- Biomedical Research (2015) Volume 26, Issue 4
Clinical application of absorbable anti-adhesive film in tendon repair
Ji-Hong Wang, Lin-Qing Wu, Shang-Fei Jing, Chao-Qian Han, Zeng-Tao Hao, Shu-Zheng Wen
Department of Hand and Microsurgery II, the Second Affiliated Hospital of Inner Mongolia Medical University, Hohhot 010030, China
- Corresponding Author:
- Shu-Zheng Wen
Department of Hand and Microsurgery II
The Second Affiliated Hospital of
Inner Mongolia Medical University
Hohhot 010030, China
Abstract
The aim of this study was to investigate the clinical effect of biologically absorbable antiadhesive film to promote zone II flexor tendon healing and reduce tendon adhesion. Eighty fingers of 67 postoperative patients of zone II flexor tendon repair were randomly divided into two groups: an anti-adhesion film group and a non anti-adhesion film group. After 12 weeks, the VAS method was used to assess the degree of hand pain. TAM standard was used to evaluate functional status of the finger flexor tendon. The Lovett classification method was used to evaluate muscle strength. Twelve weeks after operation, the VAS pain scores of the experimental and control groups were 1.9 ± 1.8 and 2.3 ± 1.9, respectively (P = 0.337). The standard evaluation system of TAM yielded excellent rates of 94.9% and 70.7% for the experiment and control groups, respectively. Significant difference was found between the groups (P = 0.000), with the value for the experimental group being significantly higher than that for the control group. The finger flexor muscle strength recovery to normal incidence rates of the two groups were 100% and 95.1%, respectively, with no significant difference (P = 0.162). In conclusion, anti-adhesive biologically absorbable film promotes zone II flexor tendon healing, prevents tendon adhesion, and improves the autonomic active function of fingers.
Keywords
Medical absorbable film, Flexor tendon, Healing, Postoperative adhesion.
Introduction
Statistics show that tendon injuries are the most common injuries (approximately 30%) for hand surgery with a relatively high disability rate. Thus, studies on tendon injury are important in hand surgery.
Many scholars have conducted considerable research on tendon injury with significant achievements. However, some problems remain unsolved. One such problem is the hand dysfunction caused by the adhesion of the zone II flexor tendon injury after operation.
The application of absorbable film in clinical surgery has significantly increased [1-3]. However, further prospective studies are still needed on the prevention of postoperative tendon adhesion. This prospective randomised study aimed to investigate the application effect of biologically absorbable anti-adhesive film to prevent tendon adhesion.
Materials and methods
Subjects
Sixty-seven adult outpatients, aged 19 to 58 years, who underwent operation for finger flexor tendon injury from December 2010 to April 2013, were included in this study. The mean age of the patients was 38.5 ± 16.4. The actual work was done with 80 fingers from these patients. The sole criterion for inclusion was the flexor tendon injury (zone II concis). The patients filled out a questionnaire with details such as age, gender, profession, reason for injury, mechanism of injury, as well as health state and hand function before injury.
The criteria for exclusion were as follows: patients aged <18 or >60 years, those who have taken cortisol within the past six months (for general or local injury), diabetic, have a broken finger or bone fracture, mentally disturbed and cannot comply with the treatment protocol.
Through the random number table, patients were prospectively, randomly, and double-blindly divided into two groups. One group was the anti-adhesive group, in which biologically absorbable anti-adhesive film was used to prevent tendon adhesion after anastomosis. This group consisted of 20 males and 13 females with the mean age being 36.9 ± 15.8 years. The other group consisting of 34 patients was the control group, in which no anti-adhesive materials or drugs were used. This group had a total of 41 fingers and their mean age was 39.1 ± 17.2. The age and gender constituent ratio of the two groups had no significant difference (P > 0.05). This study was conducted in accordance with the declaration of Helsinki and with approval from the Ethics Committee of Inner Mongolia Medical University. Written informed consent was obtained from all participants.
Surgical method
Under brachial plexus anaesthesia, the same group of surgeons performed surgery on the patients by the following methods: debridement, tendon repair [4], modified Kessler method [5] and tendon suture with 4/0 nylon suture. The broken tendon of the anti-adhesive film group was bandaged with anti-adhesion absorbable film (MAST operation American polylactic acid protective filmfrom MAST, Biosurgery Inc.; San Diego, CA USA). Meanwhile, the broken tendon of the control group was not wrapped with any tendon anti-adhesion material, nor was any drug applied.
