment of knee osteoarthritis.
Methods: A total of 120 patients with knee osteoarthritis, who visited the Department of Chinese Medicine of Nanjing Medical University No.2 Affiliated Hospital or Recovery Center of Yantai Hospital of Traditional Chinese Medicine from January of 2013 to September of 2014, were included in this study. Patients were selected based on strict inclusion criteria, and received bone decompression needle treatment or conventional treatment. Patients were randomized into two groups (n=60). Physical conditions and haemorheological changes of patients were assessed before treatment and 6 weeks after treatment to evaluate the therapeutic responses.
Results: Prior to treatment, there were no significant differences in general characteristics between the two groups. And after treatment, both treatments showed significant improvement in pain, physical function, and overall score (P<0.05). With regard to stiffness, the group that received bone decompression needle treatment demonstrated more prominent improvement than conventional treatment group. While both groups demonstrated improvement in overall score (P<0.05), the decompression needle group exhibited greater improvement in RP and MH. Overall score of decompression needle group was superior to that of normal treatment group (P<0.05).
Conclusions: Treatment with bone decompression needle demonstrated superior effectiveness in alleviating knee osteoarthritis than conventional treatment methods. Bone decompressing needle deserves further promotion and wider application to improve the clinical management of knee osteoarthritis.
Keywords
Knee osteoarthritis, Core decompression, Decompression needle.
Introduction
Knee joint bears the maximum burden of human body, and is prone to disease due to its complex structure [1]. Knee Osteoarthritis (OA) is a devastating disease with chronic progressive degeneration, accompanied by joint pain, stiffness, and deformity [2]. Knee OA has a high incidence rate of 30% among the population over 60 years old [3,4], and accounts for the major reason of labor deprivation of elderly males. Knee OA is a result of abnormal degeneration of knee cartilage. Factors such as mechanical stress, genetic susceptibility, and environmental factors, may contribute to the onset and progression of knee OA [5,6]. Recent studies indicate that bone marrow edema is another contributor of knee osteoarthritis [7]. Bone marrow edema may result in intraosseous hypertension and venous congestion [8], which are major causes of join pain. It is still an urgent clinical need to develop effective regimens to alleviate intraosseous hypertension and venous congestion for the treatment of knee OA.
Knee Degenerative Osteoarthritis known as KDOA is a chronic, degenerative disease often commonly affects the elderly. Although knee joint is the one of the largest joint, it is easy to get damaged due to The knee joint gets damaged easily in spite of being one among the largest joints due to its anatomical structure being in stable. KDOA is first characterized by a change that is degenerative is what first takes place in the subchondral bone of the synovial joint and in the articular cartilage as the first change in KDOA. This results in an impairment that is physiological [9].
Therapies for KDOA that are conventional make use of nonsteroidal anti-inflammatory drugs, glucosamine, an intraarticular injection made with sodium hyaluronate, and surgical treatment. 1). Another way to improve the physical function of the knee and reduce pain thereby improving quality of life is through land-based therapeutic exercise. 2). Exercises and pharmacological therapy also have some benefits when it comes to patients suffering from limited knee pain but however can lead to some adverse effects that can be serious 3). Some conventional therapies that are used now try to bring down pain and physical disability in order to prevent structural failure.
Some constituents of bone marrow can be used to repair cartilage and also in restoring vascularity by injecting into the knee joint. This includes Platelet-Derived Growth Factor (PDGF), Transforming Growth Factor (TGF), Vascular Endothelial Growth Factor (VEGF), Bone Morphogenetic Protein (BMP), and also includes stem cells. An enhanced mention of angiogenesis and a promotion of the synthesis of collagen are made by PDGF and it also for mesenchymal progenitor cells it serves as a chemo-attractant. VEGF is a subfamily of the PDGF which promotes mitosis and migration of the endothelial cells in angiogenesis. TGF-β helps promote the synthesis of fibronectin, osteonectin and collagen which in turn adds to deposition of bone matrix. TGF-β helps the stimulation of the production of cartilage and also moves to the bone through endochondral ossification when injected into long bones. On the other hand, BMP helps stimulate hypertrophy and chondrocyte proliferation. Hematopoietic cells and premature mesenchymal cells that together help in promoting angiogenesis, osteogenesis, vasculogenesis, and also extracellular matrix synthesis are included in bone marrow stem cells [10].
