Research Paper - Archives of General Internal Medicine (2017) Volume 1, Issue 4
Changing Trends in Etiology of Pancytopenia-our Experience
Mohanty Bijaya*, Singh Reetu and Prasad Satish
Department of Medicine, Tata Main Hospital, Jamshedpur, India
- *Corresponding Author:
- Bijaya Mohanty
Department of Medicine
Tata Main Hospital
Jamshedpur, India
E-mail: bijayamohantytmh@gmail.com
Accepted on September 04, 2017
Citation: Bijaya M, Reetu S, Satish P. Changing trends in etiology of pancytopenia-our experience. Arch Gen Intern Med. 2017;1(4):1-6
Abstract
Introduction: Pancytopenia is actually a triad of laboratory findings comprising of anemia, leucopenia and thrombocytopenia due to reduction of these elements below the reference value. Usually pancytopenia occurs in serious and life threatening illnesses including malignancy but is not uncommon in benign conditions like drug induced bone marrow hypoplasia, megaloblastic anemia etc. Management and the prognosis of these patients depend on the underlying etiology. So it is important to identify the correct etiology in all cases which is the cornerstone in implementation of appropriate management. The aim of this study was to assess the clinical profile of patients with pancytopenia and to determine the etiology along with comparing our findings with those of other similar studies. Material and methods: This is a prospective study of hundred cases of pancytopenia admitted to different medical wards of Tata Main Hospital, Jamshedpur a teaching institute and a secondary care hospital in Jharkhand, India over a period of twelve months (April 2014-March 2015). All adult patients of both sex with provisional diagnosis of pancytopenia was taken in to the study group the parameters being haemoglobin value less than 10 gm/dl, total leucocyte count less than 4000/cu mm and platelet count less than 100,000/cumm. Complete medical history was documented in all patients. Detailed general and systemic examinations were carried out. Total haematological work up was done including bone marrow aspiration and trephine biopsy. Other investigations like serum protein electrophoresis, ultrasonography of abdomen and pelvis etc were also carried out where ever indicated. The data was compiled and analyzed. Observation and Result: Out of 100 cases 56 cases were female and 44 were male. Age varied between 14-84 years. Most common symptoms in our series were nonspecific, weakness accounting to 70% of cases. Fever of varying degree was noted in 51%, breathlessness on exertion in 40% and 22% presented with complains of bodyache. Bleeding manifestations was observed in 9% of cases. 32% of patients had haemoglobin below 4 gm/dl, 36% had between 4-6 gm/dl and rest presented with haemoglobin above 6 gm/dl. Pancytopenia was due to megaloblastic anaemia in 44% of cases in our series where as 24% had dimorphic picture. 8% of cases were diagnosed to have myelodysplastic syndrome. Nine cases had aplasic anemia. Conclusion: Megaloblastic anaemia is the most common cause of pancytopenia in our series which is similar to studies conducted in other institutions except a few where aplastic anaemia was the commonest etiology. It is a rapidly corrective disorder and should not be missed and should be kept in mind as one of the commonest etiology of pancytopenia.
Keywords
Pancytopenia, Megaloblastic anaemia, Myelodysplastic syndrome, Aplasia, Hypoplasia, Leukaemia.
Introduction
Pancytopenia was not a discrete haematological entity till as late as 1919. The term was used almost synonymously for aplastic anemia, it being the major cause of pancytopenia in Western countries [1]. However in present scenario pancytopenia is an important clinico-haematological problem encountered in our day-to-day clinical practice. It is not a disease by itself. It is a triad of laboratory findings leading to reduction in level of red blood cells, white blood cells and platelets below their normal reference limit leading to anaemia, leucopenia and thrombocytopenia [2,3]. Many serious and life threatening illnesses present with features of pancytopenia including various haematological malignancies like leukaemia, lymphomas, myelodysplastic syndrome and aplastic anaemia. But it is also reported in several benign and treatable conditions like megaloblastic anaemia. Though there is a wide array of etiology leading to the causation of pancytopenia the primary mechanism include either reduction in blood cell production, infiltration of bone marrow by abnormal or malignant cells or ineffective hematopoiesis with cell destruction. Bone marrow suppression is the leading cause in reduction of blood cell production as occurs in aplastic/hypoplastic anaemia. Dys-hematopoiesis with cell destruction may be antibody mediated leading to sequestration of cells in the reticulo-endothelial system specially spleen leading to hypersplenism [2]. A review of literature both Indian and Western shows that there are not many comprehensive studies on this subject from developed world. However extensive studies have been done on various etiological factors like aplastic anemia, megaloblastic anaemia, leukaemia and myelodysplastic syndrome etc [4]. The underlying pathology plays a key role in the management and prognosis of these patients [4]. Identifying the correct etiology is crucial and is the corner stone in implementation of appropriate treatment. The aim of our study is to diagnose the patients with pancytopenia by analyzing the clinico-haematological parameters including bone marrow aspiration and trephine biopsy and finding out the common disease entities responsible for it.
