Case Report - Journal of Neurology and Neurorehabilitation Research (2016) Volume 1, Issue 2
C2 Vertebral Corpectomy for Kyphosis Malunion of Remote Dens Fracture with Atlantoaxial Ankylosis and Myelopathy: Case Report at Twelve Years Follow-Up
Drew Bednar*Faculty of Health Sciences Hamilton, McMaster University, Ontario, Canada
- *Corresponding Author:
- Drew Bednar
Faculty of Health Sciences Hamilton
McMaster University
Ontario, Canada
Tel: 9055770639
Fax: 9055770178
E-mail: drewbednar@hotmail.com
Received date: September 06, 2016; Accepted date: October 05, 2016; Published date: October 06, 2016
DOI: 10.35841/neurology-neurorehabilitation.1.2.43-46
Visit for more related articles at Journal of Neurology and Neurorehabilitation ResearchAbstract
Late myelopathy from dens fracture non-union is rare and management in this case was greatly challenged by complete arthritic ankyloses C1/2. Purpose We report a case of ankylosed dens malunion in kyphosis developing progressive myelopathy decades after injury and requiring unique salvage surgery. Study design/Setting An academic spine care center. Patient sample-the patient was a 75-year-old female at presentation. Outcome measures Clinical myelopathy, X-ray alignment, CT scan. Methods-careful C2 corpectomy immediately distal to the odontoid process was successful in reversing myelopathy and preserving stability. This case is presented without funding support and the patient has given her permission for her case to be presented.
Case Report
A 75-year old woman had undergone posterior wire-instrumented instrumented atlantoaxial fusion for displaced odontoid base fracture at the age of 32 years. She presented with an 8 months history of progressive numbness in all four limbs with nondisabling loss of fine motor control and dexterity in the hands. There was occasional instability of gait on stairs but not yet requiring walking aids and without falls. There was stable mild chronic neck pain and no incident trauma.
Physical exam revealed a normally ambulatory senior with brisk hyperreflexia in all four limbs and positive Hoffman’s and Babinski’s signs, but no clonus.
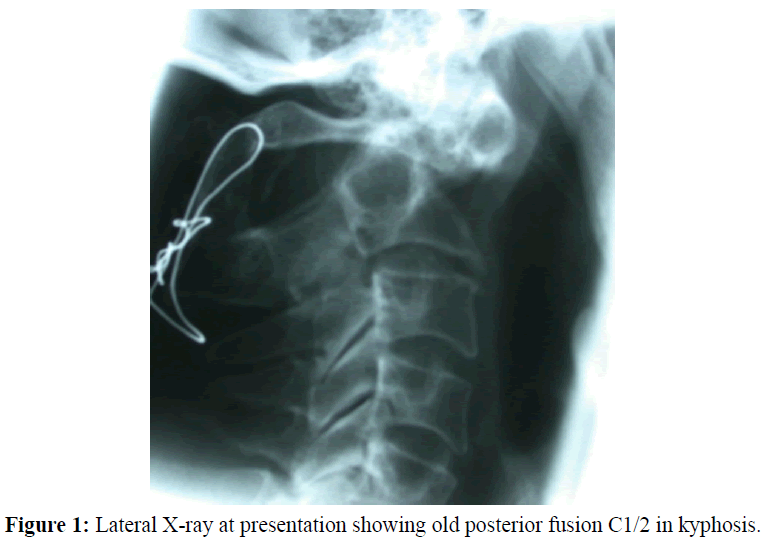
X-ray (Figure 1) suggested a stable and intact posterior wire/graft fusion from C1 to C2 in kyphosis. Flexion/extension views confirmed stability.
