Research Article - Biomedical Research (2017) Volume 28, Issue 13
Central venous-to-arterial carbon dioxide difference as a useful complementary goal of fluid resuscitation for septic shock patients
Yan Chen, Jian Zhang, Yonggang Tian, Li Zhang, Yahong Li and Lujun Qiao*
Department of Critical Care Medicine, Shengli Oilfield Center Hospital, Dongying City, Shandong Province, PR China
- *Corresponding Author:
- Lujun Qiao
Department of Critical Care Medicine
Shengli Oilfield Center Hospital, PR China
Accepted on May 26, 2017
Abstract
Introduction: Central venous oxygen saturation has inevitable limitation when it serves as a goal of fluid resuscitation. The objective of this study was to assess the capacity of central venous-to-arterial carbon dioxide difference (P(cv-a)CO2) as a complementary marker to guide fluid resuscitation when ScvO2 has reached its threshold in septic shock patients.
Methods: This is a singel-central, observational study of septic shock patient. Patients were randomly divided into two groups with ScvO2 normalized and both ScvO2 and P(cv-a)CO2 normalized as a target of fluid resuscitated respectively. Compared the variables at the beginning of study (T0) and 6 h after fluid resuscitated (T6) for both groups. Lactate clearanc were calculated, and dose of vasoactive drugs, duration of mechanical ventilation and ICU stay and 28-day mortality were recorded.
Results: 68 septic shock patients were included in study. At T0, no defference were found between the two groups. Heart rate and lactic acid decreased significantly at T6 in both groups, but lactate clearance rate of ScvO2+P(cv-a)CO2 group (30.1 ± 17.2) were significantly higher than ScvO2 group (21.6 ± 14.3) (p<0.05). Mechanical ventilation time and duration of ICU stay of ScvO2+P(cv-a)CO2 group were shorter than ScvO2 group (11.7 ± 4.9 days vs. 14.7 ± 6.2 days and 9.3 ± 4.4 days vs. 13.2 ± 6.2 days respectively). No significant difference was observed in 28-days mortality for the two groups.
Conclusion: P(cv-a)CO2 is a valuable complementay goal to guide the fluid resuscitation for septic shock patients. The inclusion of P(cv-a)CO2 into resuscitation protocol would be a safely and effectively practice. But P(cv-a)CO2 may not availably enough to serve as a predictor of prognosis and mortality.
Keywords
Septic shock, Fluid resuseitation, Hemodynamics, P(cv-a)C02.
Introduction
Severe sepsis and septic shock is a life-threatening condition with an incidence of 300 per 100000, and still a common cause of death for patients of intensive care unit (ICU) [1,2]. Promoted practice for septic shock therapy is largely based on a study by Rivers et al. which developed a protocol known as early goal-direeted therapy (EGDT) [3]. EGDT is the key to early treatment of septic shock, which could maintain effective circulating blood volume and improve tissue perfusion. According to Rivers et al. several predefined resuscitation end point should be achieved in EGDT: CVP 8-12 mmHg, MAP 65-90 mmHg, urine output >0.5 mL/kg/hr, mixed venous oxygen saturation (SvO2)>65% or central venous oxygen saturation (ScvO2)>70%, haematocrit>30% [3].
Among those parameters, SvO2 or ScvO2 has been considered as a reliable and sensitive indicator to reflect systemic oxygen supply and demand relationship in septic shock patients, low SvO2 or ScvO2 always indicated unbalance state of tissue oxygen delivery and consumption, and always associated with increased postoperative complications [4,5]. But SvO2 or ScvO2 serves as an estimate of oxygen delivery/uptake relationship are not sufficiently precise to detect tissue hypoxia thus may not efficacious to improve tissue perfusion and metabolism [6,7]. Several studies have reported that EGDT goals achieved and ScvO2 over 70% cannot rule out hypoxic tissue metabolism and hemodynamic abnormalities [8,9]. Recently, some multicenter studies also failed to demostrate ScvO2>70% was effective in septic shock therapy [10,11]. These finding triggers the discussion if ScvO2 alone is accurate enough to guide fluid resuscitation and vasoatctive drugs application effectively. To address the limitation of ScvO2, some candidate parameters such as tissue oxygen saturation [12], lactate clearance [13] and carbon dioxide partial pressure [14] have been investigated as substitutable or complementary target to guide fluid resuscitation.