Material and Methods
This is a prospective observational study carried out for twelve months from April 2014 to March 2015 in the Department of internal medicine Tata Main Hospital, a teaching institute and a secondary care hospital catering to both rural and urban population of Jharkhand and part of Odisha, Westbengal and Bihar. Patients admitted for evaluation of anaemia from haematology as well as medicine OPD and from Emergency were screened for pancytopenia and taken in to study group. Written consent was taken from each patient/relative and studied according to predesigned proforma. Approval of Ethics committee of Tata Main Hospital, Jamshedpur was taken.
Hunderd cases of pancytopenia defined by modified degruchy [1] were included in the study group. As per the criteria haemoglobin level must be below 10 gm/dl, total leucocyte count less than 4000/cumm and platelet count lower than 150,000/cumm. Previously diagnosed cases, patients on chemotherapy or radiotherapy, pregnant females, patients with chronic liver disease and chronic kidney disease were excluded from the study.
A pre-designed proforma was prepared to record history, examination details and investigation reports in a systematic manner. All patients were thoroughly examined with special attention on history of prior drug intake, exposure to chemical agents and radiation either by occupational, accidental or by medical treatment. History of recent viral infections, fever, weight loss, bleeding from various sites (gums, nose, mouth, vagina) were noted. Dietary history in detail including on type of food, intake animal products e.g. meat milk, eggs was taken. History of abdominal pain and bowel habits were noted. History of previous blood transfusions were also noted. A detailed meticulous physical examination of every patient was done for pallor, icterus, pedal oedema, mouth ulcers, hepatosplenomegaly, lymphadenopathy, sternal tenderness and gum hypertrophy was done. Evidence of hypersplenism and primary malignancy was searched for wherever necessary.
The laboratory analysis includes Complete Blood Count (CBC) with absolute values which were conducted on an automated blood analyzer. All hematological parameters were obtained. Values of hemoglobin, red blood cell count, total leucocyte count, differential leucocyte count, platelet count, Mean Corpuscular Volume (MCV), Mean Corpuscular Hemoglobin (MCH), Mean Corpuscular Hemoglobin Concentration (MCHC), Packed Cell Volume (PCV) and reticulocyte count were noted and analyzed. Peripheral blood smear examination was done systematically under low, high and oil immersion microscope for RBC morphology-i.e microcytosis, macrocytosis, anisocytosis, poikilocytosis, polychromasia, nucleated red blood cells and presence of inclusions. Differential leucocyte count was done. Neutrophils were studied in detail for defective granulation and hypersegmentation. Platelet count and morphology was also analyzed. Bone marrow aspiration studies along with trephine biopsy were done where ever indicated from anterior superior iliac spine using standard methods and under all aseptic precautions after obtaining written consent from the patient or guardian. The bone marrow aspiration smears and the biopsy sections were studied in detail. As and when required, bone marrow aspiration and bone marrow biopsy slides were stained with Perl's stain, periodic acid Schiff stain, Zeihl–Neelsen stain or Reticulin stain.
Iron profile (serum iron and ferritin), serum folic acid and serum vitamin B12 level was done in all cases. Other investigations were performed as and when indicated which includes erythrocyte sedimentation rate, liver function tests, renal function tests, serological investigations for enteric fever, blood culture, ELISA for HIV, hepatitis B and C viruses and serum protein electrophoresis. Urine examination including, urinary Bence Jones proteins and stool examination was also advised depending on the case. Chest and bone radiographs, abdominal and pelvis ultrasonography were also carried out. The investigative work up being directed by the pancytopenia profile developed by us and the suspected underlying pathology.
All the patients thus selected were investigated in a systematic manner and cause of pancytopenia was ascertained. The data were recorded, tabulated and analyzed on the basis of etiology, clinical and haematological findings. Clinico-pathological correlation was done in all cases before reaching a definitive diagnosis.