After surgery, patients underwent therapy forslight wrist flexion (0° to 50°) [5], metacarpophalangeal (MP) joint flexion, proximal interphalangeal (PIP) joints and distal interphalangeal (DIP) joint straight position. Conventional anti-inflammatory rehydration therapy was also applied to observe wound healing and finger blood. Stitches were removed two weeks after the operation. Patients were kept under gypsum protection for four weeks, after which external fixation was removed. Patients began to perform functional exercises until 12 weeks after the surgery.
Assessment
Wound healing was assessed two weeks after surgery. The visual analogue scale (visual analogue scale, VAS) [3] was used to assess hand pain after 12 weeks. Tendon function was evaluated according to hand surgery of the tendon total active motion (TAM) [3] of the American Association [TAM = the total flexion (MP flexion degree + PIP flexion degree +DIP flexion degree) − the total extension limitation degree (MP extension limits degree + PIP extension limitation degree + DIP extension limitation degree)]. If the TAM was equal to that of a normal finger, the status is excellent. TAM >75% of that of a normal finger is considered good, TAM >50% of that of a normal is considered medium and TAM <50% of that of a normal finger is considered poor. Lovett classification [3] was used to evaluate finger flexor muscle strength.
Statistic analysis
SPSS13.0 software was used for statistical data treatment. Measurement data were recorded as mean±standard deviation, whereas count data were expressed as ratio. The student t test orχ2 test was used to comparethe data between groups, with a test level of α = 0.05.
Results
All wounds of the two groups healed in grade A, with no adverse effect, such as infection, and no palondromic tendon case.
VAS pain score results
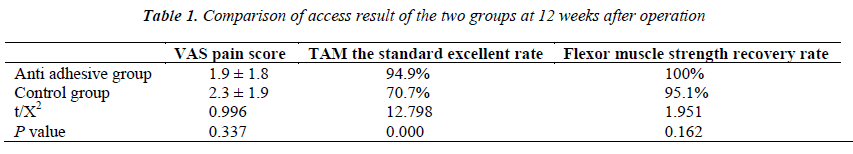
Twelve weeks after operation (Table 1), the VAS pain scores of the anti-adhesive and control groups were 1.9 ± 1.8 and 2.3 ± 1.9, respectively, with no significant difference (t = 0.996, P = 0.337).
TAM Evaluation Result
According to the TAM score criteria, we found two excellent fingers, 35 good fingers, two medium fingers and no poor finger in the anti-adhesive group. Meanwhile, we found no excellent finger, 29 good fingers, 10 medium fingers and two poor fingers in the control group. The excellent rate of the anti-adhesive group was 94.9%, whereas that of the control was 70.7%. The two groups were significantly different (χ2 = 12.798, P = 0.000), with the anti-adhesive group having significantly higher values than the control group.
Lovett classification evaluation results
According to the Lovett classification method, V level muscle strength of the finger flexor was observed in 39 fingers in the anti-adhesive group. The finger flexor muscle strength recovery to normal incidence rates of the two groups were 100% and 95.1% for the anti-adhesive and control groups, respectively, with no significant difference (χ2 = 1.951, P = 0.162).
Discussion
The clinical tendon fracture or defect repair methods being conducted include direct suture, tendon autograft, allograft, xenograft tendon transplantation, and artificial tendon [6-9]. These methods need postoperative routine immobilisation for four weeks (tendon transplantation or even immobilisation longer). However, long-term immobilisation after tendon repair may cause tendon adhesion, which often results in poor recovery of hand function [10]. A considerable proportion of patients must accept the second release operation three months to half-a-year after tendon repair, especially when the flexor tendon in zone II is damaged [11]. Therefore, promoting the healing of tendon repair to reduce incidence rates remains one of the problems related to tendon adhesion. Hand surgeons must thus focus on this matter.