In recent years, some studies have reported the inverse correlation between mix venous to arterial carbon dioxide differnce (P(v-a)CO2) and cardiac index (CI) in septic patient or non-septic circulatory failure patients [15-17]. Carbon dioxide produced by peripheral tissues is removed by venous blood, therefore the reduced of blood flow and development of anaerabic metabolism could be indicated by elevated P(va) CO2, experimental studies has suggested P(v-a)CO2 could be used as a marker of tissue hypoxia [18,19]. Unfortunately, the measurement of P(v-a)CO2 requires pulmonary artery catherter insertion, which is seldom utilized in clinic today [20]. Central venous-to-arterial carbon dioxide difference (P(cv-a)CO2) as an estimate of P(v-a)CO2, is derived from the insertion of central venous catheter that has been applied to most patients with septic shock [20]. As P(v-a)CO2 potentially represents a more accessible parameter than P(v-a)CO2, P(v-a)CO2 have also been investigated of its possiblility to assess tissue hypoperfusion, Cushieri et al. showed a strong agreement between P(v-a)CO2 and (P(cv-a)CO2), and found (P(cv-a)CO2) and CI also present a negative correlation [21].
Therefore, we aim to investigate the possibility of P(cv-a)CO2 as a useful complementary marker to guide fluid resuscitation when ScvO2 has reach its threshold in septic shock patients, and assess its potential to evaluate the severity of the disease and prognostic of patients in present study.
Materials and Methods
Patients
Patients with septic shock admitted to ICU of Xiangya Hospital Center of Zhongnan University from September 2010 to September 2011 were studied. All patients were diagnosed following the criteria defined by 2001 SCCM/ESICM/ ACCP/ATS/SIS International Sepsis Definitions Conference [22]. All recruitted patients required tracheotomy and assisted breathing with ventilator to improve hypoxia condition. Exclusion creteria were: age under 18, dying or predict death within 24 h; the presence of irreversible underlying disease; underlying heart disease or acute myocardial infarction, cardiogenic shock; patient or family members refused to have the operation; history of renal insufficiency and hemodialysis. All patients were randomly divided into two groups according to different fluid resuscitated goals, ScvO2 group and ScvO2+P(cv-a)CO2group; and all resuscitated prectice were following the international guidelines for management of severe sepsis and septic shock in 2008 [4].
Resuscitation protocol and hemodynamic management
The fluid resuscitated targets of ScvO2+P(cv-a)CO2 group as follow: CVP8~12 mmHg (12~15 mmHg with mechanical ventilation) , MAP ≥ 65 mmHg, urine volume ≥ 0.5 mL/kg/h, ScvO2>70% and P(cv-a)CO2<6 mmHg; and goals of ScvO2 group were the same as ScvO2+P(cv-a)CO2 group except P(cva) CO2 was not monitored and controlled.
When a patient was included in the study, a central venous catheter was inserted with right internal jugular or right subclavian vein approach and a pulse indicator continous cardiac output (PiCCO) catheter was placed in the same time for continuous central venous pressuer (CVP) and ScvO2 monitoring. Blood pressure after invasive and noninvasive opration and arterial blood gas analysis were also monitered. In ScvO2+P(cv-a)CO2 group, P(cv-a)CO2 was calculated every hour. Cultivate blood and/or hematuria and/or phlegm before antibiotics administered. Isotonic crystalloid was administered first to target CVP achieved 8~12 mmHg, if systolic blood pressure less than 80 mmHg, vasoactive drug would be administered at the same time. In any case of CVP decreased, retitration treatment would be adopted, and do not need to deal with the case of CVP higher than upper limit. Second, if CVP achieved 8~12 mmHg but MAP<65 mmHg, 2~20 μg/kg/min dopamine would be administered, and 0.1~2 μg/kg/min norepinephrine would be administered if blood pressure still cannot maintain. Fanally, if CVP achieved 8~12 mmHg and MAP achieved 65~90 mmHg, urine volume ≥ 0.5 mL/kg/h, but ScvO2still lower than 70%, following treatment would be conduct: (1) blood transfusion until haematoerit (HCT)>30%; (2) if HCT>30% but ScvO2<70%, combined with dobutamine (start dose is 3 μg/kg/min, increase by 1~2 μg/kg/min every 10 min, stop admitted when heart rate>150/min); (3) if ScvO2 still cannot reach 70% by increase oxygen supply, treatment that such as cooling, sedative and analgesic could be adopted to lowering oxygen consumption. All goals must be achieved for a maximum of 6 h. For ScvO2+P(cv-a)CO2 group, when P(cva) CO2<6 mmHg, CVP achieved 8~12 mmHg and MAP achieved 65~90 mmHg, urine volume ≥ 0.5 mL/kg/h, ScvO2>70% should maintained in 6 h, if P(cv-a)CO2 ≥ 6 mmHg, adopt retitration therapy.
