Research Article - Journal of Orthopedic Surgery and Rehabilitation (2023) Volume 7, Issue 5
Cause-effect association of high cervical disc disease with degeneration at craniovertebral junction.
Puram Saikiran*, Mudumba Vijayasaradhi, Rajesh Alugolu, Abhishek Arora
Department of Neurosurgery, Nizams Institiute of Medical Sciences, Hyderabad, India
- Corresponding Author:
- Puram Saikiran
Department of Neurosurgery,
Nizams Institiute of Medical Sciences,
Hyderabad,
India,
E-mail: saikiran.puramsaikiran.puram@gmail.com
Received: 27-Apr-2020, Manuscript No. AAOSR-23-9900; Editor assigned: 30-Apr-2020, PreQC No. AAOSR-23-9900 (PQ); Reviewed: 14-May-2020, QC No. AAOSR-23-9900; Revised: 13-Jul-2023, Manuscript No. AAOSR-23-9900 (R); Published: 10-Aug-2023, DOI: 10.35841/aaosr-7.5.161
Citation: Saikiran P, Vijayasaradhi M, Alugolu R, et al. Cause-effect association of high cervical disc disease with degeneration at properties of craniovertebral junction. J Ortho Sur Reh. 2023;7(5):161.
Abstract
Objective: To analyze the association of High Cervical Disc Degeneration (HCDD) to the presence of Cranio-Vertebral Junction (CVJ) ligamentous calcification.
Methods: The study included 100 consecutive symptomatic cervical PIVD patients who presented to neurosurgery OPD of NIMS, Hyderabad between October 2016 and October 2018. Of these, 70 had C3-4 PIVD (cases) and 30 had C5-6 PIVD (controls). VAS, FIM, mJOA, Nurick’s grades were used for clinical assessment. CT scan focusing at CVJ (occipital condyles to inferior body of C2), 1 mm sections with zero spacing with axial, coronal and sagittal reconstructions was performed. The incidence and patterns of ligamentous calcifications of apical, alar, transverse atlantal ligaments and anterior atlanto-occipital membrane were observed.
Results: The mean age of patients with C3-4 PIVD (cases) was 55.5 years (range: 30 to 80 years) while that of C5-C6 PIVD (controls) was 43.5 years (range: 25 to 65 years) (p<0.001). Amongst the 70 cases, 68 patients (97.1%) had CVJ ligamentous calcifications while only 1 (3.3%) of the 30 control patients had CVJ ligamentous calcification. The apical ligament was the most frequent to be calcified accounting for 31 (44.3%) cases. Alar ligament, anterior atlanto-occipital membrane calcification were noted in 3(4.3%) patients and 9(12.9%) patients in high cervical disc disease. A combination of alar and apical ligament calcification was noted in 2 (2.9%) patients, combination of apical and TAL ligament calcification was noted in 1 (1.4%) patient. In controls, 1 (3.3%) patient had calcification of the anterior atlanto-occipital ligament. Calcification of CV Junction ligament was more in cases than in controls (p<0.001). C3-4 PIVD patients presented with a poorer pre-op (58.6% in cases vs. 8% in controls) and post-op nurick’s grade. 43 (61.4%) patients of high cervical disc disease had T2 hyperintense signal changes on pre-operative MRI compared to 7 (23.3%) patients in low cervical disc disease group (p<0.001).
Conclusion: CVJ ligamentous calcifications have strong association with HCDD.
Keywords
CV junction ligamentous calcification, High cervical disc prolapse, Nurick’s grades, Patients.
Introduction
Spondylotic changes in the cervical spine are the result of wear and tear secondarily to aging and abnormal stress. The common occurrence of these beginning in 4th decade at C5-C6/C6-C7 level are attributed to being the most mobile segment, with a general belief that the degeneration proceeds from below upwards from cervico-thoracic junction [1].
High cervical disc disease differs with its occurrence, a decade or two. An element of surprise stems from the fact that in many such patients, the lower levels i.e., C5-C6 are normal contrary to the general belief. The scarcely available literature with anecdotal case reports or retrospective reviews pointed it to CVJ as the causative factor. This study is our attempt to look into the probable relation between CVJ ligamentous involvements in the form of calcification to the occurrence of symptomatic HCDD [2].