Observation and Results
Of the 100 cases studied 56 were female and 44 were male with Male to Female ratio of 3:2. In our series pancytopenia was found to be more common in female in comparison to male population. The age of our patients ranged from 14-84 years, average being 41.3 years. Maximum number of cases (51%) in our study group are below 45 years of age, with majority of cases (34%) occurring between age group of 31-45 years. Generalized weakness was the commonest presentation in our series to the tune of 70%. 51% of cases had complains of low grade irregular fever. Breathlessness on mild to moderate exertion was the key presenting symptom in 40% of cases. 22% of patients had complaints of only bodyache. 9% presented with bleeding manifestations in the form of epistaxis, purpuric spots over the body and gum bleeding. There was no major bleeding in any of our patients. All patients in our study presented with signs of pallor. 21% had splenomegaly and 18% had hepatomegaly. Bony tenderness was found in one case. Icterus was documented in four cases. One patient had multiple lymph node enlargements. There is a wide variation in haemoglobin levels of patients in our study ranging from 1.9 to 9 gm/dl. Of 100 cases 32% had haemoglobin levels below 4 gm/dl, suggesting severe degree of anaemia at the time of presentation. 36% had haemoglobin between 4-6 gm/dl and the rest 32% of cases had haemoglobin above 6 gm/dl. The lowest haemoglobin encountered in our series was 1.9 gm/dl. Total leucocyte count varied between 500-3900 (mean value -2100/cu mm). Total platelet count varied between 12000-100,000 (mean -69000/ cu mm). Majority (46%) of cases had platelet counts between 50,000- 100,000/cu mm. Also 12% had platelet counts below 20,000/cu mm. MCV (mean corpuscular volume) was as high as 145 fentoliter. This high MCV was observed an all cases of megaloblastic anaemia due to vitamin B12 deficiency presenting as pancytopenia, where as it is within normal range in other causes of pancytopenia. Serum iron measured was as low as 12.8. After clinical, biochemical and haematological work up we have diagnosed the etiology of pancytopenia in all cases. In our study 85% of cases had non-malignant disorders responsible for pancytopenia. Out of 100 cases the most common cause of pancytopenia was megaloblastic anaemia of varying severity noted in 44% of cases. Dimorphic anaemia was observed in 24% of cases which reflects features of a combination of both iron deficiency and megaloblastic anaemia in varying proportions due to nutritional deficiency. Patients were treated with both folic acid and parenteral methyl cobalamine therapy. They were closely monitored for clinical and haematological improvement. This group of pancytopenia with megaloblastic anaemia improved dramatically with vitamin B12 supplementation as per the standard therapy protocol.
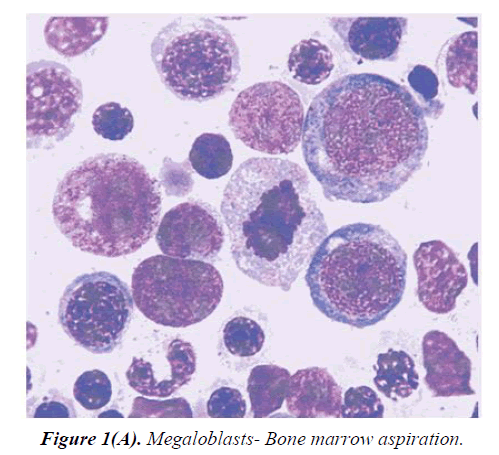
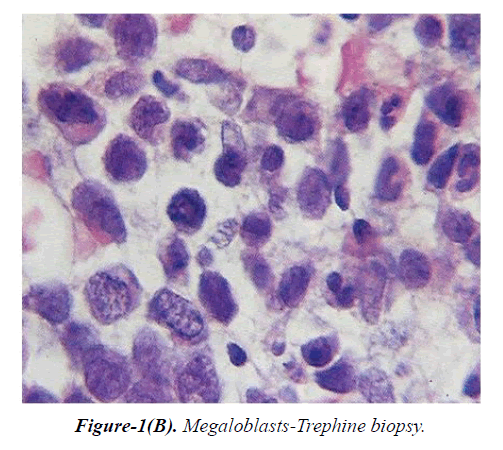
Bone marrow aspiration showed megaloblastic erythroid hyperplasia. Megaloblasts had the characteristics feature of sieved nuclear chromatin, asynchronous nuclear maturation and bluish cytoplasm with cytoplasmic blebs (Figures 1A and 1B). Giant metamyelocytes and band forms were predominant in granulocyte series. Aplastic anaemia was found in 9% of cases in which bone marrow aspiration smear examination showed hypocellular marrow with reduced erythropoiesis, myelopoiesis and megakaryopoiesis. Bone marrow biopsy specimens showed hypocellularity with a predominance of fat spaces and focal hematopoietic activity (hot spots). Myelodysplastic syndrome accounted for 8% of cases. Peripheral blood smear examination in these cases showed macrocytic normochromic anemia, nucleated red blood cells, and immature white blood cells. Bone marrow examination revealed various dysplastic changes affecting different cell lines. In one case increased blast cells were present (11%). Serum Vitamin B12, folic acid, and ferritin levels were normal in these patients. Multiple myeloma was diagnosed in three cases who presented with extreme weakness, varying degrees of bodyache and bony tenderness. Bone marrow examination showed abnormal proliferation of plasma cells, constituting more than 40% of marrow cells, including good number of binucleate and trinucleate forms. Acute leukemias were observed in 3% of cases. We encountered one case of Non- Hodgkins lymphoma. All of these disorders were more common in females than males in our series.
