Research Article - Journal of Clinical Ophthalmology (2020) Volume 4, Issue 1
Choroidal neovascular membrane following vitreoretinal surgery for retinal detachment
Krishna Nagaradh1*, Prarthana Gokarn21Sapthagiri Institute of Medical Sciences and Research Centre, Bengaluru, Karnataka, India
2Narayana Netralaya, Bengaluru, Karnataka, India
- Corresponding Author:
- Dr. Krishna Nagaradh
Sapthagiri Institute of Medical Sciences
and Research Centre Chikkasandra
Chikkabanavara Bengaluru Karnataka, India
E-mail: allwayskrish@gmail.com
Accepted date: January 30, 2020
Citation: Nagaradh K, Gokarn P. Choroidal neovascular membrane following vitreoretinal surgery for retinal detachment. J Clin Ophthalmol 2019;4(1):212-215.
Abstract
Purpose: Choroidal neovascular membrane can arise secondary to many other causes other than aging. No cases have been reported on CNVM post vitrectomy for retinal detachment. We present two cases of classical sub-foveal CNVM occurring following VR surgery in retinal detachment patients.
Method: A retrospective analysis of databases was done at our centre. Around 800 VR surgeries were done of which 300 were macular surgeries over a period 3 years from 2014 to 2017. All cases were operated by a single surgeon with 3 port 23- gauge vitrectomy. Two cases of retinal detachment developed CNVM after silicon oil removal.
Results: The prevalence of CNVM formation after macular surgery at our institution was 2 out of 300 (0.66%) patients from a period of Jan 2015 to Dec 2018. The time period for the formation of CNVM was around 7 months after vitrectomy and 2 weeks after Silicon oil removal in both patients.
Discussion: After all the literature search for knowing the reported cases and the pathophysiology for CNVM occurring post Retinal detachment surgery we attribute it to post-operative inflammation, silicon oil induced retinal toxicity, weakening of retinal layers and retinal photo toxicity.
Conclusion: Despite the fact that CNV post retinal detachment surgery is rare, we suggest that it must be included in the consent process prior to surgery, as patients should be warned about potential guarded visual outcome. Further research is needed to evaluate the possible mechanisms and risk factors that lead to formation of CNVM after retinal detachment surgery.
Keywords
Choroidal neovascular membrane, Sub Retinal fluid, Pars plana vitrectomy, Retinal detachment.
Introduction
Choroidal neovascular membrane (CNVM) is one of the forms of age related macular degeneration [1]. But it can also arise secondary to many other causes like like inflammation (punctate inner choridopathy, multifocal pigment epitheliopathy, multifocal choroiditis, presumed ocular histoplasmosis syndrome) and hereditary retinal diseases, pathological myopia, trauma, angiod streaks and so on. Amongst many complications of vitreoretinal surgery Choroidal neovascularisation is one of the least common. Very little is found in literature about the CNVM occurring in patients following vitrectomy for macular pathology (hole and ERM) [2-4]. No cases have been reported on CNVM post vitrectomy for retinal detachment. We hereby present two cases of classical sub-foveal CNVM occurring following VR surgery in retinal detachment patients.
Method
A retrospective analysis of databases was done at our centre. Around 800 VR surgeries were done of which 300 were macular surgeries over a period 3 years from 2014 to 2017. All cases were operated by a single surgeon with 3 port 23- guage vitrectomy with settings of 5000 cut rate, 50 to 300 vacuums with endo illuminator (xenon light). As tamponad silicon oil/ C3F8 gas on choice depending on case was used. The two cases presented here met the same surgical protocol. Average exposure to light source (xenon) from endolight and operating microscope in both the cases is about 45 minutes. Endolaser is used to the periphery with no laser being applied in the macular area. No agent was used to stain the vitreous or the ILM during the surgery in both the cases. Internal limiting membrane was not peeled in both the cases. The average time taken for the surgeries is one and half hours (1-2 hrs). Post operatively patients are followed up on first week, third week, 1st month and monthly till the first year.
Our first patient was a 62 year old man who presented to our center with diminution in vision in his right eye. He had previous lasered lattice with holes in the superotemporal quadrant in the same eye. On ophthalmological examination, the best corrected visual acuity was Counting Finger 1 mt in the right and 20/50 in the left eye. Patient is simple myope with -1.5 DS in both eyes. The anterior segments were unremarkable in both eyes. Dilated fundus examination of the left eye was normal, but an inferior retinal detachment was identified in the right eye with macular detachment.
The patient underwent 360 band with inferior segmental buckle with pars plana vitrectomy with sub retinal fluid drainage with endolaser and silicon oil injection. During the surgery, there was no macular trauma and the surgery was uneventful.