Blood glucose control within 6~8.3 mmol/L, volume replacement was performed with ringer’s solution and hydroxyethyl starch as appropriate, some patient required to infuse concentrated red blood cells and albumin with crystalloid ratio at 3-4: 1.
Data collection
General information of patient includes sex, age, basic desease, type of disease, Acute Physidogy and Chronic Health Evaluation (APACHE) II score, Sequential Organ Failure Assessment (SOFA) score were collected. Patient's heart rate, respiration, invasive and noninvasive blood pressure, pulse oximetry, OI, CVP, hourly urine output, arterial blood gas analysis, central venous blood gas analysis and other indicators were monitored hourly. Blood lactate concentration, CI, EVLWI, liquid qeuilibrium state were determined in T0 (at the start of the study) and T6 (6 h after inclusion) and calculated lactate clearance by following formula: lactate clearance=(blood lactate at T0-blood lactate at T6)/(blood lactate at T0). Dose of vasoactive drugs (integral dose of norepinephrine and dobutamine) comparison within 6 h, duration of mechanical ventilation, 28 day mortality and ICU stay were also recorded.
Statistical analysis
The data were analyzed using SPSS17.0, all results are presented as mean ± standard deviation. Pairwise comparision of geometric mean were used SNK-q test (student newmankeula, SNK method), analysis of attribute data used chi-square test, P<0.05 was considered statistically significant.
All data were checked by normality test and homogeneity of variance test.
Results
During the study period, a total of 128 patients with septic shock were admitted into the ICU of Xiangya hospital center of Zhongnan University. Among those patient, 60 were excluded according to the following criteria: septic shock over 24 h when enter ICU (n=28), refusal of PiCCO catheter placement (n=12), death within 24 h (n=12), ScvO2<70% after fluid resuscitation (n=8). Finally, 68 patients were eligible for this study. No patients were found complications such as bleeding, infection, pneumothorax, air embolism in puncture site. Basic information was shown in Table 1.
| ScvO2 group (n=30) | ScvO2+P(cv-a)CO2 group (n=38) | P value | |
|---|---|---|---|
| Sex (male/fermale) | 16/14 | 22/16 | p>0.05 |
| Age (years) | 54.1 ± 15.0 | 53.6 ± 14.0 | p>0.05 |
| Infection site | |||
| Lung | 12 | 14 | p>0.05 |
| Enterocoelia | 12 | 14 | p>0.05 |
| Urinary tract | 3 | 5 | p>0.05 |
| Other | 3 | 5 | p>0.05 |
| Basic deseases | |||
| COPD | 8 | 10 | p>0.05 |
| Hematological malignancy | 8 | 10 | p>0.05 |
| Autoimmune disease | 8 | 8 | p>0.05 |
| Diabetes | 3 | 5 | p>0.05 |
| Hypertension | 5 | 6 | p>0.05 |
Table 1. Baseline characteristics of patients.
Comparison between patients in ScvO2 group and ScvO2+P(cv-a)CO2 group at T0
Demographic and clinical characteristics such as sex, age, basic desease and infection site at baseline were similar in the two groups (p>0.05). Before fluid resuscitation practice, there are no significantly defferent in heart rate, MAP, CVP, ScvO2, APACHE II score, SOFA score between the two groups either. As shown in Table 2, lactic acid level of patients in ScvO2+P(cv-a)CO2 group was slightly higher than ScvO2 group patients, but no statistical difference was found between the two groups. Mean arterial pressure of all patients were lower than 60 mmHg, OI lower than 200, CI in both groups were high normal, and MAP, OI, CI, EVLWI and SOFA score have no difference between the two groups (p>0.05).