Materials and Methods
This is a prospective study of 100 cases where 70 patients of high cervical disc disease were taken as cases and 30 patients of low cervical disc disease were taken as controls. Symptomatic degenerated sub-axial cervical spine disease cases attending neurosurgery OPD, NIMS from October 2016 to October 2018 were grouped into high or low cervical disc disease. All the patients were grouped into following categories: 1) High cervical disc disease (C2-C3, C3-C4) 2) Low cervical disc disease (C5-C6, C6-C7). Clinical status (using VAS, Nurick’s grade, FIM, mJOA), radiological parameters and follow-up status of the two groups were compared and analyzed. All patients underwent routine MRI of cervical spine. Patients with symptomatic cervical degeneration were subjected to CT cervical spine focusing at CVJ (occipital condyles to inferior body of C2), 1 mm sections with zero spacing with axial, coronal and sagittal reconstructions. The incidence and patterns of ligamentous calcifications at the CVJ were analyzed in either group. Statistical analysis was performed with SPSS software version 10.0 [3].
Results
Demography
Mean age of cases was 55.5 years (range: 30 to 80 years) and of controls was 43.5 years (range: 25 to 65 years) (p<0.001). Among 70 cases, 57 (81.4%) were male and 13 (18.6%) were female and amongst 30 controls, 22 (73.3%) were male and 8 (26.7%) were female [4].
Clinical features
Pre OP clinical symptoms and signs were recorded such as neck pain, tightness of limbs, parasthesias and weakness. The mean pre-operative neck pain VAS score of cases was 4.2 (range: 0-8) and of controls was 4.8 (range: 0-7). The mean FIM values were 90 (range: 44-116) among cases and 106 (range: 64-126) among controls. The mean mJOA score was 11 (range: 6-18) and 13 (range: 7-18) among cases and controls respectively. Clinical follow up of all cases and controls was done and ranged from 6 months to 2 years with an average follow up of 1 year. Post operative mean neck pain VAS score for cases was 3.8 (range: 0-7) and 3.2 (range: 0-6) respectively. Post OP FIM scores of cases and controls were 93.3 (range: 49-106) and 110.7 (range: 68-126). The mean post operative mJOA score were 12 (range: 8-18) and 15 (range: 9-18) in cases and controls respectively. Overall both in clinical symptoms and signs control group showed improvement compared to cases (p<0.01). Table 1 gives a tabular data of age, pre op and post op VAS, FIM, mJOA along with p values between cases and controls [5].
| Variables | Group | N | Mean | Std. deviation | P value |
|---|---|---|---|---|---|
| Age | Cases | 70 | 55.514 | 10.8944 | 0.001 |
| Controls | 30 | 43.533 | 8.5892 | ||
| VAS pre op | Cases | 70 | 4.286 | 1.9422 | 0.157 |
| Controls | 30 | 4.867 | 1.6761 | ||
| FIM pre op | Cases | 70 | 90.371 | 17.7602 | 0.001 |
| Controls | 30 | 106.233 | 17.7486 | ||
| MJOA pre op | Cases | 70 | 11.343 | 2.2321 | 0.001 |
| Controls | 30 | 13.833 | 2.5337 | ||
| Post op VAS | Cases | 70 | 3.086 | 1.558 | 0.143 |
| Controls | 30 | 3.567 | 1.3309 | ||
| Post op FIM | Cases | 70 | 93.371 | 17.1026 | 0.001 |
| Controls | 30 | 110.7 | 15.7462 | ||
| Post op MJOA | Cases | 70 | 12.786 | 2.1928 | 0.001 |
| Controls | 30 | 15.933 | 2.3034 |
Table 1. Comparison of various scoring systems between pre operative and post operative in cases and controls.
Nuricks grading
Most of the patients in cases group i.e., high cervical disc disease had myelopathy features with most of them presenting with poor nuricks grade compared to controls in which nuricks grade was good. Among 70 cases, 60 patients (85.7%) presented with myelopathy and among 30 controls, 12 patients (40%) presented with myelopathy (p<0.001). Among 70 cases, 10 patients (12.9%) presented with radiculopathy and among 30 controls, 18 patients (60%) presented with radiculopathy. 71% of patients in cases (C3/C4 PIVD) had poor Nuricks grading (3-5) where as 29% of patients in cases (C3/C4 PIVD) had good Nuricks grading (0-2) whereas in controls 27% of patients have poor nurick’s grading (3-5) and 73% of patients have good Nuricks grading (0-2). Patients in C3/C4 PIVD group continued to remain in poorer Nuricks grade even after surgery compared to C5/C6 PIVD (p<0.001). Tables 2 and 3 gives comparative list of nuricks grading for cases and controls between pre and post op values [6].