Over the past 10 years the improvement of tendon suture methods enabled doctors and scientists to study biological materials (including sodium hyaluronic acid, chitosan, and collagen membrane) [12-14], growth factors (including insulin-like growth factor, transforming growth factor, and epidermal growth factor) [15], and stem cells [16] for tendon healing. Among these approaches, the application of all kinds of absorbable materials is common in clinical surgery. Biologically absorbable film has ultra-high molecular weight, flexibility and good adhesion, with a physical isolation effect that can separate the operation wound from surrounding tissues and thus prevent fibroblast invasion. The film effectively protects the wound and prevents tissue adhesion, besides being highly biocompatible and easily absorbed without stimulation [17, 18]. Moreover, the selective permeability function of absorbable film enables the entry of synovial fluid and other nutrients to promote endogenous healing of tendon and prevent scar tissue formation thereby preventing tendon adhesion [1, 2].
Oryan et al [19, 20] recently explored the effect of applying absorbable film and sodium hyaluronate on tendon repair. Results showed that when the cast was removed three weeks after surgery, the excellent and good rates of TAM exhibited no statistically significant difference between groups. However, when TAM was measured after eight and 12 weeks, the absorbable film group exhibited better rates than the sodium hyaluronate group. The researchers concluded that absorbable film and sodium hyaluronate can effectively prevent muscle tendon adhesion, but the earlier effect of absorbable film was better than that of the sodium hyaluronate, thus supporting the application of anti-adhesion materials in tendon repair. The study, however, did not use a blind model design. Hanako Nishimoto [21] investigated the application of polylactic acid anti-adhesion membrane in tendon repair. In animal studies, tissues were drawn for morphological analysis four weeks to eight weeks after surgery. The comprehensive excellent rate of the biological anti-adhesion membrane was significantly higher in the anti-adhesion group than in the control group (P < 0.05). Results showed that polylactic acid anti-adhesion membrane can effectively reduce the formation of adhesions after tendon repair. However, the researcher selected the extensor tendon or flexor tendon in the experiment, which meant that the study was un-uniform.
In our study through prospective randomised clinical trial, the clinical effect of absorbable film in treating tendon injury was evaluated. This study also focused on the promotion of healing and reduction of tendon adhesion effect. The subject of research was the zone II flexor tendon only, in a single-blind method, which produced more credible results than the previous study. Results showed that the two groups had no tendon recurrent rupture cases. An evaluation at 12 weeks after surgery showed that the VAS pain score had no statistically significant difference between the anti-adhesion film and control groups (t = 0.996, P = 0.337). The flexor muscle recovery rate had no statistically significant difference (χ2 = 1.951, P = 0.162) between the two groups. However, according to the TAM system evaluation criteria, the difference in the ‘excellent’ and ‘good’ rates of function recovery for the two groups was statistically significant (χ2= 12.798, P = 0.000), with the anti-adhesion film group having significantly better outcome than the control group. Results of this study showed that anti-adhesion film promotes the flexor tendon healing effect, effectively reduces flexor tendon adhesion incidence after anastomosis and improves the active function of fingers.
The mechanism by which absorbable films promote flexor tendon healing is still not entirely clear [22]. This study only clinically observed and evaluated the research subject without MRI radiographic inspection because the subject is part of the living human body, for which histological observation cannot be performed. This is the limitation of this study. In addition, post-operative observation time is relatively short for the long-term follow-up. Further studies should be conducted to analyse whether medical treatment using absorption film has an enhanced functional effect.
Acknowledgements
This research was supported by the Second Affiliated Hospital of Inner Mongolia Medical University.
References
- Liu Y, Skardal A, Shu XZ, Prestwich GD. Prevention ofperitendinous adhesions using a hyaluronan-derived hydrogel film following partial-thickness flexor tendon injury. J Orthop Res 2008; 26:562-569.
- Aoki S, Kinoshita M, Miyazaki H, Saito A, Fujie T,Iwaya K, Takeoka S, Saitoh D. Application of poly-Llactic acidnanosheet as a material for wound dressing. PlastReconstrSurg 2013; 131:236-240.
- Hakimi O, Murphy R, Stachewicz U, Hislop S, Carr AJ. An electrospunpolydioxanone patch for the localization of biological therapies during tendon repair.EurCell Mater 2012; 24:344-357.
- Ozgenel GY, Etöz A. Effects of repetitive injections of hyaluronic acid on peritendinous adhesions after flexor tendon repair: a preliminary randomized, placebocontrolled clinical trial. UlusTravmaAcilCerrahiDerg2012; 18:11-17.