Current methods for treating knee OA are primarily tibial osteotomy and knee arthroplasty [11,12]. Despite their effects in relieving pain, improving physical function, and correcting lower extremity alignment, these two methods are technically demanding procedures [13]. Considering that intramedullary pressure is one of the main causes of knee osteoarthritis, core decompression techniques have been employed to decrease the intramedullary pressure. Core decompression represents a conservative treatment, which preserves the knee and is associated with less surgical complications. Compared with osteotomy and arthroplasty, this procedure is manageable in less stringent conditions. Emerging evidences show that core decompression is effective in treatment of osteonecrosis [14], and improving life quality of patients.
Conventionally, trephine is used as the bone decompression instrument. Trephine has a diameter of 8-10 mm and operation with trephine requires that a cortical incision window be made prior to decompression treatment, thus necessitating strict disinfection. This procedure is associated with long postoperative recovery, and may lead to complications that affect quality of life of patients. Due to this reason, more operative and non-invasive bone decompression techniques are warranted to improve the clinical management of knee OA. Bone decompressing needle is a novel instrument developed for treatment of knee OA. It is only 1.1 to 1.3 mm in diameter [15]. Bone decompressing needle can be used without other devices, greatly facilitating the treatment process. Apart from decreasing the intraosseous pressure, drills made by decompressing needles creates new circulatory path within the bone. Currently, clinical practices using bone decompression needle are emerging in China. However, controlled clinical trials are warranted to demonstrate the benefit of bone compression needle in the prevention and treatment of knee osteoarthritis.
Herein, we carried out a randomized clinical trial to compare the effectiveness of bone decompression needle treatment with conventional decompression treatment in knee osteoarthritis. The result of this study can provide scientific grounds for further application of bone decompression needle.
Literature Review
Since it is generally easily available and possesses a strong and fundamental science in terms of autologous mesenchymal stem cells, such biological therapies have now got increased applications which are to be applied in addressing the orthopedic challenges which are inherent and which have limit to their ability to self-repair and its vascularity. Sampson et al. has reviewed in a concise manner the emergence of mesenchymal stem cell applications which are for various pathologies that are related to the bone which are fractures, avascular necrosis and cartilage [16].
Zhang and Sun further investigated the clinical nursing path combined with the Chinese dialectical nursing on different patients suffering from osteoarthritis of the knee and its effects [17]. A highly Random and controlled trial made on 60 patients with osteoarthritis of the knee who were hospitalized between 2012 and 2013 were taken into consideration. The patients of the control group were given normal and routine care making use of the traditional models and the patients of the experimental group were given Chinese dialectical nursing in addition to routine care. There can be a significant improvement to this method in terms of consciousness of selfcare, its clinical presentation, satisfaction of clinical nursing and also if clinical application was possible.
Zhang conducted an investigation on the needle-warming moxibustion and also the electroacupuncture for various degenerative diseases of the knee joint for which 80 cases of patients suffering from joint disease of the knee which was degenerative were grouped randomly as a treatment group and a control group [18]. The chief points remaining same for both groups which were Neixiyan (EX-LE-4), Xuehai (SP 10), Zusanli (ST 36), Xiliao (EX), Waixiyan (EX-LE-5), and Yinlingquan (SP 9). Some more points were identified in accordance to the differentiation of the syndrome and an observation of its effect was made after a period of 12 days of treatment. This work not only had the function of activating the collaterals and the meridians but also enables promotion of qi and blood, and helped in dissipating dampness and cold and killing pain by subsiding swelling.
The perfusion that was necessary for to the femoral head which can cause necrosis of the bone which is underlying (avascular necrosis) and can lead to both femoral as well as acetabular surface changes when in very advanced stages. There are many different treatments which have been reported in the literature which includes various surgical and non-operative procedures. Along with the standard core decompression, another description of the usage of bone marrow aspirate for the stimulation for a response in healing and grafting of bone which allows immediate weight bearing postoperatively was made by Arbeloa-Gutierrez et al. [19]. The reason behind this work was the description of the core decompression method that was augmented along with a concentrate of bone marrow aspirate and also bone grafting for enabling treatment of early identified femoral head avascular necrosis.