| Group | Total | ||||
|---|---|---|---|---|---|
| Case | Control | ||||
| Pre op Nuricks grading | Grade 0 | Count | 0 | 11 | 11 |
| % within group | 0 | 36.7% | 11% | ||
| Grade 1 | Count | 3 | 5 | 8 | |
| % within group | 4.3% | 16.7% | 8% | ||
| Grade 2 | Count | 26 | 6 | 32 | |
| % within group | 37.1% | 20% | 32% | ||
| Grade 3 | Count | 29 | 7 | 36 | |
| % within group | 41.4% | 23.3% | 36% | ||
| Grade 4 | Count | 10 | 0 | 10 | |
| % within group | 14.3% | 0 | 10% | ||
| Grade 5 | Count | 2 | 1 | 3 | |
| % within group | 2.9% | 3.3% | 3% | ||
| Total | Count | 70 | 30 | 100 | |
| % within group | 100% | 100% | 100% | ||
Table 2. Pre op nuricks grading in cases and controls.
| Group | Total | ||||
|---|---|---|---|---|---|
| Case | Control | ||||
| Post op Nuricks | Grade 0 | Count | 7 | 15 | 22 |
| % within group | 10% | 50% | 22% | ||
| Grade 1 | Count | 21 | 7 | 28 | |
| % within group | 30% | 23.3% | 28% | ||
| Grade 2 | Count | 28 | 6 | 34 | |
| % within group | 40% | 20% | 34% | ||
| Grade 3 | Count | 13 | 2 | 15 | |
| % within group | 18.6% | 6.7% | 15% | ||
| Grade 4 | Count | 1 | 0 | 1 | |
| % within group | 1.4% | 0 | 1% | ||
| Total | Count | 70 | 30 | 100 | |
| % within group | 100% | 100% | 100% | ||
Table 3. Post op Nuricks grading comparison in cases and controls.
Radiological features
In our study among 70 cases, 68 patients (97.1%) had craniovertebral ligamentous calcification and among 30 controls, 1 patient (3.3%) had cranio-vertebral ligamentous calcification. There were individual ligamentous calcifications as well as multiple ligamentous calcifications. Alar, apical, TAL, anterior atlanto-occipital membrane were the principal ligaments involved [7]. Among cases, apical ligament was the most frequent ligament noted to be calcified accounting for 31 (44.3%) cases. In controls, 1 (3.3%) patient had calcification of the anterior atlanto-occipital ligament. Calcification of CV junction ligament was more in cases than in controls (p<0.001). Individual ligaments calcification such as alar ligament, apical ligament, anterior atlanto-occipital membrane calcification were found in 3 (4.3%) patients, 31 (44.3%), 9 (12.9%) patients in high cervical disc disease. In few cases both ligaments were found to be calcified. For example combination of alar and apical ligament calcification was noted in 2 (2.9%) patients, combination of apical and TAL ligament calcification was noted in 1 (1.4%) patients, calcification of both alar ligaments were noted in 3 (4.3%) patients, combination of left alar and apical ligament calcification was noted in 2 (2.9%) patients. Calcification of left alar and left side of TAL was noted in 2 (2.9%) of patients. Table 4 shows number and percentage of various CV junction ligamentous calcifications [8].