In our series 44% of cases of pancytopenia were found to be due to megaloblastic anaemia, 24% due to dimorphic anaemia and 9 % had aplastic anaemia. Myelodysplastic syndrome was diagnosed in eight cases, multiple myeloma in three cases. Acute leukaemia was diagnosed in three cases and one case had Non-Hodgkins Lymphoma. Majority of cases of pancytopenia in our series belongs to age group of 31-60 years. Aplastic anaemia was found in younger age group between 15-30 years. Myelodysplastic syndrome was detected in patients above sixty years old. Seven cases were diagnosed who were above seventy five year old.
Discussion
We came across cases of pancytopenia quite commonly in our day today clinical practice. This poses a challenge to both physicians and haematologists. Patients of pancytopenia present to us most commonly with features of varying degrees of anaemia followed by infections and bleeding manifestations. There is an exhaustive list of the causes of pancytopenia demanding thorough evaluation. In most of the cases it can be diagnosed by peripheral blood smear examination, bone marrow aspirations and trephine biopsy [5,6]. We have studied 100 cases of pancytopenia and compared our observations with those studies published in the literature. In our study pancytopenia was found to be prevalent more in younger people with age ranging from 14-45 years. Also prevalence rate among females were 56% and that of males 44% with female to male ratio 3:2. This is similar to the study conducted in Karachi by Aziz et al. [7] where 59% of their pancytopenic patients were females’ vs. 41% males. Deepak B Kumar and A R Raghupathi also observed a female preponderance in their series [8]. However another study conducted by Jalbani A [9] showed 72.5% males and 26.1% females with female to male ratio 2.6:1. The exact cause of this gender variation is not clearly understood. May be the males are more exposed to agricultural insecticides and pesticides, or industrial toxins, or radiation depending on their work. On the other hand females also perform jobs almost in every sector along males hence are equally exposed to chemicals and environmental toxins in urban areas.
In present study generalized weakness, fever and breathlessness were the most common clinical features in pancytopenic patients comprising of 70%, 57% and 40% respectively. Similar results have been reported in studies by Pathak et al. [10]. The frequencies of other clinical features were variable and different from these studies probably due to broad spectrum of etiologies behind pancytopenia. After analyzing our data; we feel that the presenting symptoms in pancytopenia patients are usually attributable to anaemia or thrombocytopenia. Leukopenia leading to sepsis is a rare cause of initial presentation but is usually life threatening with increased morbidity and mortality as has been suggested by deGruchy [1]. A wide variety of disorders can cause pancytopenia although the frequency with which each condition is associated with it differs considerably. Table 1 show the various causes of pancytopenia in different studies conducted in different countries.
| Study | Country | Year | No of cases | Commonest cause | Second most common cause |
|---|---|---|---|---|---|
| Tilak and Jain et al. | India | 1999 | 77 | MA (68%) | AA (7.7%) |
| Khodke et al. | India | 2000 | 50 | MA (44%) | AA (14%) |
| Kumar et al. | India | 2001 | 166 | AA (29.5) | MA (22.5%) |
| Jalbani et al. | Pakistan | 2009 | 40 | AA (32%) | HS (22.5%) |
| Aziz et al. | Pakistan | 2010 | 88 | MA (40.9%) | AA (31.9%) |
| Gayathri et al. | India | 2011 | 104 | MA (74.04%) | AA (18.3%) |
| Vandana et al. | India | 2012 | 80 | MA (41.2%) | DA (8.7%) |
| Present study | India | 2015 | 100 | MA (44%) | DA (24%) |
Table 1: Various causes of pancytopenia in different studies. MA-Megaloblastic anaemia, AA-Aplastic anaemia, HS-Hypersplenism, DA-Dimorphic anaemia.