Methods
Study participants
Participants were selected from patients visited Physical Medical Functional Recovery Center of Yantai Hospital of Traditional Chinese Medicine. A total of 120 patients were recruited. Diagnosis of knee osteoarthritis was made according to criteria denoted by Chinese Osteoarthritis Guidelines [20].
Inclusion criteria
Participants eligible for the study must meet all of the following inclusion criteria: a) had recurring knee pain during the recent month; b) had narrowing of joint space indicated by X-ray, or had subchondral bone sclerosis, cyst, osteophyte formation at the joint edge; c) had clear, viscous joint fluid and had a WBC of less than 200/ml; d) were no less than 40 years of age; e) experienced morning stiffness of less than 10 min; f) had bone friction sound during activities. Any case that met criteria a and b, or a, c, e, and f, or a, d, e, and f were diagnosed as knee osteoarthritis. In addition to meeting the above diagnostic criteria, patients included in the clinical study were required to have clear consciousness and stable vital signs.
Exclusion criteria
Patients with any condition listed below were excluded from the study: a) severe heart, lung and kidney disease; b) depression or psychological diseases; c) malignant tumors; d) bleeding tendency; e) other unstable diseases and unwillingness to cooperate.
Withdrawal criteria
Subjects were considered exiting the study if they experienced serious accidents, unable to continue study due to other complications, exited voluntarily, or were unable to complete the courses. Treatments were stopped if patients experienced allergy, severe adverse effects, or severe complications that led to rapid disease exacerbation.
Ethical review and informed consent
This research was conducted in accordance with the Declaration of Helsinki. The benefits and risks of participation in the trial had been explained to each participating patient, legal deputy or witness by the investigators or their designee, and written informed consent were obtained before the clinical study. The informed consent with the signature of the patient, legal deputy and person who explained the benefits or risks were preserved by medical staff related with this study.
Randomization and treatment procedure
The 120 patients included in the study were equally randomized into two groups (conventional treatment group, i.e. CT group, and decompression needle group i.e. DN group) using the random number table method.
For conventional treatment group, patients received oral administration of anti-inflammatory drugs and placebos, injected with sodium hyaluronate, and treated with conventional surgical instruments. During surgical treatment, trephine was inserted on the outer or upper 1 cm position of the left tibial tubercle. Local anesthesia was performed with 2% lidocaine. Patients adopted supine position during the operation. Iodine was used to disinfect knee joint. After treatment, Chinese medicine decoction (Raw Astragalus 30 g, Codonopsos 25 g, BiXie 30 g, Zeeland 25 g, Achranthes bidentate 20 g, Eucommia 20 g, Millettia 30 g, Full Angelica 30 g, Tuckahoe 20 g, Citrus 10 g, Aconite 10 g, Asarum 3 g; boiled in water) were given to patients daily. Skin was opened with type II knife, which was also used to sequentially release pressure at positions of knee lateral collateral ligament, medial and lateral support band, infrapatellar bursa, paterllar fat pad, synovial hyperplasia adhesions and contractures. If the patella bursa, and quadriceps show hyperplasic adhesions and contracture. The treatment was done once other week, and a course consisted of three treatments.
For decompression needle group, bone decompression needles were applied in addition to conventional treatments. Briefly, during treatments, patients remained supine with diseased knee exposed and covered by disinfected towels. Needles were inserted around the left tibial tubercle (at 1 cm of the outer left side, and 1/3 lower than patella). With patients under local anesthesia (in the deep periosteum) with 2% lidocaine, surgeons used their left hand to fixate the knee, right hand holding the T-bone needle and piecing into cancellous region of bone with rotation. Piecing boundaries were defined as the opposite side of the bone. Immediately after the needle was withdrawn, a syringe equipped with a 20 ml sterile needle was inserted to the opened position, followed by blood draw. Pressure was enforced on the wounded area for 1-2 min, and patch was applied. If no blood could be drawn after adjusting needle position for several times, this position was considered not suitable for decompression therapy. The treatment was also undertaken once other week, with 3 times being one course.
