Review Article - Journal of Clinical and Experimental Toxicology (2018) Volume 2, Issue 1
Cardiovascular health risk posed by Polycyclic Aromatic Hydrocarbon and Ultrafine Particles.
Collins Otieno Asweto*
School of Public Health, Maseno University, Kenya
- *Corresponding Author:
- Collins Otieno Asweto
School of Public Health, Maseno University, Kenya
Tel: +254731632798
E-mail: asweto_collins@yahoo.com
Accepted date: January 04, 2018
Abstract
There is increased cardiovascular disease incidence attributed to ambient air pollution. It is estimated that ischaemic heart disease and stroke account for 80% of ambient air pollution-related early deaths. The most deleterious are the ultrafine particles (UFPs) which have more prominent potential health threat, since they can act as carriers of other strong air pollutant such as polycyclic aromatic hydrocarbons (PAHs). UFPs are small in size, hence can easily penetrate and reach cardiovascular tissues and organs. To understand their mechanisms, studies on UFPs and PAHs induced cardiovascular diseases were reviewed. The studies showed that UFPs and PAHs initiate events in atherogenesis including oxidative stress, expression of cell adhesion molecules on the surface of the endothelium, inflammation, and endothelial dysfunction. Endothelial dysfunction is associated with cardiovascular diseases such as hypertension, coronary artery disease, chronic heart failure, and peripheral vascular disease. The current review provides useful information on deleterious effect of UFP and PAH exposure on cardiovascular system. Thus advancing knowledge on UFP and PAH toxicity underscores the importance of the cardiovascular effects of air pollutants.
Keywords
Ultrafine particles, cardiovascular, endothelial dysfunction.
Introduction
Escalating air pollution is contributing to increased cardiovascular health problems currently witnessed in the world. Cardiac diseases such as ischaemic heart disease and strokes account for 80% of ambient air pollution-related early deaths [1]. Additionally, it is estimated that about 3 million deaths and 85 million disability adjusted live years (DALYs) resulted from particulate matter of ambient air pollution in 2012 [1]. Ambient air pollution has been on the rapid increase in most part of the world due to industrialization, urbanization, and motorization [1].
Ambient air pollutants comprise of particulate matter (PM), gases, organic compounds, and toxic metals [2,3]. Particulate matter (PM) is a blend of liquid droplets (aerosols) and solid particles like dust, soot, smoke, and dirt. PM is found in smoke, diesel exhaust, and haze that either come specifically from combustion or is a result of response to gases and sunlight or air [4]. In any case, the inhalable particles are of 10 μm in aerodynamic diameter (PM10), fine particles 2.5 μm (PM2.5), and ultra-fine particles <0.1 μm (UFP). PM2.5, most generally utilized as a representative marker of exposure to air pollution, is progressively measured and checked by national air quality monitoring networks [5]. However, experimental evidence suggests that UFP may be more dangerous than PM10 and PM2.5 due to their chemical composition, small size, large surface area/ mass ratio, capability of generating reactive oxygen species (ROS), high retention rate, and deep penetration in the respiratory system [6]. Thus the World Health Organization (WHO) and the Organization for Economic Co-operation and Development (OECD) have called for a critical and comprehensive assessment of UFP safety [7]. Moreover, research substantiations demonstrate that exposure to UFPs adds to the advancement of cardiovascular disease; along these lines, triggering acute cardiac events such as altered heart rate, heart rate variability, changes in microvascular function, and systemic inflammation [8,9]. This is due to their unique physicochemical properties which have unpredicted biological effects [10-12].
Polycyclic aromatic hydrocarbons (PAHs) result from incomplete combustion of organic materials and are ever present in the environment. Human exposure to PAHs can occur via ingestion of PAHs contaminated soil, food, and water, inhalation of PAHs contaminated soil dust and air [13], and dermal contact with PAHs contaminated soil [14,15]. After PAHs entering human body via various exposure pathways, complex metabolism and unknown factors would also make PAHs reach cardiovascular tissues and organs. PAH has been previously link to development of cardiovascular disease (CVD) such as coronary heart disease, peripheral arterial disease, stroke, and myocardial infarction [16-20].
Due to widespread sources and persistent UFPs and PAHs in the environment. Human beings are exposed to UFP and PAH mixtures in particulate phases in ambient air. Long-term exposure to high concentrations of the mixture is associated with adverse health problems. Thus, studies on PAHs in particulate matter (PM), such as UFP in ambient air, have become attention greater focus of research in recent years.