| Group | Total | ||||
|---|---|---|---|---|---|
| Case | Control | ||||
| Individual ligament calcification | Alar ligament | Count | 3 | 0 | 3 |
| % within group | 4.3% | 0 | 3% | ||
| Ant atlanto-occipital membrane | Count | 9 | 0 | 9 | |
| % within group | 12.9% | 0 | 9% | ||
| Anterior atlanto-occipital ligament | Count | 0 | 1 | 1 | |
| % within group | 0 | 3.3% | 1% | ||
| Apical ligament | Count | 31 | 0 | 31 | |
| % within group | 44.3% | 0 | 31% | ||
| Apical ligament and alar ligaments | Count | 2 | 0 | 2 | |
| % within group | 2.9% | 0 | 2% | ||
| Apical ligament and TAL calcification | Count | 1 | 0 | 1 | |
| % within group | 1.4% | 0 | 1% | ||
| Bilateral alar ligament calcification | Count | 3 | 0 | 3 | |
| % within group | 4.3% | 0 | 3% | ||
| Left alar and apical | Count | 2 | 0 | 2 | |
| % within group | 2.9% | 0 | 2% | ||
| Left alar and left side of TAL | Count | 2 | 0 | 2 | |
| % within group | 2.9% | 0 | 2% | ||
| Left alar ligament calcification | Count | 3 | 0 | 3 | |
| % within group | 4.3% | 0 | 3% | ||
| No | Count | 2 | 29 | 31 | |
| % within group | 2.8% | 96.7% | 31% | ||
| Right alar and atlanto-occipital membrane | Count | 1 | 0 | 1 | |
| % within group | 1.4% | 0 | 1% | ||
| Right alar and right side of TAL | Count | 4 | 0 | 4 | |
| % within group | 5.7% | 0 | 4% | ||
| TAL and Apical ligament calcification | Count | 3 | 0 | 3 | |
| % within group | 4.3% | 0 | 3% | ||
| TAL and atlanto-occipital membrane | Count | 2 | 0 | 2 | |
| % within group | 2.9% | 0 | 2% | ||
| TAL and bilateral alar | Count | 1 | 0 | 1 | |
| % within group | 1.4% | 0 | 1% | ||
| Tal, alar and apical ligament | Count | 1 | 0 | 1 | |
| % within group | 1.4% | 0 | 1% | ||
| Total | Count | 70 | 30 | 100 | |
| % within group | 100% | 100% | 100% | ||
Table 4. Number and percentage of various CV ligaments calcification.
T2 hyperintense signal changes
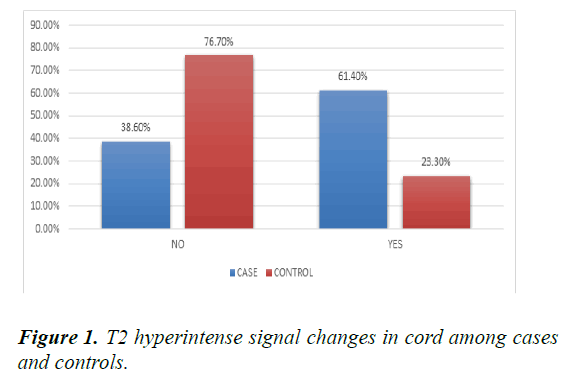
Most of the patients in cases (C3/C4 PIVD) group had T2 hyperintense signal changes compared to controls (p<0.001). 43 (61.4%) patients of high cervical disc disease had T2 hyperintense signal changes on pre-operative MRI compared to 7 (23.3%) patients in low cervical disc disease group. Figure 1 shows percentage of cases having T2 hyperintense signal changes in cord among cases and controls [9].
Case illustration
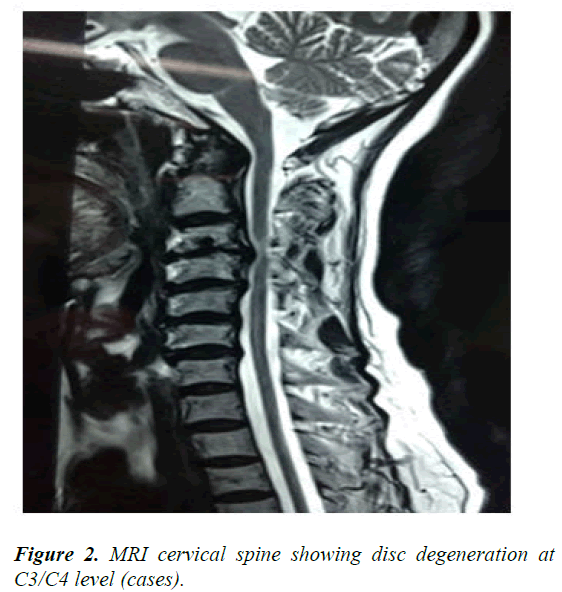
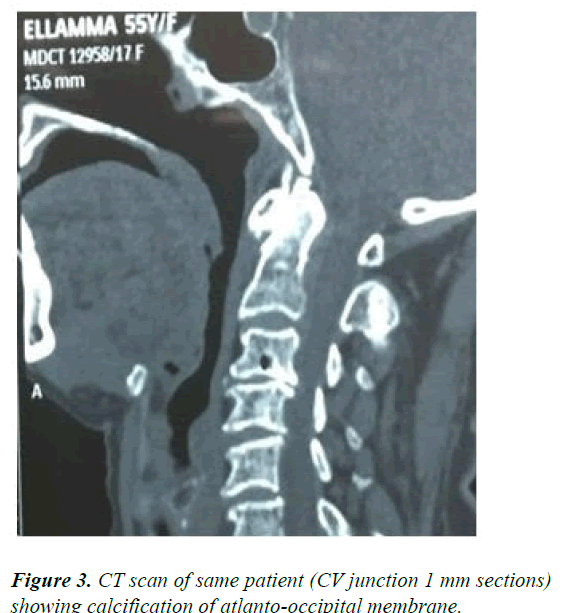
This is a 60 year old male who presented with myelopathy features and sensory loss below C4 level. MRI showed evidence of C3/C4 PIVD. CT scan CV junction zoomed images were taken to see for calcification (Figures 2 and 3) [10].