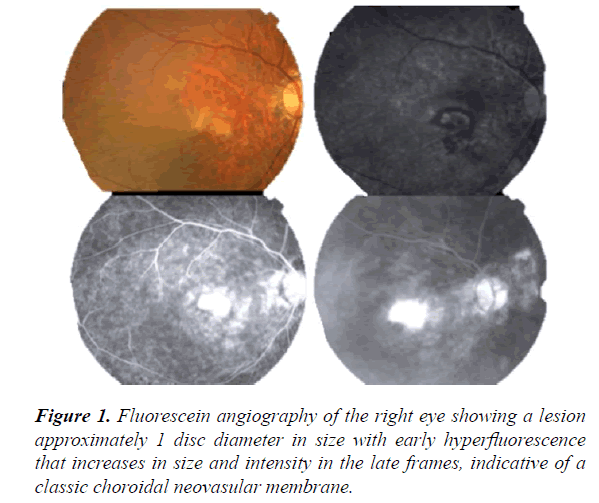
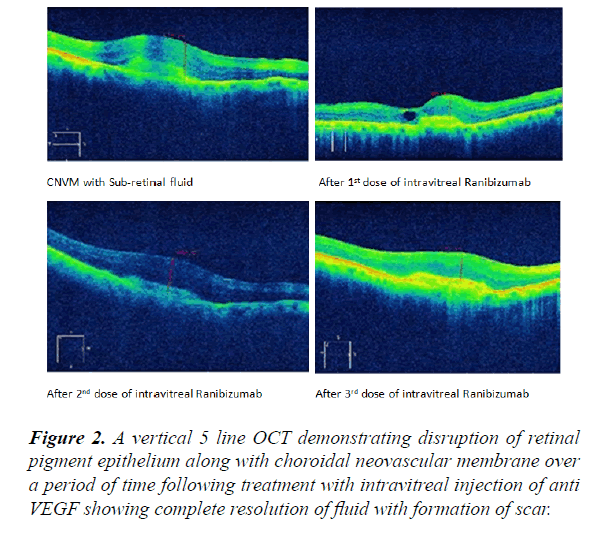
The patient was regularly examined following the surgery and his vision got stabilized at 20/200. Patient underwent silicon oil removal 6 months after surgery the patient’s visual acuity was 20/125, but after 2 weeks of silicon oil removal the patient presented to us with sudden blurring in vision in his right eye with vision of Counting Fingers 3 mts and on examination a serous elevation of the neurosensory retina was noted. CNVM was diagnosed. Fluorescein angiography revealed a classic CNVM (Figure 1). Macular optical coherence tomography (OCT) showed disruption of RPE at the fovea together with the serous detachment (Figure 2).
At that point the patient was treated with 3 doses of intravitreal Ranibizumab injection over a period of 3 months. The sub retinal fluid was resolved and the membrane healed with a sub foveal scar. His vision got stabilized at 20/200.
Our second patient was a male aged 62 years presented with diminution in vision in his right eye 1 month duration. Vision at the time of presentation was Counting finger close to face. On examination a diagnosis of Subtotal retinal detachment with macular detachment and proliferative vitreo retinopathy grade 2 was made and posted for surgery. Patient underwent surgery (360 bandwidth Pars Plana vitrectomy with PVR removal with endolaser with silicon oil injection).
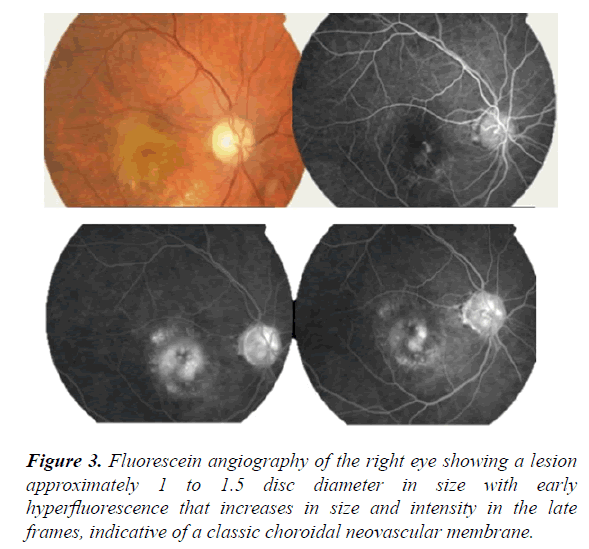
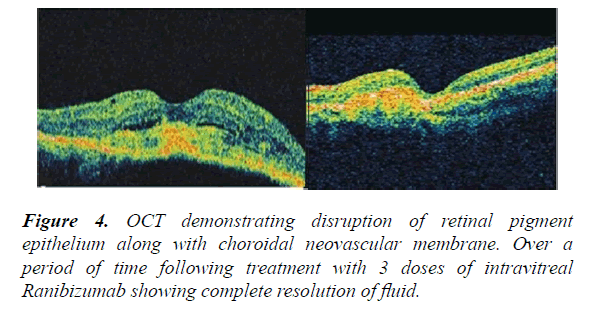
Patient was followed up with frequent visits as advised and silicon oil removal was done after 7 months. Vision recorded after oil removal was 20/125. Patient presented to us with blurred vision after 2 weeks of oil removal. On examination a diagnosis of CNVM was made (Figures 3 and 4). He received anti VEGF injections for the same. Sub-retinal fluid resolved with the formation of a scar.