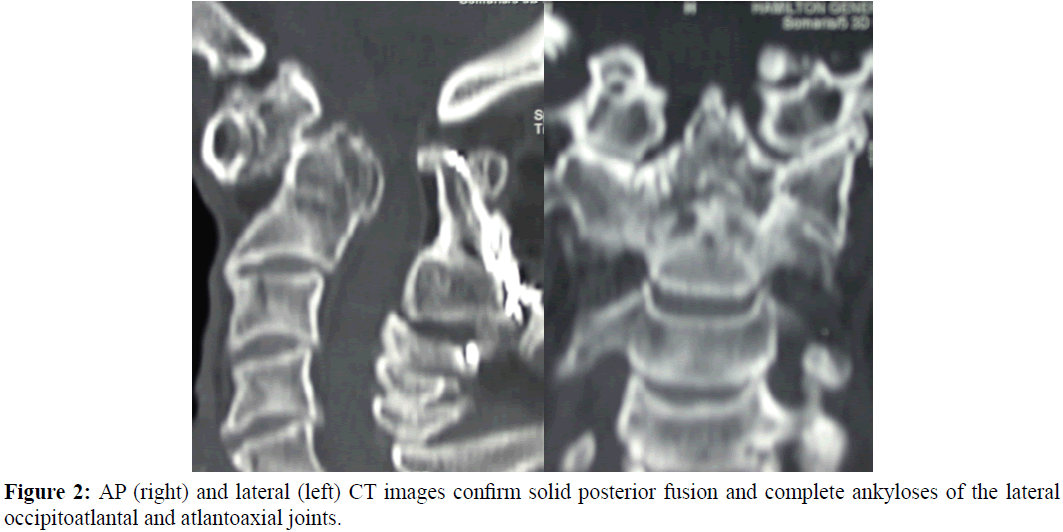
CT scan (Figures 2A and 2B) confirmed a continuous posterior fusion mass at C1/2 with established kyphotic malunion of previous dens base fracture. There were also complete ankyloses of the lateral atlantoaxial joints, the atlantodental joint and the antlanto-occipital joint with incomplete extraarticular ankylosis at C2/3.
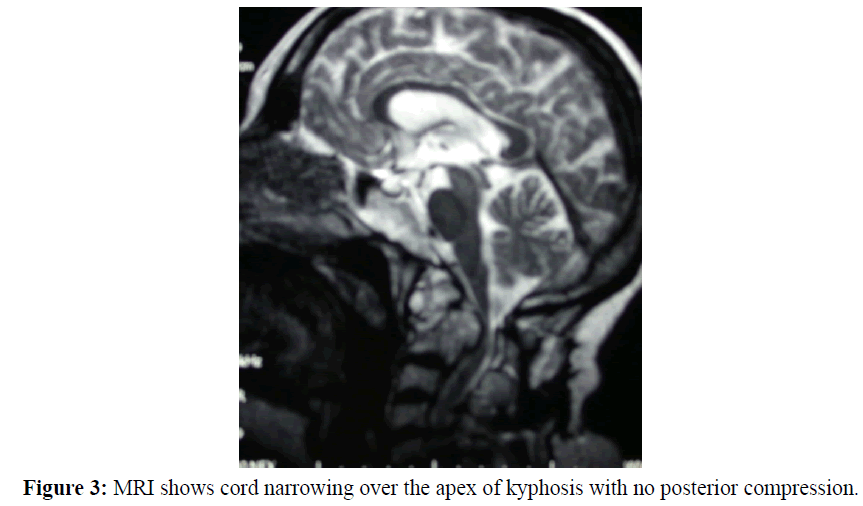
MRI (Figure 3) showed kyphotic tenting/thinning of the spinal cord at the postero-superior body of C2. There was neither posterior compression nor any anterior compression behind the dens itself.
Case Management
Transoral odontoidectomy was not an option because spinal cord compression was not caused by the odontoid but by the vertebral body of C2 below it. Also, maxillary excursion was limited by arthritic temporomandibular joints and judged insufficient for transoral exposure.
Realignment osteotomy at C1/2 was considered and declined for potential risk to the vertebral arteries.