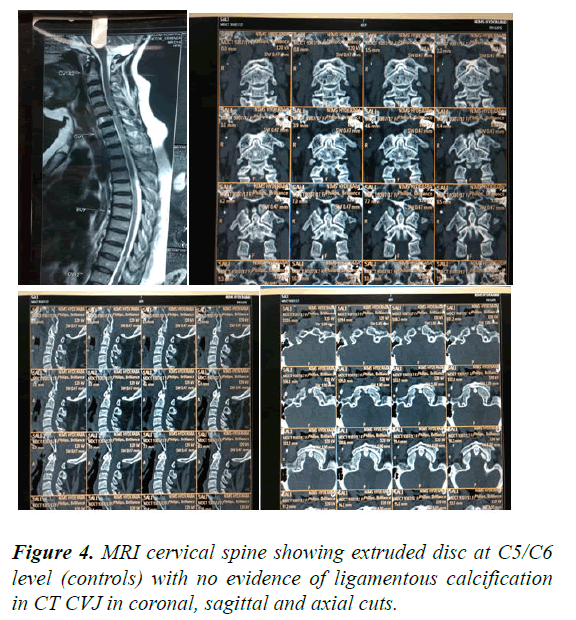
Here is an example to show no ligamentous calcification noted at CV junction in low cervical disc disease. This is a 50 year old female who presented with C6 radiculopathy features. MRI showed evidence of C5/C6 PIVD. CT scan CV junction 1 mm sections shows no evidence of calcification in axial, coronal and sagittal cuts (Figure 4).
Discussion
The mean age of presentation of HCDD in Mohanty et al., was 48 years (range 26-65 years) which was significantly higher as compared to controls with C5-6 PIVD (mean: 38 years, range 21-55 years, (p<0.001). Similar mean age groups were noted in our study with mean age of cases being 55.5 years (range: 30 to 80 years) which was significantly higher compared to mean age of controls (mean: 43.5; range: 25 to 65 years) (P<0.001) [11]. According to previous authors in the past, high cervical disc disease results due to degenerative changes developing at low cervical level in young age and as age progresses weight bearing shifts to high cervical level resulting in high cervical disc disease. Other authors like Mohanty et al., documented presence of CVJ pathology as a predisposing factor for high cervical disc disease. In our study, we tried to find an association between high cervical disc disease and ligamentous calcification at CV junction. 68 (97.1%) patients of 70 cases of HCDD had calcification of CV Junction ligaments whereas only 1 (3.3%) patient out of 30 controls had CV Junction ligamentous calcification. The reason hypothesized for this according to us was that high cervical disc protrusion could be a result of excessive strain on high cervical level due to the abnormally fixed cranio-vertebral junction due to ligamentous calcification [12].
CV junction ligamentous calcification had resulted in restricted mobility of adjacent segment and thereby leading to high cervical disc protrusion. Exact cause of high cervical disc compression and the results of manipulating CV junction are difficult to evaluate in this study but there seems to be strong association between CVJ ligamentous calcification and HCDD. In study by Mohanthy et al., C3-4 PIVD presented in a poorer Nurick’s grade compared to C5-6 PIVD group (p=0.001). Patients in C3-4 PIVD group continued to remain in a poorer Nurick’s grade even after surgery compared to C5-6 PIVD (p=0.001). Similar results were noted in our study with most of the patients in cases group i.e., high cervical disc disease had myelopathy features with most of them presenting with poor Nuricks grade compared to controls. 71% of patients in cases (C3/C4 PIVD) had poor Nuricks grading (3-5) whereas 29% of patients in cases (C3/C4 PIVD) had good Nuricks grading (0-2) whereas in controls 27% of patients had poor Nurick’s grading (3-5) and 73% of patients had good Nuricks grading (0-2). Patients in C3-4 PIVD group continued to remain in a poorer Nurick’s grade even after surgery compared to C5-6 PIVD (p<0.01). Post operatively overall both in clinical symptoms and signs control group improved significantly compared to cases (p<0.001). Most of the patients in cases (C3/C4 PIVD) group had T2 hyperintense signal changes compared to controls. 43 (61.4%) patients of high cervical disc disease had T2 hyperintense signal changes on pre-operative MRI compared to 7 (23.3%) patients in low cervical disc disease group (p<0.01) [13].