| T0 | T6 | |
|---|---|---|
| MAP | ||
| ScvO2 group | 53.0 ± 4.9 | 74.7 ±5.3* |
| ScvO2+P(cv-a)CO2 group | 50.6 ± 5.6 | 73.6 ± 13.9* |
| Heart rate | ||
| ScvO2 group | 122.5 ± 18.6 | 108.4 ± 12.5* |
| ScvO2+P(cv-a)CO2 group | 125.3 ± 15.3 | 113.0 ± 11.9* |
| APACHE II score | ||
| ScvO2 group | 20.0 ± 6.0 | 15. 3 ± 4.9* |
| ScvO2+P(cv-a)CO2 group | 19. 5 ± 5.9 | 13.9 ± 5.6* |
| SOFA score | ||
| ScvO2 group | 8.1 ± 1.0 | 5.3 ± 1.8* |
| ScvO2+P(cv-a)CO2 group | 7.7 ± 1.2 | 5.0 ± 1.2* |
| CVP | ||
| ScvO2 group | 3.3 ± 1.9 | 10.1 ± 2.8* |
| ScvO2+P(cv-a)CO2 group | 4.3 + 2.4 | 11.8 + 2.4 *# |
| ScvO2 | ||
| ScvO2 group | 52.3 ± 8.0 | 72.6 ± 3.0* |
| ScvO2+P(cv-a)CO2 group | 51.6 ± 10.0 | 83.2 ± 11.0*# |
| Lactate | ||
| ScvO2 group | 5.3 ± 1.6 | 4.3 ± 1.5* |
| ScvO2+P(cv-a)CO2 group | 5.9 ± 1.7 | 4.1 ± 1.5* |
| Lactate clearance | ||
| ScvO2 group | 21.6 ± 14.3 | |
| ScvO2+P(cv-a)CO2 group | 30.1 ± 17.2# | |
| OI | ||
| ScvO2 group | 132.3 ± 26.5 | 151.4 ± 25.3* |
| ScvO2+P(cv-a)CO2 group | 126.0 ± 22.4 | 150.9 ± 20.4* |
| CI | ||
| ScvO2 group | 4.3 ± 0.8 | 4.5 ± 0.6 |
| ScvO2+P(cv-a)CO2 group | 4.2 ± 0.7 | 5.3 ± 1.0*# |
| EVLWI | ||
| ScvO2 group | 4.9 ± 2.9 | 7.3 ± 3.4* |
| ScvO2+P(cv-a)CO2 group | 4.7 ± 2.7 | 7.6 ± 3.3* |
*Significant difference between T0 and T6 in the same group, P<0.05
#Significant difference between ScvO2+P(cv-a)CO2 group and ScvO2 group, P<0.05
Table 2. Effect evaluation indices of fluid resuscitation at T0 and T6.
Comparison between patients in ScvO2 group and ScvO2+P(cv-a)CO2 group at T6
After fluid resuscitation 6 h, heart rate and lactic acid decreased significantly in both ScvO2+P(cv-a)CO2 and ScvO2 group, and CYP, MAP and ScvO2 increase significantly (p<0.05), but no statistically significant were observed between the two groups (p>0.05). Lactate clearance rate of ScvO2+P(cv-a)CO2 group (30.1 ± 17.2) were higher than ScvO2 group(21.6 ± 14.3) (p<0.05). After 6 h, liquid equilibrium state of ScvO2+P(cv-a)CO2 group (3011 ± 1198) mL were higher than ScvO2 group (2415 ± 680) mL (p<0.05), but vasoactive drug dose were significanly less than ScvO2 group (dose of dobutamine and norepinephrine were (87.8 ± 40.1) mg vs. (111.7 ± 45.1) mg and (13.1 ± 5. 7) mg vs. (16.8 ± 6.0) mg respectively) (p<0.05). After 6 h, CVP and CI of ScvO2+P(cv-a)CO2 group were also higher than ScvO2 group (p<0.01), but incidence of pulmonary edema and EVLWI (12/30) vs. (l4/38) between the two group have no significant difference (p>0.05). After recovery, oxygenation index in both groups were significantly improve, but no difference were found between two groups (p>0.05).
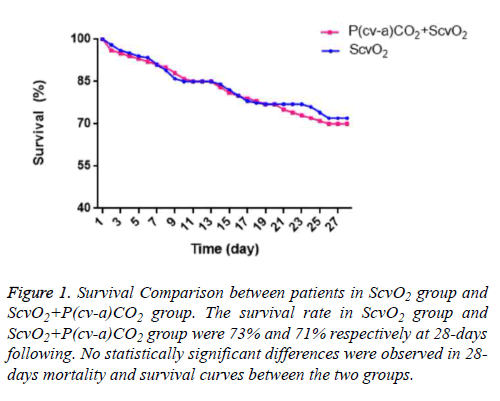
P(cv-a)CO2 and outcome in 28-days following
Results of 28 days follow up shown in Table 3 and Figure 1. Mechanical ventilation time and duration of ICU stay of ScvO2 group were significantly increased than ScvO2+P(cv-a)CO2 group (p<0.05). Eight of 30 patients in ScvO2 group and 11 of 38 patient in ScvO2+P(cv-a)CO2 group death after 28 days, the mortality in 28 days and overall mortality in patients were very close, no significant difference were observed between the two groups. As Figure 1 shows, the survival curves of the two groups were also not found statistically significant difference (p>0.05).