Clinical effects assessment by physical performance evaluation
The Western Ontario and McMaster Universities Arthritis Index (WOMAC) [21] was used to evaluate the physical performance of patients. This method evaluates knee joint structure and physiology through pain, stiffness, and joint function. It includes 24 items (5 for pain, 2 for stiffness, and 17 for joint function), covering almost all general symptoms and vital signs. According to WOMAC, the Therapeutic Index (TI) can be calculated as: (S_pre-S_post)/S_pre × 100%, where Spre and Spost represent scores of pre-treatment and posttreatment, respectively. For TI of over 80%, treatment was regarded to induce full recovery; for 50%< TI<80%, treatment was regarded as very effective; for 25%< TI<50%, treatment was regarded as effective; TI<25% was regarded as ineffective.
Quality of life
The life quality evaluation was performed using SF-36 evaluation method [22]. The higher score patients had according to the SF-36 standard, the better life quality patients had. SF-36 method contains 26 items, including: physical functioning (PF); role limitations due to physical health problems (RP); Bodily Pain (BP); General Health Perceptions (GH); Vitality (VT); Social Functioning (SF); role limitations due to emotional problems (RE); and Mental Health (MH) [22]. Every item consisted of several questions, totalling 35 questions. Another aspect of health evaluation was health selfassessment, which was analysed independently.
Haemorheological analysis
Blood sample of each patients in this study were collected before and. Haemorheological data were analysed including Whole Blood Viscosity (WBV), Plasma Viscosity (PV), Hematokrit (HCT), and Erythrocyte Sedimentation Rate (ESR).
Data collection and processing
Two groups were compared in terms of general characteristics to ensure they did not differ significantly. Thorough evaluations were made before and 6 weeks after treatment, to evaluate patient responses. Data from two groups were analysed according to the identical criteria. One medical staff was assigned for data collection and evaluation.
Statistical analysis
Statistical analysis was performed using SPSS19.0. All data were represented as Mean ± SD. Percentage was mostly used for numbers. F-test were used for comparing two groups (if the standard error was not even, Kruskal-Wallis H-test was used). Paired comparison between two groups was tested using LSD method. Parameters of pre-treatment and post-treatment were compared using paired t-test or Wilcoxon paired test. Comparison between categories were made using χ2 test.
Results
General information of patients
To ensure that the two groups did not differ significantly in overall physical properties, two groups were compared in terms of gender, menopause, stress, wound history, treatment history, complications, KL grade, age, weight, etc., the two groups did not show difference (P>0.05), except height (P<0.05) (Tables 1 and 2). Height is not supposed to affect the treatment result. Thus, the two groups were suitable for further analysis.
| CT group | DN group | Total number | χ2 | P | ||
|---|---|---|---|---|---|---|
| Gender | Male | 39 | 39 | 78 | 0 | 1 |
| Female | 21 | 21 | 42 | |||
| Menopause | No | 38 | 36 | 74 | 1.054 | 0.305 |
| Yes | 1 | 3 | 4 | |||
| Stress | Low | 37 | 34 | 71 | 0.310 | 0.577 |
| High | 23 | 26 | 49 | |||
| Wound history | No | 58 | 54 | 112 | 2.143 | 0.143 |
| Yes | 2 | 6 | 8 | |||
| Treatment history | No | 41 | 33 | 74 | 2.256 | 0.133 |
| Yes | 19 | 27 | 46 | |||
| Complications | No | 56 | 58 | 114 | 0.702 | 0.402 |
| Yes | 4 | 2 | 6 | |||
| KL grade | I | 5 | 10 | 15 | 5.93 | 0.1149 |
| II | 41 | 28 | 69 | |||
| III | 13 | 20 | 33 | |||
| IV | 1 | 2 | 3 |
Table 1: General information of the patients (part 1).
| CT group | DN group | t | P | |
|---|---|---|---|---|
| Height | 166.93 ± 7.11 | 163.50 ± 9.69 | 2.21 | 0.03 |
| Weight | 63.28 ± 11.08 | 60.73 ± 11.05 | 1.26 | 0.21 |
| Age | 57.46 ± 9.82 | 55.52 ± 11.73 | 0.99 | 0.33 |
Table 2: General information of the patients (part 2) (Mean ± SD).