Conclusion
High cervical disc disease is a geriatric disease. CVJ ligamentous calcification has strong association with HCDD. Apical ligament calcification is the most common ligament to be calcified. High cervical disc disease patients present with poorer nurick’s grade and have lesser degree of improvement after surgery. Presence of ligamentous calcification at craniovertebral junction leads to restricted mobility and faster degeneration at adjacent segment level leading to high cervical disc disease. Further studies are needed to look into exact cause of high cervical disc disease and its relation to changes at cranio-vertebral junction and its exact pathogenesis.
Declaration of Interest
No conflicts of interest.
References
- Bohlman HH, Emery SE. The pathophysiology of cervical spondylosis and myelopathy. Spine. 1988;13(7):843-6.
[Crossref] [Google Scholar] [PubMed]
- Connell MD, Wiesel SW. Natural history and pathogenesis of cervical disk disease. Orthoped Clin North Am. 1992;23(3):369-80.
[Crossref] [Google Scholar] [PubMed]
- Houser OW, Onofrio BM, Miller GM, et al. Cervical disk prolapse. Clin Proc. 1995;70(10):939-45.
[Crossref] [Google Scholar] [PubMed]
- Nishizawa S, Yokoyama T, Yokota N, et al. High cervical disc lesions in elderly patients-presentation and surgical approach. Acta Neuro. 1999;141(2):119-26.
[Crossref] [Google Scholar] [PubMed]
- Hayashi HA, Okada KO, Hashimoto J, et al. Cervical spondylotic myelopathy in the aged patient. A radiographic evaluation of the aging changes in the cervical spine and etiologic factors of myelopathy. Spine. 1988;13(6):618-25.
[Google Scholar] [PubMed]
- Goel A, Phalke U, Cacciola F, et al. Surgical management of high cervical disc prolapse associated with basilar invagination-two case reports. Neurol Med Chir. 2004;44(3):142-5.
[Crossref] [Google Scholar] [PubMed]
- Tomii M, Mizuno J, Itoh Y, et al. Clinical study of C3-C4 level surgical cases of cervical spondylosis. Clin Neurol Neurosurg. 2015;135:11-4.
[Crossref] [Google Scholar] [PubMed]
- Mohanty CB, Shukla DP, Indira Devi B, et al. Craniovertebral junction pathology in high cervical disc disease. British J Neurosurg. 2012;26(6):845-50.
[Crossref] [Google Scholar] [PubMed]
- Takahashi MU, Yamashita YA, Sakamoto Y, et al. Chronic cervical cord compression: Clinical significance of increased signal intensity on MR images. Radiology. 1989;173(1):219-24.
[Crossref] [Google Scholar] [PubMed]
- Chikuda H, Seichi A, Takeshita K, et al. Radiographic analysis of the cervical spine in patients with retro-odontoid pseudotumors. Spine. 2009;34(3):E110-4.
[Crossref] [Google Scholar] [PubMed]
- Goel A, Darji H, Shah A, et al. Retro-odontoid and retro-C2 body pseudotumor, pannus and/or cyst. A study based on analysis of 63 cases. World Neurosurg. 2021;151:e170-7.
[Crossref] [Google Scholar] [PubMed]
- Goel A, Vutha R, Shah A, et al. Spinal kyphoscoliosis associated with chiari formation and syringomyelia recovery following atlantoaxial fixation: A preliminary report and early results based on experience with 11 surgically treated cases. World Neurosurg. 2019;125:e937-46.
[Crossref] [Google Scholar] [PubMed]
- Joshi S, Balthillaya G, Neelapala YR. Thoracic posture and mobility in mechanical neck pain population: A review of the literature. Asian Spine J. 2019;13(5):849.
[Crossref] [Google Scholar] [PubMed]