Subtraction osteotomy (excision) of the prominent posterior aspect of the C2 vertebral body was performed via a high Smith-Peterson approach as recently described by Yang et al. The patient was positioned supine in light (5 pounds) Gardner-Wells traction with an inflatable pillow (Rudzki, 2004) placed immediately posterior to the neck to maximize cervical lordosis. Traction tape was applied under the mentum to give slight incremental extension proximally and lift the mandible away from the surgical field. Incision was at C4 to allow for the required obliquity of instrumentation access. Deep to platysma blunt dissection was used to approach C2 directly and so create a working channell into which a standard self-retaining cervical retractor (Trimline©; Medtronic Canada, Mississauga) could be placed for protection of the surrounding structures. The infrajacent C2/3 disc space and the malunited fracture site at the dens base defined respectively the caudal and cephalad limits of resection. The uncovertebral articulations C2/3 were preserved to protect the vertebral arteries and to provide anatomic continuity C2/3 in the anterior column.
At surgery in 2003 neither image guidance nor spinal cord monitoring was available at our hospital. The postero-inferior dens base was collinear to the postero-superior cortex of the C2 pars providing a radiographic guide to the site of compression and required decompression.
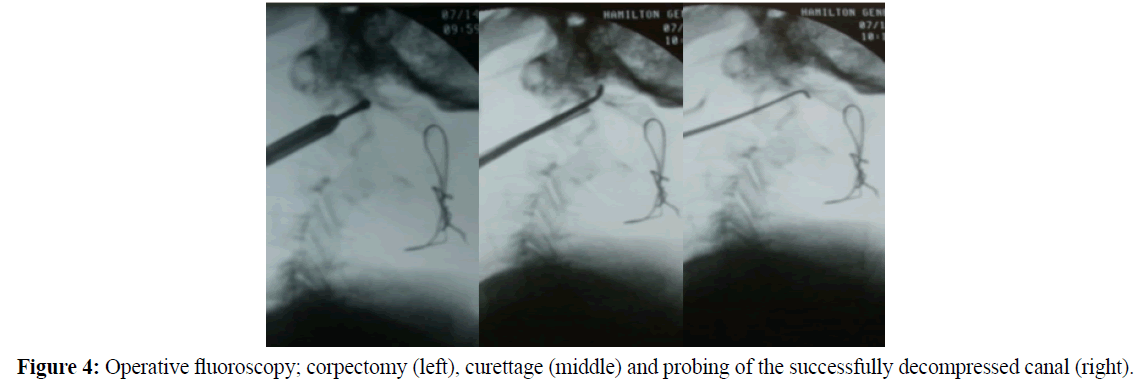
Resection was performed with a high-speed drill (Figure 4) until the posterior cortex was penetrated. Remaining middle column bone was then reflected forward into the osteotomy defect with fine curettes (Figure 5) and a dural hook (Figure 6) until the dura could be visualized across the full extent of the decompression site.
Postoperatively there was immediate and complete relief of myelopathy. The patient wore a hard cervical collar when ambulatory for a three-month period. At six months X-rays confirmed no change in cervical alignment and the asymptomatic patient was discharged from active care.