Results
CNVM confirmed with Fundus angiography (classical) and OCT (Sub foveal) and with no ARMD or Myopic macular degeneration changes pre operatively, the diagnosis of Post vitreo retinal surgery CNVM was made.
The prevalence of CNVM formation after macular surgery at our institution was 2 out of 300 (0.66%) patients from a period of Jan 2015 to Dec 2018. The time period for the formation of CNVM was around 7 months after vitrectomy and 2 weeks after Silicon oil removal in both patients. Preoperatively, both the patients had PVD induced retinal breaks leading to retinal detachment with macular detachment. Both patients underwent vitrectomy without any ILM peel at the time of surgery. Both the patients had no clinical evidence of any form of age related macular degeneration preoperatively. Both patients had no signs of inflammation after silicon oil removal. Both the patients developed sub foveal CNVM. The classification of CNVM, as determined by FA, included both cases of pure classic CNVM. The size of the CNVM, measured in disc diameters, ranged from 1 to 2 disc diameters.
Both patients were treated with anti VEGF injections 3 doses every month for 3 months with complete regression of CNVM with formation of scar and a stable vision in subsequent follow up.
Discussion
A review of literature for CNVM complicating VR surgery revealed seven cases of CNVM following epiretinal membrane peel and the etiology of direct surgical trauma to the bruchs membrane was put forward [5,6].
It was Kelly and Wendel in one of their articles quoted an approximate incidence of 10% of postoperative RPE mottling following macular hole surgery and they attributed it to direct surgical trauma, light toxicity and intra ocular manipulations at the time of surgery. Choroidal neovascular membrane occurring following macular hole surgeries has been reported in 14 eyes [7]. No case of CNVM has been reported till date following retinal detachment surgery and we are reporting 2 cases of CNVM following RD surgery.
After all the literature search for knowing the reported cases and the pathophysiology for CNVM occurring post Retinal detachment surgery we attribute it to the following factors. Firstly post-operative inflammation, as macula was detached in the both the patients, surgery itself might have caused additional oxidative stress on the neurosensory retina and a subclinical weak RPE, leading to VEGF up-regulation and CNVM. The response we got to anti VEGF in both the patients will support this hypothesis [8-10].
Secondly to silicon oil induced retinal toxicity, as our patients had endotamponade with silicone oil for seven long months. Many explanations have been put forward to explain the pathophysiology of the potential toxic effects of silicone. The dissolution of lipophilic macular pigments in silicone oil may render the macula more susceptible to phototoxicity [11-14]. Another theory is the loss of the buffering capacity of vitreous, leading to impaired homeostasis and potassium accumulating in the retina with silicone tamponade. This may cause degeneration of Müller cells [15]. Moreover, the retro-oil fluid contains elevated levels of cytokines, which may affect retinal function by inducing apoptosis and neuronal degeneration, resulting in retinal thinning [16]. Patients in another study on silicon oil use in retinal detachment surgeries showed microcystic edema in the inner nuclear layer and thinning of inner retinal layers [17-19]. In contrast, a more recent study demonstrated that silicone oil caused significant thinning of each retinal layer, not only the inner retinal layers [20]. Both the patients in our study had similar kind of OCT picture with cystic changes in inner nuclear layers and retinal thinning.
Thirdly, the healing process of macula off retinal detachments itself might cause weakening of retinal and choroidal layers leading to CNVM. A recent study by Wakabayashi et al. evaluated the macula's postoperatively in both macula on and macula off RRDs with Fourier domain OCT [10]. Disruption of the photoreceptor inner segment/outer segment (IS/OS) junction line (61%) and the external limiting membrane (24%) was observed only in macula off cases. As both of our cases had macular detachment, RPE function might have been compromised with resulting CNVM.
Fourthly, surgical endolight induced photopic damage to the retina. In practice with all available safety measures the safe exposure time of the posterior pole can be up to 11 minutes. This time limit is still unrealistic in vitreoretinal surgery and macular phototoxic damage remains a factual danger during vitrectomy, even with maximum precautions.