| ScvO2 group | P(cv-a)CO2+ ScvO2 group | t/x2 | P value | |
|---|---|---|---|---|
| Norepinephrine (mg) | 16.8 ± 6.0 | 13.1 ± 5.7 | 0.011 | P<0.05 |
| Dobutamine (mg) | 111.7 ± 4 5.1 | 87.8 ± 40.1 | 0.023 | P<0.05 |
| Fluid balance volume (mL) | 2415 ± 680 | 3011 ± 1198 | 0.017 | P<0.05 |
| Pulmonary edema (%) | 6/30 (20%) | 8/38 (21%) | - | P>0.05 |
| Mechanical ventilation time (day) | 14.7 ± 6.2 | 11.7 ± 4.9 | 0.028 | P<0.05 |
| duration of ICU stay (day) | 13.2 ± 6.2 | 9.3 ± 4.4 | 0.003 | P<0.05 |
| 28 days mortality (%) | 8/30 (27%) | 11/38 (29%) | P>0.05 |
Table 3. Practice in fluid resuscitation and outcomes comparison between ScvO2+P(cv-a)CO2 group and ScvO2 group.
Figure 1: Survival Comparison between patients in ScvO2 group and ScvO2+P(cv-a)CO2 group. The survival rate in ScvO2 group and ScvO2+P(cv-a)CO2 group were 73% and 71% respectively at 28-days following. No statistically significant differences were observed in 28- days mortality and survival curves between the two groups.
Discussion
The main findings of present study are as follows: for fluid resuscitation in patients with septic shock, when ScvO2>70% is achieved, the presence of P(cv-a)CO2 within normal range is relevant to elevated CVP, CI; reduce dose of vasoactive drugs; correlate with higher lactate clearance; and less mechanical ventilation and ICU stay. Therefore P(cv-a)CO2 may be a useful complementary target for EGDT.
P(cv-a)CO2 with better CI and tissue perfusion
Sufficient tissue perfusion is an essential component of oxygenation for patients with septic shock. When oxygen delivery could not reach oxygen demand, it would trigger tissue hypoxia, eventually lead to organ failure [23]. Therefore, the use of early and efficient tool to identify and correct hypoperfusion state is the key for fluid resuscitation practice of patients with septic shock patients, and then improves outcomes. Since the landmark study by Rivers et al. [3], ScvO2 was used as measurement of the balance of oxygen delivery and consumption, and serve as a goal for EGDT. But ScvO2 alone has its limitation as it is measured downstream from tissue [5]. Oxygenation index (OI) basically independent of anaerobic metabolism, in septic condition, capillary shunting and mitochondrial damage will affect tissue oxygen extraction, but the heterogeneity of microcirculation may cover up low local oxygen venous saturation [24,25]. In that case, tissue hypoxia would present while ScvO2 over its threshold, therefore ScvO2 maybe an inaccuracies indicator to reflect the global tissue perfusion. Because the solubility of carbon dioxide is around 20 times than oxygen, carbon dioxide is more likely to spread out of ischemic tissue into veins, making it an extremely sensitive indicator of hypoperfusion [26]. Some studies have confirmed that the increase of CO2 partial pressure is capable to reflect tissue perfusion than other normal indicator (eg, blood lactate) althought its pathophysiology is still unclear [27].
In our study, we have investigatd the potential of P(cv-a)CO2 as a complementary target in fluid resuscitation while ScvO2>70%. By maintaining P(cv-a)CO2 within normal range in a group of septic shock patients that ScvO2 already over 70%, and with another group of patients only normalize ScvO2>70% s a control group, we found that both groups mean arterial pressure and CVP were significantly higher in T6, and heart rate decrease significantly than T0, indicated fluid resuscitation is effective. But CI of patients in ScvO2+P(cva) CO2 group increased significantly than control group, which revealed that P(cv-a)CO2 as a complementary target is beneficial to elevate cardiac output, then improve tissue perfusion.