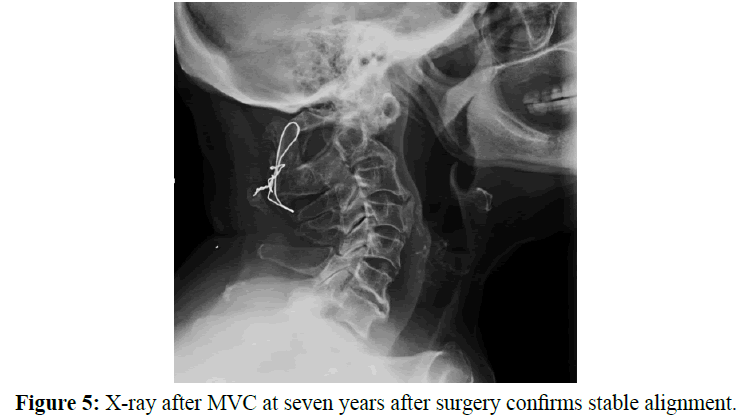
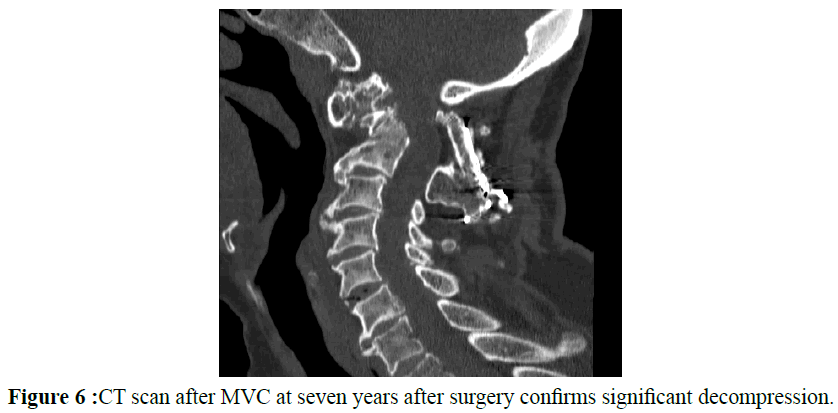
Seven years later she was involved in a low-energy motor vehicle accident and evaluated in the emergency room with X-rays and a CT scan confirming stable cervical alignment and adequate decompression at the osteotomy site. At fourteen years she remains free of myelopathy.
Discussion
In this case excessive fixed cervical kyphosis caused cord compression through acute angulation and decompression could be achieved either by realignment of kyphosis or anterior resection of the apex of the bony kyphosis at the vertebral body C2. Neurological symptoms were of recent onset and quickly progressive so observation was not an option. Interestingly (and in retrospect) both the O/C2 angle of Ota et al. at 15° and the occipitocervical angle of Riel et al. at 118° were within normal limits in this case.
It is unclear why our patient developed myelopathy several decades after her fracture repair though there are precedents (Fairholm, 1996., Alsunbul, 2014). No remote imaging or reports were available to define the immediate postoperative alignment after fracture repair but the position of the patients’ C1/2 interspinous wire (spanning C1 to C2 in good juxtaposition) suggests that the baseline fracture alignment had not changed significantly. Realignment osteotomy would have required resection through the vertebral artery foramena bilaterally and was not considered safely possible. It remains unprecedented.
Conclusion
Apex decompression for myelopathy from cervical kyphosis can be achieved and successful long-term in rare cases where realignment osteotomy may not be feasible. Careful resection of the C2 vertebral body’s posterior cortical prominence with preservation of the uncovertebral joints proved safe and long-term effective in this case.
References
- Alsunbul, W.A., Algird, A.R., Sanjer, M.F., Kesava, R. (2014) Inflatable Device for Intraoperative Control Cervical Extension in Cervical Surgery. Can J Neurol Sci, 41, 293-295.
- Fairholm, D., Lee, S.T., Lui, T.N. (1996) Fractured odontoid: the management of delayed neurological symptoms. Neurosurgery, 38, 38-43.
- Ota, M., Neo, M., Aoyama, T., Ishizaki, T., Fujibayashi, S., Takemoto, M., …. Nakamura, T. (2011) Impact of the O-C2 Angle on the Oropharyngeal Space in Normal Patients. Spine 36(11), E720-E726.
- Riel, R.U., Lenke, L.G., Riew, K.D. (2010) Measurement of a posterior occipitocervical fusion angle. J Spinal Disord Tech, 23, 1:27-29.
- Rudzki, J.R., Lenke, L.G., Blanke, K., Riew, K.D. (2004) Pseudoarthrosis of a thirty-nine-year-old dens fracture causing myelopathy: A case report. J Bone Joint Surg, 86-A, 2509-2513.
- Yang, J.S., Chu, L., Xiao, F.T., Zhang, D.J., Wang, Y., Chen, L., …. Deng, Z.L. (2015) Anterior retropharyngeal approach to C1 for percutaneous vertebroplasty under C-arm fluoroscopy. Spine J, 15, 539-545.