Megaloblastic anaemia was found to be the commonest cause of pancytopenia in most of the studies whereas aplastic anaemia is the second most common etiology. This variation in the etiology causing pancytopenia in different study groups observed may be due to differences in stringency of diagnostic criteria, period of observation, geographic area, nutritional status, prevalence of infective disorders, genetic differences and varying exposure to toxins [11]. Megaloblastic anaemia was the most common cause of pancytopenia in our patients accounting for 44% This is similar with Kumar and Kalra et al. [11] and Gayathri and Satyanarayan Rao et al. [12]. Prevalence of megaloblastic anaemia was as high as 74% by Gayathri in 2011. Megaloblastic anaemia due to vitamin B12 and folate deficiencies is now a well-recognized and established cause of pancytopenia and there is increased health concern about its consequences worldwide [12]. Poor nutrition, avoidance of animal products may be responsible for increased frequency of megaloblastic anaemia. Kumar et al. and Jalbani et al. study in 2009 documented aplastic anaemia as the commonest cause in their series which is in contrast to our series. Most of the studies concluded megaloblastic anaemia as the commonest cause of pancytopenia which is similar to our observation. However the second most common cause in our series was diamorphic anaemia which is in contrast to most of the studies where either aplastic anaemia or hypersplenism was found to be ranked second. Vandana et al. also found diamorphic anaemia to be the second common cause accounting to 8.7% where as we had 24% of cases in our series.
MDS constituted 8% of total cases in our study compared to Khunger et al., where it is reported to be 2% [13-15]. The incidence was even lower (0.96%) in a study conducted by Gayathri and Rao. Multiple myeloma in their series of 104 patients with pancytopenia. 4% of patients with pancytopenia were diagnosed to have multiple myeloma in a study by Khodke et al. vs. 3% in our series. We had one case of NHL and three cases of acute leukaemia in our series. In contrast to our findings, Kumar et al. noted 12% incidence of aleukemic leukemia in their study. Some other causes of pancytopenia reported in various studies by Tilak V, Jain R, Khunger JM, et al. and Gayathri, Rao. Include malaria, hemophagocytic syndrome, Waldenstrom's macroglobulinemia, myelofibrosis, and Niemann-pick disease. Hypersplenism was a major cause of pancytopenia (29.2%) as shown by Jain et al. [16-22] in contrast to our study. Premkumar et al. stated that in contrast to developed countries where pancytopenia is mostly attributed to malignancy or marrow aplasia, infectious diseases such as tuberculosis, leishmaniasis, and HIV constitute important etiologies of pancytopenia in countries like India [12]. Vitamin B12 deficiency was found to be more common than folic acid deficiency in our study which is similar with the results of other studies conducted in India and its neighboring countries [16,17].
The causes of pancytopenia can be ascertained in 97.58% of cases with the help of detailed clinical history, thorough physical examination and systematic investigations as evidenced in study by Senjuti Dasgupta, Prakas K Mandal et al. [21].
Limitation of our Study
1. This study limits the conclusion about the etiology. A prospective study with large sample size and follow up evaluation would have helped to evaluate the various causes better.
2. This is a hospital based small study of a short duration.
Conflict of Interest
Nil
Conclusion
Pancytopenia is a common hematological entity encountered in our day today clinical practice. This should put the physicians on high alert demanding further investigations to look for the possible cause. since the underlying pathology determines the management and prognosis of these patients, identification of the cause is crucial. Pancytopenia and aplastic anaemia are not synonymous anymore as was thought earlier. There is a definite change in trend from aplastic to megaloblastic anaemia over the years. Megaloblastic anaemia is quite common in Indian population possibly due to nutritional factors and is easily reversible with appropriate treatment. Thus megaloblastic anaemia should always be considered in the evaluation of pancytopenia in Indian and other Asian countries. High mean corpuscular volume is a reliable indicator for diagnosis of megaloblastic anaemia. So a complete haemogram showing high MCV almost clinches the diagnosis while evaluating pancytopenia. Poverty, poor eating habits and avoidance of animal products may be the causes of nutritional deficiencies leading to megaloblastic anemia which can be prevented by improving the nutritional status. However other important causes of pancytopenia should be kept in mind while planning investigations for the complete work-up.