Summary
Very little is found in literature about the CNVM occurring in patients following vitrectomy for macular pathology. Despite the fact that CNV post RD surgery is rare, we suggest that it must be included in the consent process prior to surgery, as patients should be warned about potential guarded visual outcome.
Conclusion
Despite the fact that CNV post retinal detachment surgery is rare, we suggest that it must be included in the consent process prior to surgery, as patients should be warned about potential guarded visual outcome.
Further research is needed to evaluate the possible mechanisms and risk factors that lead to formation of CNVM after retinal detachment surgery.
Financial Interest
None financial disclosures.
Conflicts of Interest
Conflicts of interest none with any of the authors.
References
- Fang X, Chen Z, Weng Y, et al. Surgical outcome after removal of idiopathic macular epiretinal membrane in young patients. Eye (Lond). 2008;22:1430-5.
- Graham K, D’Amico DJ. Postoperative complications of epiretinal membrane surgery. Int Ophthalmol Clin. 2000;40:215-23.
- Warden SM, Pachydaki SI, Christoforidis JB, et al. Choroidal neo- vascularization after epiretinal membrane removal. Arch Ophthal-mol. 2006;124:1652-4.
- Ng EW, Bressler NM, Boyer DS, et al. Iatrogenic choroidal neovascularization occurring in patients undergoing macular surgery. Retina. 2002;22:711-8.
- Korobelnik JF, Dureau P, Sarfati A, et al. Choroidal neovascularization complicating epiretinal membrane removal. Acta Ophthalmol Scand. 1997;75:320-1.
- Micelli Ferrari T, Dammacco R, Quaranta GM, et al. Choroidal neovascularization secondary to vitrectomy for idiopathic epiretinal membrane: report of an unusual case. Eur J Ophthalmol. 2003;13:218-20.
- Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: results of a pilot study. Arch Ophthalmol. 1991;109:654-9.
- Kirkness CM. Do ophthalmic instruments pose a hazard of light induced damage to the eye? In: Cronly-Dillon J, Rosen ES, Marshall J (eds), Hazards of Light; Myths & Realities; Eye and Skin. Oxford: Pergamon Press; 1986:179-186.
- Michael R, Wegener A. Estimation of safe exposure time from an ophthalmic operating microscope with regard to ultraviolet radiation and blue-light hazards to the eye. J Opt Soc Am A Opt Image Sci Vis. 2004;21:1388-92.
- Wakabayashi T, Oshima Y, Fujimoto H, et al. Foveal microstructure and visual acuity after retinal detachment repair. Imaging analysis by Fourier domain optical coherence tomography. Ophthalmology. 2009;116:519-28.
- Herbert EN, Habib M, Steel D, et al. Central scotoma associated with intraocular silicone oil tamponade develops before oil removal. Graefes Arch Clin Exp Ophthalmol. 2006;244:248-52.
- Refojo MF, Leong FL, Chung H, et al. Extraction of retinol and cholesterol by intraocular silicone oils. Ophthalmology. 1988;95:614-18.
- Pastor JC, Del Nozal MJ, Marinero P, et al. Concentraciones de colesterol, alfa-tocoferol y retinoides en aceite de silicona tras su utilizaciσn como sustitutivo vνtreo. Archivos de la Sociedad Española de Oftalmología. 2006;81:13-19.
- Williams PD, Fuller CG, Scott IU, et al. Vision loss associated with the use and removal of intraocular silicone oil. Clin Ophthalmol. 2008;2:955-959.
- Winter M, Eberhardt W, Scholz C, et al. Failure of potassium siphoning by Muller cells: a new hypothesis of perfluorocarbon liquid-induced retinopathy. Invest Ophthalmol Vis Sci. 2000;41;256-61.
- Asaria RH, Kon CH, Bunce C, et al. Silicone oil concentrates fibrogenic growth factors in the retro-oil fluid. Br J Ophthalmol. 2004;88:1439-42.
- Scheerlinck LM, Schellekens PA, Liem AT, et al. Incidence, risk factors, and clinical characteristics of unexplained visual loss after intraocular silicone oil for macula-on retinal detachment. Retina. 2016;36:342-50.
- Shalchi Z, Mahroo OA, Shunmugam M, et al. Spectral domain optical coherence tomography findings in long-term silicone oil-related visual loss. Retina. 2015;35:555-63.
- Christensen UC, la Cour M. Visual loss after use of intraocular silicone oil associated with thinning of inner retinal layers. Acta Ophthalmol. 2012;90:733-7.
- Lee SH, Han JW, Byeon SH, et al. Retinal layer segmentation after silicone oil or gas tamponade for macula-on retinal detachmentusing optical coherence tomography. Retina. 2018;38:310-9.