Ultra-fine Particles and Polycyclic Aromatic Hydrocarbons
Ultra-fine Particles (UFPs) have been found to have an atmospheric concentration ten times higher in the urban air than in rural air and are considered the most detrimental of all PM fractions [21]. This is on the account of UFP size empowers them to infiltrate through the lung to the circulatory system and reach other organs [22]. In addition, UFPs act as carriers of other strong air pollutant such as Polycyclic Aromatic Hydrocarbons (PAHs) [23] because of their adsorption capabilities. UFP are incidentally generated in the environment, often as by-products of fossil fuel combustion, condensation of semi-volatile substances or industrial emissions [24,25]. In addition, the speedy growth of nanotechnology is increasing the environmental exposure to nano-size particles. This exposure may be especially chronic for those employed in research laboratories and in high tech industry where workers handle, manufacture, use and dispose of nanoparticles.
On the other hand, PAHs are ubiquitous environmental pollutants generated primarily during the incomplete combustion of organic materials such as coal, oil, petrol, and wood. Exposure to PAH has been previously link to development of cardiovascular disease (CVD) such as coronary heart disease, peripheral arterial disease, stroke, and myocardial infarction [16-20]. Besides, elevated PAH metabolites in urine has been associated with increased CVD events [18]. Moreover, a previous study reported an increased risk for fatal ischemic heart disease in relation to occupational exposure to benzo(a)pyrene [16]. The major route of PAH exposure include in halation, ingestion, and dermal contact in both occupational and non-occupational setting [26]. Many PAHs are toxic and rapidly distributed in a wide variety of tissues with a marked tendency to localize in body fat [26].
Polycyclic aromatic hydrocarbons (PAHs) are organic compound pollutants, which are ubiquitous in ambient air and exist as gases or joined to the Particulate Matter (PM) [27]. The existing interaction between UFPs and PAH from trafficrelated air pollutants [28] might be the reason for progression of atherosclerosis observed in low level pollution below the existing regulatory standards [29,30].
Mechanisms of Ultra-fine Particles and Polycyclic Aromatic Hydrocarbons Action
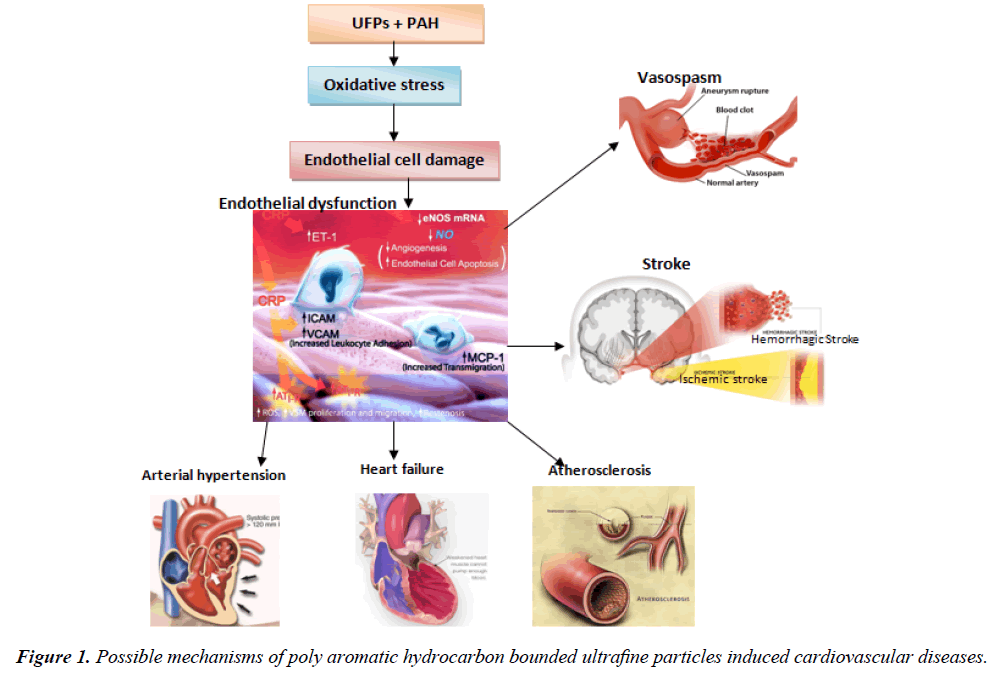
Upon entering the bloodstream, the UFPs bound with PAH get into direct contact with blood vessels and the heart endothelial cells lining. Endothelial cells are the biological barriers which mediate clearance of nanoparticles, maintain vascular function and homeostasis [31]. Moreover, in vivo and human studies have indicated damage to endothelial cells as an important mechanistic event by which inhalation of particles is associated with cardiovascular diseases [32]. The initial events in atherogenesis include the expression of cell adhesion molecules on the surface of the endothelium, inflammation, and endothelial dysfunction [33]. Both UFPs and PAH have also been shown to individually induce endothelial cell toxicity resulting in endothelial dysfunction [34-36]. Long term exposure to high levels of environmental UFPs have been shown to increase risk of arteriosclerosis, whereas short-term exposure can cause changes in heartrate variability [37]. UFP exposure depresses myocardial contractile response and coronary flow in both spontaneously hypertensive and wild-type rats [38,39].