- Tang JB, Chang J, Elliot D, Lalonde DH, Sandow M, Vögelin E. IFSSH Flexor Tendon Committee Report 2014: From the IFSSH Flexor Tendon Committee (Chairman: Jin Bo Tang). J Hand SurgEurVol 2014; 39:107-115.
- Tang JB. Uncommon methods of flexor tendon and tendon-bone repairs and grafting. Hand Clin 2013; 29:215-221.
- Karabekmez FE, Zhao C. Surface treatment of flexortendon autograft and allograft decreases adhesion without an effect of graft cellularity: a pilot study. ClinOrthopRelat Res 2012; 470:2522-2527.
- Rawson S, Cartmell S, Wong J. Suture techniques for tendon repair; a comparative review. Muscles Ligaments Tendons J 2013; 3:220-228.
- Hamido F, Misfer AK, Al Harran H, Khadrawe TA, Soliman A, Talaat A, Awad A, Khairat S. The use of the LARS artificial ligament to augment a short or undersized ACL hamstrings tendon graft. Knee 2011;18:373- 378.
- Starr HM, Snoddy M, Hammond KE, Seiler JG 3rd. Flexor tendon repair rehabilitation protocols: a systematic review. J Hand Surg Am 2013;38:1712-1717.
- James R, Kumbar SG, Laurencin CT, Balian G, Chhabra AB. Tendon tissue engineering: adiposederivedstem cell and GDF-5 mediated regeneration using electrospun matrix systems. Biomed Mater 2011;6:025011.
- de Wit T, de Putter D, Tra WM, Rakhorst HA, van Osch GJ, Hovius SE, van Neck JW. Auto-crosslinkedhyaluronic acid gel accelerates healing of rabbit flexor tendons in vivo. J Orthop Res 2009;27:408-415.
- Bhavsar D, Shettko D, Tenenhaus M. Encircling the tendon repair site with collagen-GAG reduces the formation of postoperative tendon adhesions in a chicken flexor tendon model. J Surg Res 2010;159:765-771.
- Jiang K, Wang Z, Du Q, Yu J, Wang A, Xiong Y. A new TGF-b3 controlled-released chitosan scaffold for tissue engineering synovial sheath. J Biomed Mater Res A 2014;102:801-807.
- Duffy FJ Jr, Seiler JG, Gelberman RH, Hergrueter CA. Growthfactors and canine flexor tendon healing: initial studies in uninjured and repair models. J Hand SurgAm 1995;20:645-649.
- Young RG, Butler DL, Weber W, Caplan AI, Gordon SL, Fink DJ. Use of mesenchymal stem cells in a collagen matrix for Achilles tendon repair. J Orthop Res 1998;16:406-413.
- Sato T, Shimizu H, Beppu M, Takagi M. Effects on bone union and prevention of tendon adhesion by new porous anti-adhesive poly L-lactide-co-e-caprolactonemembrane in a rabbit model. Hand Surg 2013;18:1-10.
- Mentzel M, Hoss H, Keppler P, Ebinger T, Kinzl L,Wachter NJ. The effectiveness of ADCON-T/N, a newanti-adhesion barrier gel, in fresh divisions of the flexor tendons in Zone II. J Hand Surg Br 2000;25:590-592.
- Oryan A, Moshiri A, MeimandiParizi AH, RaayatJahromi A. Repeated administration of exogenousSodium- hyaluronate improved tendonhealing in an in vivo transection model. J Tissue Viability 2012;21:88-102.
- Oryan A, Moshiri A, Meimandiparizi AH. Effects of sodium-hyaluronate and glucosamine-chondroitin sulfateon remodeling stage of tenotomized superficial digital flexor tendonin rabbits: a clinical, histopathological, ultrastructural, andbiomechanical study. Connective Tissue Res 2011;52:329-339.
- Nishimoto H, KokubuT, Inui A, Mifune Y, Nishida K, Fjioka H, Yokota K, Hiwa C, Kurosaka M. Ligament regeneration using an absorbable stent-shaped poly-Llacticacid scaffold in a rabbit model. IntOrthop2012;36:2379-2386.
- Nho JH, Lee TK, Kim BS, Yoon HK, Gong HS, SuhYS.Closed rupture of flexor tendon by hyperextension mechanism in wrist level (zone V): a report of three cases. Arch Orthop Trauma Surg 2013;133:1029-1032.