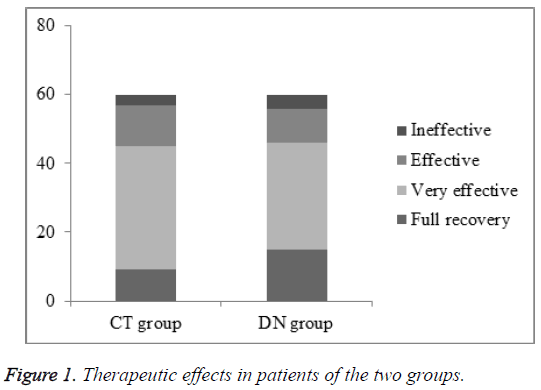
Therapeutic effects in patients assessed by physical performance evaluation
As shown in Figure 1, the recovery rate of DN group was higher than that of CT group (15% in CT group and 25% in DN group, χ2=5.395, P<0.05) but there were no significant difference between the total efficiency rate of each group, the total efficiency rates were 95% and 93% in CT and DN group, respectively (P>0.05).
The osteoarthritis condition of two groups was compared using WOMAC. It turned out that the two groups did not show significant differences in terms of pain, stiffness, and physiological function (P>0.05). Thus, the two groups should be comparable.
To evaluate the treatment efficacy, parameters before and after treatment were compared within each group. As shown in Table 3, all parameters demonstrated a decrease in both groups, suggesting that both conventional and bone needle decompression exerted ameliorating effects (P<0.05). Furthermore, at the end of the treatment, inter-group comparison was made. While needle decompression did not show significant improvement in terms of pain reduction (P>0.05), it greatly relieved the stiffness from osteoarthritis (P<0.05). In term of physiological function, the two groups did not demonstrate significant differences (P>0.05). However, a greater reduction of the overall score was seen in the group that received needle decompression. Collectively, needle decompression showed higher-ameliorating effect than conventional treatment.
| Time point | CT group | DN group | |
|---|---|---|---|
| Pain | Before treatment | 10.05 ± 4.03 | 9.30 ± 3.12 |
| After treatment | 5.26 ± 1.09* | 4.04 ± 0.68* | |
| Stiffness | Before treatment | 4.65 ± 1.12 | 4.42 ± 1.49 |
| After treatment | 2.46 ± 0.57* | 1.07 ± 0.24*# | |
| Physical function | Before treatment | 31.28 ± 8.04 | 33.19 ± 7.36 |
| After treatment | 23.35 ± 6.28* | 20.16 ± 5.21* | |
| Overall score | Before treatment | 46.73 ± 9.76 | 44.28 ± 10.03 |
| After treatment | 29.15 ± 7.53* | 20.42 ± 6.03*# |
Table 3: WOMAC analysis (Mean ± SD).
SF-36 life quality evaluation
The general life quality of patients in two groups was compared using SF-36 method. Before treatment began, two groups did not differ in terms of all parameters, including PF, RP, BP, GH, VT, SF RE and MH. After treatment, intra-group comparison indicated that significant improvement were seen in PF, RP, BP, GH, VT, and SF (P<0.05) for needle decompression group. However, no significant improvement was seen in conventional treatment group on these parameters (P>0.05). In terms of GH, bone needle decompression led to a significant improvement, which was not seen in conventional treatment group. Taken together, both two groups demonstrated improvement in varying degrees, and bone needle decompression demonstrated prominent efficacy in RP and MH. In support of this, bone needle decompression also resulted in greater efficacy in GH and MH than conventional treatment, despite that other parameters, including PF, RP, BP, VT, SF and RE, did not show much improvement. Needle decompression group demonstrated higher overall score than conventional group (P<0.05).
Haemorheological analysis
As shown in Table 4, before treatment there were no significant differences between each haemorheological parameter of the two groups (P>0.05). After treatment, the inter-group comparison was made in each group, both treatment could improve the haemorheological parameters in OA patients (P<0.05 before vs. after treatment in each group respectively), however, in DN group, the patients revealed better therapeutic efficacy (P<0.05 CT group vs. DN group).