Tithof et al. (2002) investigate the effects of polycyclic aromatic hydrocarbons contained in cigarette smoke on phospholipase A2 (PLA2) activity and apoptosis of human coronary artery endothelial cells. They found that B(a)P induce apoptosis of endothelial cells by a mechanism that involves activation of phospholipase A2 (PLA2) [40], leading to endothelium dysfunction. Endothelial dysfunction has been recognized as the source of multiple cardiovascular events that causes damage to the vascular wall, forms atherosclerotic plaque and consequently promotes vascular injury [41,42]. Besides, cardiovascular diseases such as hypertension, coronary artery disease, chronic heart failure, and peripheral vascular disease have been associated with endothelial dysfunction [43]. The underlying mechanisms are not understood, but oxidative stress and systemic inflammation have been suggested to play a role in PAH-induced CVD [44,45].
Ultra-fine Particles and Polycyclic Aromatic Hydrocarbons Joint Effects
Ultra-fine particles have been shown to have a greater content of redox active compounds, such as prooxidative polycyclic aromatic hydrocarbons (PAHs) that could provide them with a greater prooxidative potential [46]. In addition, their smaller size and greater surface-to-mass ratio may enable them to have greater bioavailability for the PAHs on their large surface area, making them more accessible to the contact sites of cells [46]. PAHs adsorb onto particles play a toxicological role in generating ROS, oxidative stress, and inflammation once inhaled [47]. Our previous study reported unanticipated toxicity induced by the co-exposure of UFPs and PAH, which was beyond the well-known toxicities of the individual compounds [48]. The SiNPs and B[a]P coexposure of induced excessive oxidative stress, subsequently resulting to DNA damage, cell cycle arrest, and apoptosis of endothelial cells [48]. Moreover, enhanced expression of proinflammatory and procoagulant genes have also been previously observed in SiNPs and B[a]P co-exposure [49], which is an indication of inflammation-coagulation cascade involvement in the co-exposure toxicity mechanism. Furthermore, oxidant injury plays an important role in UFPinduced adverse health effects including exacerbation and promotion of atherosclerosis [50].
In summary, the current review provides useful information on deleterious effect of UFP and PAH exposure on cardiovascular system. Thus advancing knowledge that underscores the importance of the cardiovascular effects of air pollutants. Further research is required to better understand the specific mechanisms by which PAH bounded UFP can lead to various cardiovascular effects. In addition, better parameters need to be developed to improve the assessment of PAH bounded UFP toxicity (Figure 1).
References
- World Health Organization. Ambient (outdoor) air quality and health: Fact sheet. WHO media, Geneva, Switzerland 2016.
- Craig L, Brook JR, Chiotti Q, et al. Air pollution and public health: a guidance document for risk managers. Journal of Toxicology and Environmental Health 2008; 71:588-698.
- Block ML, Calder´ GL. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends in Neurosciences 2009; 32:506-16.
- United Nations Environmental Programme (UNEP). Pollutants: Particulate matter (PM) 2016.
- World Health Organization. Ambient air pollution: Global assessment of exposure and burden of disease. WHO Press, Geneva, Switzerland 2016.
- Kumar S, Verma MK, Srivastava AK. Ultrafine particles in urban ambient air and their health perspectives. Rev Environ Health 2013; 28:117-28.
- Yoshida T, Yoshioka Y, Tochigi S, et al. Intranasal exposure to amorphous nanosilica particles could activate intrinsic coagulation cascade and platelets in mice. Particle and Fibre Toxicology 2013;10: 41.
