Letter to Editor - Current Pediatric Research (2018) Volume 22, Issue 2
Chediak-Higashi syndrome-A few comments.
Javad Ghaffari*Professor, Department of Allergy and Clinical Immunology, Mazandaran University of Medical Sciences, Sari, Iran.
- Corresponding Author:
- Javad Ghaffari
Department of Allergy and Clinical Immunology
Molecular and Cellular Research Center, Faculty of Medicine
Mazandaran University of Medical Sciences, Sari, Iran
Tel: +98-11-3340518
Email: javadneg@yahoo.com
Accepted date: July 10th, 2018
Keywords
Chediak-higashi syndrome, Pediatrics, Piebaldism, Immunologic deficiency syndromes.
Letter to Editor
Arulappan et al. [1] reported a case of Chediak-Higashi syndrome (7 years old male) that died due to sepsis. I have added more comments about Chediak-higashi syndrome (CHS).
CHS (CHS; MIM #214500) is relatively a rare immunodeficiency disease (autosomal recessive) which is associated with recurrent infections, occulocutaneous albinismphotophobia, progressive neurologic abnormalities, horizontal and rotatory nystagmus and bleeding tendency due to platelet dysfunction [2]. The exact prevalence and incidence of CHS is not clear. Not more than 500 cases have been report in the world. LYST or CHS1 gene of CHS get localized to bands 1q42-43. Most mutations are null or nonsense mutations. Neutropenia is common in CHS. Neutrophils, monocytes and natural killer cells function and chemotaxis are impaired.
Hypergammaglobulinemia due to frequent infections is common. Giant azurophilic granules of granulocytes on the peripheral blood smear can be diagnosis of CHS. Genetic testing for mutations of CHS1/LYST gene plays an important role in CHS diagnosis. Prenatally by examining amniotic or chorionic villus cells and examination of a fetal blood sample or hair from a scalp biopsy is useful in diagnosing CHS. Inactive and live vaccines of bacteria and virus both are recommended in CHS and are not contraindicated [2]. Without transplantation, most of the patients with CHS die before seven to eight years of age due to pyogenic infection.
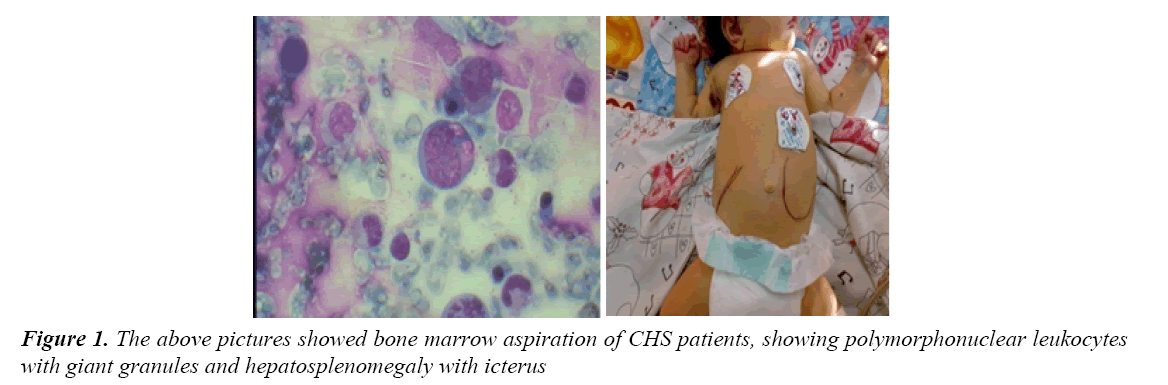
We have reported few cases of CHS at different ages including; 18 months girl, 2 month's age girl and 23 month`s age boy. Our second case (2 months girl) presented with hemophagocytic lymphohistiocytosis and accelerated phase. Her clinical manifestations were high fever, bleeding tendency, hepatosplenomegaly, tachypnea, respiratory disteress, poor feeding, low sucking reflex and pancytopenia [3,4]. Peripheral blood smear (PBS) and bone marrow aspiration showed giant granules. Her hair and skin were not in silvery color (Figure 1). Laboratory tests of that patient include; WBC=2100/L , Hb=7.2 gr/ dL , Plt=11000/microliter, SGOT=54/L, SGPT=320/L, Na=132 mEq/L, K=5.2mEq/L, BUN=44 mg/dl, Urine culture=negative, Urine analysis=normal, Creatinine=1.3 mg/dL, Blood culture=negative, total bilirubin=14 mg/ dL with direct=7mg/dL. Their parents were normal and healthy. She died after 10 days despite chemotherapy (cyclosporine, etoposide and steroids) with antibiotic and supportive therapies. Another case had hypopigmentation of the skin, eye and hair along with recurrent infections. The choice of treatment for CHS is allogeneic Hematopoietic stem cell transplantation (HSCT)) especially for the accelerated phase. Cord blood transplantation was also an effective treatment of accelerated phase of CHS [5]. About 50% to 80% of patients eventually enter an accelerated phase.
Ascorbic acid also can be effective in treatment of CHS. High-dose glucocorticoids, splenectomy, intravenous gammaglobulin, antiviral drugs and chemotherapy (eg, etoposide, methotrexate, and vincristine) can be used to slow the accelerated phase. Differential diagnosis of CHS is Griscelli syndrome, Oculocutaneous albinism, Hermansky Pudlak syndrome.
In conclusion, CHS is not a common disorder with varied spectrum of clinical manifestations. Finding of large granules in leukocytes in the peripheral blood smear or bone marrow aspiration should raise the possibility of CHS. Prophylactic antibiotics and aggressive therapy for acute bacterial infections is considered in CHS. Hematopoietic cell transplantation (HCT) is the treatment of choice of CHS.
References
- Arulappan J, Thomas DSH, Wali YA, et al. A child with Chediak-Higashi syndrome-A case study. Curr Pediatr Res 2018; 22: 69-72.
- Ghaffari J, Rezaee SA, Gharagozlou M. Chediak–Higashi syndrome. Journal of Pediatrics Review 2013; 1: 80-87.
- Ghaffari J, Karami H, Ghasemi M, et al. Chediak-Higashi syndrome, Report a case. J Babol Univ Med Sci 2010; 12: 79-84.
- Ghaffari J, Abediannkenari S, Rezaii MS. Chediak-Higashi syndrome: A report of three cases from the North of Iran. Pak J Med Res 2014; 53: 49-53.
- Zhang Y, Gao Z, Yu X. A case of Chediak-Higashi syndrome presented with accelerated phase could be treated effectively by unrelated cord blood transplantation. Pediatr Transplant 2017; 21.