The normal range of P(cv-a)CO2 is 2~5 mmHg, over 6 mmHg would indicated inadequate cardiac output and tissue hypoperfusion [26]. Althought ScvO2 were higher than 70% in all 30 cases of ScvO2 group, but 12 (40%) patients have P(cva) CO2>6 mmHg, which indicated tissue hypoperfusion of those patients. This is consistent with the reports of Varpuls, and in agreement with reports found that P(cv-a)CO2 have a nagitive relationship with cardiac output [25,28]. And this may contributed to the higher CI of ScvO2+P(cv-a)CO2 group. In other research, patients whose P(cv-a)CO2 over 6 mmHg always present great lactate level than whose P(cv-a)CO2 less than 6 mmHg, and CI, ScvO2 lower than patients that P(cva) CO2<6 mmHg [29]. Insufficient CI would lead to hypoxia because of low flow state, and the shortage of blood flow cannot take CO2 away from tissue, which would elevate P(cva) CO2.
The signifacantly higher blood lactate clearance observed in ScvO2+P(cv-a)CO2 group also support patients in this group reach a better perfusion state. Arterial blood lactate is a sensitive indicator of tissue ischemia and hypoxia, so dynamic monitor of arterial blood lactate is importance for early diagnosis of shock and tissue hypoxia. Oxygen delivery restoration in resuscitation would be indicated by the reduction of blood lactate concentration [30]. Studies have found that a lactate clearance of 10% or more is evidence of adequate tissue oxygen delivery, and serve as an independent predictor of prognosis and survival from septic shock [7,31,32]. In this study, blood lactate in both groups were decrease signifacantly than previous, and lactate clearance of both groups were above 10%, but ScvO2+P(cv-a)CO2 group (30.1% ± 17.2%) have higher lactate clearance than ScvO2 group(21.6% ± 14.3%), indicated ScvO2+P (cv-a)CO2 group could reach a better resuscitation state, and improve body tissue perfusion; while ScvO2 group maybe just reach the lower limit of capacity requirements. Therefore, normalize both P(cv-a)CO2 and ScvO2 may be beneficial to patients with septic shock in aspect of cardiac output and tissue hypoperfusion improvement.
P(cv-a)CO2 and fluid resuscitation practice
By fluid resuscitation, abundance crystal and colloid liquids may be use during early aggressive treatment, which may damage alveolar capillaries, resulting in pulmonary interstitial edema, increased lung damage and even lead to acute respiratory distress syndrome [33]. Extravascular lung water index (EVLWI) is a sensitive indicator of pulmonary oedema, was monitered by PiCCO to assess the degree of pulmonary edema during the early period of fluid resuscitation, reduce the incidence of lung injury. The balance fluid volume of ScvO2 group and ScvO2+P(cv-a)CO2 group was 2415 ± 680 mL and 3011 ± 1198 mL respectively, data shows statistically significant difference. Although patients in ScvO2+P(cv-a)CO2 group received more crystal and colloid fluid than did patients in the ScvO2 group during early aggressive treatment, which may cause acute lung injury, but the slight increased of EVLWI in ScvO2+P(cv-a)CO2 group (7.6 ± 3.3) did not show any significant difference compare with control group (7.3 ± 3.4). The incidence of pulmonary edema in 28-days following (20% vs. 21%) also support more intravenous fluids received in patients of ScvO2+P(cv-a)CO2 group did not cause significant harm to the lungs than control group. In contrast, ScvO2+P(cva) CO2 group (11.7 ± 4.9 days) effectively reduce the duration of mechanical ventilation than control group (14.7 ± 6.2 days). This may be because patients in ScvO2+P(cv-a)CO2 group got adequately fluid resuscitation, cardiac output increased, body tissue perfusion improved effectively, lung perfusion and cell metabolism also improved, fanally shorten the duration of mechanical ventilation. Those datas indicated that normalize both ScvO2 and P(cv-a)CO2 in fluid resuscitation could be practiced safely by balance the demand of cardiac preload and the occur of pulmonary edema.