- Li N, Georas S, Alexis N, et al. A Work Group Report on Ultrafine Particles (AAAAI) Why Ambient Ultrafine and Engineered Nanoparticles Should Receive Special Attention for Possible Adverse Health Outcomes in Humans. J Allergy Clin Immunol 2016;138:386-96.
- Franklin BA, Brook R, Arden PC. Air pollution and cardiovascular disease. Curr Probl Cardiol 2015;40:207-38.
- Beaudrie CH, Kandlikar M, Gregory R, et al. Nanomaterial risk screening: a structured approach to aid decision making under uncertainty Environ. Syst. Decis 2014;pp:1-22.
- Boholm M, Arvidsson R. Controversy over antibacterial silver: implications for environmental and sustainability assessments. J. Clean. Prod. 2014;68:135-43.
- Grieger K, Redmon J, Money E, et al. A relative ranking approach for nano-enabled applications to improve risk-based decision making: a case study of army materiel Environ. Syst. Decis. 2015;35:42-53.
- Li Z. Health risk characterization of maximum legal exposures for persistent organic pollutant (POP) pesticides in residential soil: An analysis. J. environ. Man. 2018;205:163-73.
- Li Z, Jennings A. Worldwide regulations of standard values of pesticides for human health risk control: A review. Int. J. of Environ. Res. Public Health 2017;14: 826.
- Li Z, Jennings, A. Implied maximum dose analysis of standard values of 25 pesticides based on major human exposure pathways. AIMS Public Health 2017;4:383-98.
- Burstyn I, Kromhout H, Partanen T, et al. Polycyclic aromatic hydrocarbons and fatal ischemic heart disease. Epidemiology 2005;16:744-50.
- Xu X, Hu H, Kearney GD, et al. Studying the effects of polycyclic aromatic hydrocarbons on peripheral arterial disease in the United States. Sci. Total Environ. 2013;pp:341-462.
- Xu X, Cook RL, Ilacqua VA, et al. Studying associations between urinary metabolites of polycyclic aromatic hydrocarbons (PAHs) and cardiovascular diseases in the United States. Sci Total Environ. 2010;408:4943-8.
- Gustavsson P, Plato N, Hallqvist J, et al. A population-based case-referent study of myocardial infarction and occupational exposure to motor exhaust, other combustion products, organic solvents, lead, and dynamite. Stockholm Heart Epidemiology Program (SHEEP) Study Group. Epidemiology 2001;12:222-8.
- Friesen MC, Demers PA, Spinelli JJ, et al. Chronic and acute effects of coal tar pitch exposure and cardiopulmonary mortality among aluminum smelter workers. Am. J. Epidemiol.2010;172:790-9.
- Mazaheri M, Clifford S, Jayaratne R, et al. School children's personal exposure to ultrafine particles in the urban environment. Environ Sci Technol.2014;48:113-20.
- Genc S, Zadeoglulari Z, Fuss SH, et al. The Adverse Effects of Air Pollution on the Nervous System. J. Tox. 2012;pp:1-23.
- Yu JZ, Huang XH, Ho SS, et al. Nonpolar organic compounds in fine particles: quantification by thermal desorption-GC/MS and evidence for their significant oxidatioin in ambient aerosols in Hong Kong. Anal Bioanal Chem 2011;401:3125-39.
- Nel A, Xia T, Madler L, et al. Toxic potential of materials at the nano level. Science 2006;311:622-7.
- Kliucininkas L, Martuzevicius D, Krugly E, et al. Indoor and outdoor concentrations of fine particles, particle-bound PAHs and volatile organic compounds in Kaunas, Lithuania. J. Environ. Monitoring 2011;13:182-91.
- Abdel-Shafy HI, Mansour MSM. A review on polycyclic aromatic hydrocarbons: Source, environmental impact, effect on human health and remediation. Egyptian J. Petr. 2015;25:107-23.
- Morales MG, Holgado FR, Marín MP, et al. Ambient air levels and health risk assessment of benzo(a)pyrene in atmospheric particulate matter samples from low-polluted areas: application of an optimized microwave extraction and HPLC-FL methodology. Environ Sci Pollut Res 2015;22:5340-9.
- Lee S, Kwak J, Lee J. Properties of roadway particles from interaction between the tire and road pavement. International Journal of Automotive Technology 2015;6:551-9.
- Adar SD, Sheppard L, Vedal S, et al. Fine Particulate Air Pollution and the Progression of Carotid Intima-Medial Thickness: A Prospective Cohort Study from the Multi-Ethnic Study of Atherosclerosis and Air Pollution. PLoS Med 2013;10:e1001430.