References
- Firkin F, Chesterman C, Penington D, et al. editors de Gruchys Clinical haematologyin medical practice 5th edition United States; Blackwell Science 1989.
- Beutler E, Lichtman MA, Coller BS, et al. editors Williams Haematology 6th edition New York; McGraw-Hill publishing company 2001.
- Williams DM. Pancytopenia, aplastic anaemia and pure red cell aplasia in: Wintrobes clinical haematology 10th edition UK: Waverly company. 1993;pp:1449-84.
- Tilak V, Jain R. Pancytopenia-a clinicohaematologic analysis of 77 cases, Indian J Pathol Microbiol. 1999;42:399-404.
- Dodhy MA, Bokhari N, Hayat A, et al. Etiology of pancytopenia; a five year experience. Ann Pak inst Med Sci. Apr-Jun 2005;1(2):92-5.
- Khodke K, Marwah S, Buxi G, et al. Bonemarrow examination in case of pancytopenia- J IndianAca Clin Med. 2001;2:55-9.
- Aziz T, Ali L, Shah S, et al. Pancytopenia: Megaloblastic anaemia is still the commonest cause. Pak J Med Sci. Jan-Mar 2010;26(1):132-6.
- Deepak B Kumar, Raghupati AR. Clinicohaematologic analysis of pancytopenia: Study in a tertiary care centre-Basic and applied pathology. 2012;5:19-21.
- JalbaniA, Ansari IA, Chutto M, et al. Propertion of megaloblastic anaemia in 40 patients with pancytopenia at CMC hospital, Larkana- Medical Channel. 2009;15:34-7.
- Pathak R, Jha A, Sayami G, et al. Evaluation of bone marrow in patients with pancytopenia-J Pathology Nepal. 2012;2:265-71.
- Kumar R, Kalra SP, Kumar H, et al. Pancytopenia- a six year study. J Assoc Physicians India. 2001;49:1078-81.
- Gayathri BN, Kadam Satyanarayan Rao. Pancytopenia: A clinico haematological study-J of Laboratory Physicians. 2011;3(1):15-20.
- Verma N, Dash S. A reappraisal of underlying pathologyin adult patients presenting with pancytopenia-Trop Geogr Med. 1992;44:322-7.
- Raphael V, Khonglah Y, Dey B, et al. Pancytopenia ;an etiological profile, Turk J Hematol. 2012;29:80-81.
- Khunger JM, Arulselvi S, Sharma U, et al. A clinico haematological study of 200 cases. Indian J Pathol Microbiol. 2002;45:375-9.
- Premkumar M, Gupta N, Singh T, et al. Cobalamin and folic Acid status in relation to the etiopathogenesis of pancytopenia in adults at a tertiary care centre in north India. Anemia. 2012;2012:707402.
- Iqbal SP, Kakepoto GN, Iqbal SP. Vitamin B12 deficiency-A major cause of megaloblastic anaemia in patients attending a tertiary care hospital. J Ayub Med Coll Abbottabad. 2009;21:92-4.
- Mahapatra M. Pancytopenia; aplastic anemia. In: Saxena R, Pati HP, Mahapatra M, editors. de Gruchy's Clinical Hematology in Medical Practice. 6th Adapted Edition. Greater Noida: Wiley India Pvt. Ltd. 2013;pp:106-19.
- Das Makheja K, Kumar Maheshwari B, Arain S, et al. Vikash The common causes leading to pancytopenia in patients presenting to tertiary care hospital. Pak J Med Sci. 2013;29:1108-11.
- Pathak R, Jha A, Sayami G. Evaluation of bone marrow in patients with pancytopenia. J Nepal Med Assoc. 2012;2:265-71.
- Senjuti Dasgupta, Prakas K Mandal, Sudipta Chakrabarti. Etiology of Pancytopenia: An Observation from a Referral Medical Institution of Eastern Region of India-J Lab Physicians. 2015;7(2):90-5.
- Jain A, Naniwadekar M. An etiological reappraisal of pancytopenia - largest series reported to date from a single tertiary care teaching hospital. BMC Haematol. 2013;13(1):10.