There are some patients in both group needed dobutamine because of ScvO2 lower than 70%. Dobutamine is an strong agonist for β1 and β2 adrenergic receptor. The active effect to β1 receptor could improve cardiac index by 25% to 50%, and heart rate increase by 10% to 20% [7]. β2 receptor activation could reduce pulmonary wedge pressure and improve cardiac output then improve tissue perfusion [34]. Therefore, dobutamine can increase oxygen delivery but also increase myocardial oxygen consumption. In our study, patients of ScvO2+P(cv-a)CO2 group required less vasoactive drugs than ScvO2 group after fluid resuscitation in 6 h. In consideration of more adequate resuscitation state were receives in patients of ScvO2+P(cv-a)CO2 group, they also enhanced cardiac preload to increase cardiac output, raised effective circulating volume, thereby reducing the amount of vasoactive drugs.
P(cv-a)CO2 with prognosis and mortality
SOFA score and APACHE II score are scoring system commonly used in critically ill patients, for evaluating severity of patients with septic shock and predict prognosis or mortality [35]. Fabrice V point out SOFA score obvious decrease in low P(cv-a)CO2 group patients in 24 h [29] and research from Emmanuel et al. have investigated the use of P (cv-a) CO2 as an individualized goal to guide orientation treatment for 70 high-risk surgical patients, recording the patient's CI, CVP, and P (cv-a)CO2, analyzed their prognosis, found that patients with complications have higher P(cv-a)CO2 value than patients didn’t have complications; for patients whose ScvO2 ≥ 71% and with complications, P(cv-a)CO2 value is significantly higher than patients who without complications occur [36]. Bakker and other studies suggest that surviving septic shock patients have lower P(cv-a)CO2 than the patients who died, although they have a very similar CI, oxygen supply and oxygen consumption values [28]. In this study, SOFA score and APACHE II score have no significant difference between two groups when enter the program, and SOFA score and APACHEII score decreased significantly in T6. But there are also no significant difference in SOFA score and APACHEII score in T6 between the two groups. Although the length of stay in ICU was much shorter in ScvO2+P(cv-a)CO2 group (9.3 ± 4.4 days vs. 13.2 ± 6.2 days), no significant difference were observed in 28 days mortality for the two groups. The 28 days mortality rate in both groups were similar with previous studies [3,11], indicated that the resuscitation practice in our study is effective.
But as a singel-central preliminary research, the studied patients group is small, we may not get sufficient datas to indentify some significant finding. Further multi-center chlinical trials with larger sample are required to comfirm the effective of P(cv-a)CO2 as a complementary goal to guide the fluid resuscitation.
Conclusion
P(cv-a)CO2 is a valuable complementary goal to guide the fluid resuscitation for septic shock patients. The inclusion of P(cv-a)CO2 into resuscitation protocol would be a safely and effectively practice. But P(cv-a)CO2 may not availably enough to serve as a predictor of prognosis and mortality.
References
- Jawad I, Luksic I, Rafnsson SB. Assessing available information on the burden of sepsis: global estimates of incidence, prevalence and mortality. J Global Health 2012; 2: 010404.
- Levy MM, Artigas A, Phillips GS. Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis 2012; 12: 919-924.
- Rivers E, Nguyen B, Havstad S. Early goal-directed therapy in the treatment of severe sepsis and septic shock. New Eng J Med 2001; 345: 1368-1377.
- Dellinger RP, Levy MM, Carlet JM. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Critical Care Med 2008; 36: 296-327.
- Nebout S, Pirracchio R. Should We Monitor ScVO(2) in Critically Ill Patients? Cardiol Res Pract 2012; 2012: 370697.
- Cusack RJ, Rhodes A, Lochhead P. The strong ion gap does not have prognostic value in critically ill patients in a mixed medical/surgical adult ICU. Intensive Care Med 2002; 28: 864-869.
- Nguyen HB, Rivers EP, Knoblich BP. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Critical Care Med 2004; 32: 1637-1642.
- Ladakis C, Myrianthefs P, Karabinis A. Central venous and mixed venous oxygen saturation in critically ill patients. Respiration 2001; 68: 279-285.
- Vallee F, Fourcade O, Marty P. The hemodynamic "target": a visual tool of goal-directed therapy for septic patients. Clinics 2007; 62: 447-454.
- Mouncey PR, Osborn TM, Power GS, Harrison DA, Sadique MZ, Grieve RD, Jahan R, Harvey SE, Bell D, Bion JF, Coats TJ, Singer M, Young JD, Rowan KM; ProMISe Trial Investigators. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med 2015; 372: 1301-1311.
- Peake SL, Delaney A, Bailey M. Goal-directed resuscitation for patients with early septic shock. New Eng J Med 2014; 371: 1496-1506.