- Kunzli N, Jerrett M, Mack WJ, et al. Ambient air pollution and atherosclerosis in Los Angeles, Environ. Health Perspect 2005;113:201-6.
- Albini A, Mussi V, Parodi A, et al. Interactions of single-wall carbon nanotubes with endothelial cells. Nanomedicine 2010;6:277-88.
- Miller MR, Borthwick SJ, Shaw CA, et al. Direct impairment of vascular function by diesel exhaust particulate through reduced bioavailability of endothelium-derived nitric oxide induced by superoxide free radicals. Environmental Health Perspectives 2009;117:611-6.
- Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nature Reviews Immunology 2006;6:508-19.
- van Grevenynghe J, Monteiro P, Gilot D, et al. Human endothelial progenitors constitute targets for environmental atherogenic polycyclic aromatic hydrocarbons. Biochemical and Biophysical Research Communications 2006;341:763-9.
- Corbalan JJ, Medina C, Jacoby A, et al. Amorphous silica nanoparticles trigger nitric oxide/peroxynitrite imbalance in human endothelial cells: inflammatory and cytotoxic effects. Int J Nanomedicine 2011;6:2821-35.
- Guo C, Xia Y, Niu P, et al. Silica nanoparticles induce oxidative stress, inflammation, and endothelial dysfunction in vitro via activation of the MAPK/Nrf2 pathway and nuclear factor-κB signaling. International Journal of Nanomedicine 2015;10:1463-77.
- Peters A, Dockery DW, Muller JE, et al. Increased particulate air pollution and the triggering of myocardial infarction. Circulation 2001;103:2810-5.
- Hwang H, Kloner RA, Kleinman MT, et al. Direct and acute cardiotoxic effects of ultrafine air pollutants in spontaneously hypertensive rats andWistar- Kyoto rats. Journal of Cardio. Pharm. Therap. 2008;13:189-98.
- Simkhovich BZ, Marjoram P, Kleinman MT, et al. Direct and acute cardiotoxicity of ultrafine particles in young adult and old rat hearts. Basic Research in Cardiology 2006;102:467-75.
- Tithof PK, Elgayyar M, Cho Y, et al. Polycyclic aromatic hydrocarbons present in cigarette smoke cause endothelial cell apoptosis by a phospholipase A2-dependent mechanism. FASEB Journal 2002;16:1463-4.
- Chhabra N. Endothelial dysfunction – A predictor of atherosclerosis, Internet Journal of Medical Update 2009;4:33-41.
- Cimellaro A, Perticone M, Fiorentino TV, et al. Role of endoplasmic reticulum stress in endothelial dysfunction. Nutrition, Metabolism & Cardiovascular Diseases 2016;26:863-71.
- Rajendran P, Rengarajan T, Thangavel J, et al. The Vascular Endothelium and Human Diseases. International Journal of Biological Sciences 2013;9:1057-69.
- Jeng HA, Pan CH, Diawara N, et al. Polycyclic aromatic hydrocarbon-induced oxidative stress and lipid peroxidation in relation to immunological alteration. Occup. Environ. Med. 2011;68:653-8.
- Curfs DM, Knaapen AM, Pachen DM, et al. Polycyclic aromatic hydrocarbons induce an inflammatory atherosclerotic plaque phenotype irrespective of their DNA binding properties. FASEB J. 2005;19:1290-2.
- Araujo J. Particulate air pollution, systemic oxidative stress, inflammation, and atherosclerosis. Air Qual Atmos Health. 2011;4:79-93.
- Johnson P, Miller PJ. Ultrafine Particles: Issues Surrounding Diesel Retrofit Technologies for Particulate Matter Control. NESCAUM 2007.
- Asweto CO, Wu J, Hu H, et al. Combined Effect of Silica Nanoparticles and Benzo[a]pyrene on Cell Cycle Arrest Induction and Apoptosis in Human Umbilical Vein Endothelial Cells. Int. J. Environ. Res. Public Health 2017;14:1-15.
- Duan J, Yu Y, Li Y, et al. Inflammatory response and blood hypercoagulable state induced by low level co-exposure with silica. Chemosphere 2016;151:152-62.
- Araujo JA, Nel AE. Particulate matter and atherosclerosis: role of particle size, composition and oxidative stress. Part Fibre Toxicol. 2009;6:24.