| Group | Time point | WBV | PV | HCT | ESR | |
|---|---|---|---|---|---|---|
| High shear rate (200 s-) | Low shear rate (10 s-) | |||||
| CT group | Before treatment | 19.53 ± 0.26 | 5.21 ± 0.04 | 1.62 ± 0.19 | 0.581 ± 0.08 | 2.648 ± 0.03 |
| After treatment | 16.73 ± 0.36* | 4.27 ± 0.05* | 1.25 ± 0.15* | 0.518 ± 0.07* | 2.018 ± 0.05* | |
| DN group | Before treatment | 19.94 ± 0.31 | 5.42 ± 0.06 | 1.72 ± 0.15 | 0.569 ± 0.04 | 2.653 ± 0.06 |
| After treatment | 12.92 ± 0.24*# | 3.21 ± 0.04*# | 1.01 ± 0.09*# | 0.439 ± 0.07*# | 1.832 ± 0.04*# | |
Table 4: Haemorheological data of patients from different group before and after treatment (Mean ± SD).
Discussions
Due to the pivotal function of the knee, knee OA is most commonly associated with severe clinical symptoms and disability, which significantly affects quality of life. Intraosseous hypertension gives rise to recurring joint pain, such as resting pain, night pain, etc. [23]. It appears as a precursor to diseases of knee, hip and spine. The introduction of intraosseous hypertension opened up a new avenue for diagnosing and treating osteoarthritis-associated pain. Therefore, it is imperative to find ways to prevent or alleviate intraosseous hypertension to improve the clinical management and prognosis of this disease. In the present study, we demonstrated that bone needle decompression treatment exerted significant improvement in knee osteoarthritis as indicated by the greater reduction of stiffness and improvement in life quality, compared with the conventional treatment group.
Bone decompression needle aims at not only reducing intraosseous hypertension, but also improving systemic circulation. Drills made by bone needle provide circulating pathways between marrow canal and subcutaneous region. This treatment strategy inherited the principle in Chinese medicine that muscle and bones must be treated simultaneously, by which therapeutic efficacy can be significantly improved. In fact, the bone needle decompressing method was documented in the ancient Chinese book, Huang Di Neijing [24], which precedes contemporary medicine for more than 2000 years. Importantly, this method stresses the close relationship between muscle and bones to the extent that bone treatment is not confined in the mere treatment for bones: muscle and bones are equally important in treatment of bones. Due to the convenience of operation, with no need for strict sterile environment, medical staff could carry out manual operations under normal disinfection, thereby enabling it to be applied in hospitals of various levels.
Studies have shown that the articular surface incrassated due to the long-existing inflammation on the articular surface, and the incrassated articular surface was vulnerable to suffer from local injury when bearing heavy burden, which might then cause bleeding, inflammatory exudation; inflammatory absorption and adhesion formation might finally lead to increase of blood viscosity, which could further slowdown velocity of blood flow and worsen the disease into a vicious circle [25,26]. Moreover, blood supply obstacles may cause local accumulation of acid metabolites leading to immunoreaction such as release of globulin and coagulation factor-Iby the liver, decrease of charge in erythrocyte and erythrocytes aggregation. Thus, the changes of haemorheological data are closely related to the development of OA patients. In this study, we found that the haemorheological parameters were significantly improved in both groups, while the effects in DN group were more remarkable (Table 4). The mechanism of the effects may be related to the decreased pressure on the local articular surface which may attenuate the local inflammation and finally improve the hemorheology parameters of the patients with OA.
In addition to knee osteoarthritis, the needle decompressing method can also be applied to the treatment of a variety of bone diseases. Granted that the decompression method has been successfully tested in the treatment of osteoarthritis of elbow [27], hip [28], lumbar spinal canal [28], etc., the bone decompression needle method can be applied in the treatment of those diseases. We consider our study the pioneering trial to demonstrate the benefit of bone needle decompression method. Further larger, blinded, randomized trials are necessary to achieve the wider application of this valuable therapy.
Conclusions
Bone needle decompression demonstrated higher efficacy in treating knee osteoarthritis than conventional treatment only. This method could improve the clinical management of knee OA due to its simplicity and convenience of operation.
References
- Burnett RSJ. Patellar resurfacing compared with nonresurfacing in total knee arthroplasty -a concise follow-up of a randomized trial. J Bone Joint Surg Am 2009; 91: 2562-2567.
- Focht BC. Move to improve how knee osteoarthritis patients can use exercise to enhance quality of life. Acsms Health Fitness J 2012; 16: 24-28.