- Cohn SM, Nathens AB, Moore FA. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma 2007; 62: 44-54.
- Zhang Z, Xu X. Lactate clearance is a useful biomarker for the prediction of all-cause mortality in critically ill patients: a systematic review and meta-analysis. Critical Care Med 2014; 42: 2118-2125.
- Vallee F, Mateo J, Dubreuil G. Cutaneous ear lobe Pco(2) at 37 degrees C to evaluate microperfusion in patients with septic shock. Chest 2010; 138: 1062-1070.
- Durkin R, Gergits MA, Reed JF. The relationship between the arteriovenous carbon dioxide gradient and cardiac index. J Critical Care 1993; 8: 217-221.
- Mecher CE, Rackow EC, Astiz ME. Venous hypercarbia associated with severe sepsis and systemic hypoperfusion. Critical Care Med 1990; 18: 585-589.
- Rackow EC, Astiz ME, Mecher CE. Increased venous-arterial carbon dioxide tension difference during severe sepsis in rats. Critical Care Med 1994; 22: 121-125.
- Kette F, Weil MH, Gazmuri RJ. Intramyocardial hypercarbic acidosis during cardiac arrest and resuscitation. Critical Care Med 1993; 21: 901-906.
- Zhang H, Vincent JL. Arteriovenous differences in PCO2 and pH are good indicators of critical hypoperfusion. Am Rev Respiratory Dis 1993; 148: 867-871.
- Mallat J, Pepy F, Lemyze M. Central venous-to-arterial carbon dioxide partial pressure difference in early resuscitation from septic shock: a prospective observational study. European J Anaesthesiol 2014; 31: 371-380.
- Neviere R, Chagnon JL, Teboul JL. Small intestine intramucosal PCO(2) and microvascular blood flow during hypoxic and ischemic hypoxia. Critical Care Med 2002; 30: 379-384.
- Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G; SCCM/ESICM/ACCP/ATS/SIS. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003; 31: 1250-1256.
- Donati A, Loggi S, Preiser JC. Goal-directed intraoperative therapy reduces morbidity and length of hospital stay in high-risk surgical patients. Chest 2007; 132: 1817-1824.
- van Beest PA, Hofstra JJ, Schultz MJ, Boerma EC, Spronk PE, Kuiper MA. The incidence of low venous oxygen saturation on admission to the intensive care unit: a multi-center observational study in The Netherlands. Crit Care 2008; 12: R33.
- Varpula M, Karlsson S, Ruokonen E. Mixed venous oxygen saturation cannot be estimated by central venous oxygen saturation in septic shock. Intensive Care Med 2006; 32: 1336-1343.
- Mallat J, Lemyze M, Tronchon L. Use of venous-to-arterial carbon dioxide tension difference to guide resuscitation therapy in septic shock. World J Critical Care Med 2016; 5: 47-56.
- Marik PE, Bankov A. Sublingual capnometry versus traditional markers of tissue oxygenation in critically ill patients. Critical Care Med 2003; 31: 818-822.
- Bakker J, Vincent JL, Gris P. Veno-arterial carbon dioxide gradient in human septic shock. Chest 1992; 101: 509-515.
- Vallee F, Vallet B, Mathe O. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive care medicine 2008; 34: 2218-2225.
- Weil MH, Afifi AA. Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock). Circulation 1970; 41: 989-1001.
- Arnold RC, Shapiro NI, Jones AE. Multicenter study of early lactate clearance as a determinant of survival in patients with presumed sepsis. Shock 2009; 32: 35-39.
- Jones AE, Shapiro NI, Trzeciak S. Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA 2010; 303: 739-746.
- Varpula M, Tallgren M, Saukkonen K. Hemodynamic variables related to outcome in septic shock. Intensive Care Med 2005; 31: 1066-1071.
- Guillamet MC, Rhee C, Patterson AJ. Cardiovascular management of septic shock in 2012. Curr Infect Dis Rep 2012; 14: 493-502.
- Vincent JL, de Mendonca A, Cantraine F. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on "sepsis-related problems" of the European Society of Intensive Care Medicine. Critical Care Med 1998; 26: 1793-1800.
- Futier E, Robin E, Jabaudon M, Guerin R, Petit A, Bazin JE, Constantin JM, Vallet B. Central venous O₂ saturation and venous-to-arterial CO₂ difference as complementary tools for goal-directed therapy during high-risk surgery. Crit Care 2010; 14: R193.