- Felson DT, Naimark A, Anderson J, Kazis L, Castelli W. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 1987; 30: 914-918.
- Cross M, Smith E, Hoy D, Nolte S, Ackerman I. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014; 73: 1323-1330.
- Vincent KR, Conrad BP, Fregly BJ, Vincent HK. The pathophysiology of osteoarthritis: a mechanical perspective on the knee joint. PM R 2012; 4: 3-9.
- Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage 2002; 10: 573-579.
- Collins J. Bone marrow edema: chronic bone marrow lesions of the knee and the association with osteoarthritis. Bull Hosp Joint Dis 2013; 74: 24-36.
- Uchio Y, Ochi M, Adachi N, Nishikori T, Kawasaki K. Intraosseous hypertension and venous congestion in osteonecrosis of the knee. Clin Orthop Relat Res 2001; 217-223.
- Jun S, Park MS, Oh SJ, Lee JH, Gong HM, Lee HJ, Kim JS. Efficacy and safety of miniscalpel acupuncture in knee degenerative osteoarthritis patients: a study protocol for a randomized controlled pilot trial. Korean J Acupunct 2016; 33: 67-74.
- Vad V, Barve R, Linnell E, Harrison J. Knee osteoarthritis treated with percutaneous chondral-bone interface optimization: a pilot trial. Surg Sci 2016; 7: 1.
- Karim AR, Cherian JJ, Jauregui JJ, Pierce T, Mont MA. Osteonecrosis of the knee: review. Ann Transl Med 2015; 3: 6.
- Xue JL. Therapeutic effects of segmental resection and decompression combined with joint prosthesis on continuous knee osteoarthritis. Pak J Med Sci 2014; 30: 1238-1242.
- Yang ZY. Medial compartment decompression by fibular osteotomy to treat medial compartment knee osteoarthritis: a pilot study. Orthopedics 2015; 38: 1110-1114.
- Lieberman JR, Varthi AG, Polkowski GG. Osteonecrosis of the knee-which joint preservation procedures work? J Arthroplasty 2014; 29: 52-56.
- Ziping W. New progress of osteoarthritis bone decompression needle therapy. J Taiwan Chinese Med Sci 2014; 7: 65-72.
- Sampson S, Botto-van Bemden A, Aufiero D. Stem cell therapies for treatment of cartilage and bone disorders: osteoarthritis, avascular necrosis, and non-union fractures. PMR 2015; 7: 26-32.
- Zhang C, Sun C. Role of clinical nursing path combined with traditional Chinese dialectical nursing in the treatment of knee osteoarthritis. Int J Clin Exp Med 2015; 8: 6171.
- Zhang Z. 40 Cases of degenerative knee-joint disease treated by needle-warming moxibustion and electroacupuncture. Int J Clin Acupunct 2015; 24: 80-82.
- Arbeloa GL, Dean CS, Chahla J, Pascual-Garrido C. Core decompression augmented with autologous bone marrow aspiration concentrate for early avascular necrosis of the femoral head. Arthroscopy Techniques 2016; 5: 615-620.
- Guixing Q. Osteoarthritis treatment guidelines. Chinese J Joint Surg 2007; 4: 281-285.
- Bellamy N. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988; 15: 1833-1840.
- Brazier JE, Harper R, Jones NM, Ocathain A, Thomas KJ. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 1992; 305: 160-164.
- Arnoldi CC, Lemperg K, Linderholm H. Intraosseous hypertension and pain in the knee. J Bone Joint Surg Br 1975; 57: 360-363.
- Hongtu W, Huangdi N. Diseases, symptoms, and clinical applications of the Yellow Emperor's canon on internal medicine. New World Press (1st edn.) 1999.
- Ogi N. Short-term effect of fresh disk allograft on the osteoarthrotic sheep temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 1997; 84: 259-264.
- Uchio Y, Ochi M, Adachi N, Nishikori T, Kawasaki K. Intraosseous hypertension and venous congestion in osteonecrosis of the knee. Clin Orthop Relat Res 2001; 217-223.
- Kovachevich R, Steinmann SP. Arthroscopic ulnar nerve decompression in the setting of elbow osteoarthritis. J Hand Surg 2012; 37: 663-668.
- Ganz R, Parvizi J, Beck M, Leunig M, Notzli H. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 112-120.