Research Article - Journal of Public Health and Nutrition (2018) Volume 1, Issue 4
Blood pressure pattern and body composition of hypertensive outpatients attending University college hospital, Ibadan.
Oluwasiji Olabisi O1*, Fadupin Grace T2, Adebiyi Adewole A31Department of Food Science and Technology, Wesley University, Ondo, Nigeria
2Department of Human Nutrition, University of Ibadan, Ibadan, Nigeria
3Cardiology Clinic, University College Hospital, Ibadan, Nigeria
- Corresponding Author:
- Dr. Olaitan Oluwasiji Olabisi
Department of Food Science and Technology
Wesley University
Ondo, Nigeria
Email: sijola2k3@gmail.com
Accepted Date: December 13, 2018
Citation: Olaitan OO, Adebiyi AA, Fadupin GT. Blood pressure pattern and body composition of hypertensive outpatients attending University college hospital, Ibadan. J Pub Health Catalog 2018;1(4):112-11
Abstract
Hypertension is one of the chronic non-communicable diseases which pose public health challenges in developing countries especially among black race, and excess weight gain has been found to be one of the predictors of hypertension. Conventional Body Mass Index (BMI) is limited in measuring the weight gain in individuals of all population groups and this gives the need for more reliable anthropometric index such as waist circumference, waist-to-hip ratio and waist-to-height ratio to measure body composition. This study evaluates the relationship between blood pressure pattern and body composition of the hypertensive outpatients who were attending University College Hospital, Ibadan, and Oyo State, Nigeria. The study design was descriptive cross-sectional involving ninety-two (92) hypertensive outpatients; 55 females and 37 males. A semi-structured, interviewer-administered questionnaire was used to interview the participants. The past three and the current participants’ Blood Pressure (BP) readings were assessed from their case files after the patients had consulted the physicians, and average BP was calculated for each patient. Weight (kg), body fat and visceral fat of the participants were measured by Automated Omron device. Height (m) measured with the use of stadiometer. Waist circumference (m) and Hip circumference (m) were measured with non-stretchable tape. Waist-to-height, waist-to-hip ratio and Body Mass Index were calculated. The hypertensive outpatients were 40.2% males and 59.8% females. Mean age of the male and female participants were 57.1 ± 13 years and 54.8 ± 13 years respectively. More than half (53.3%) of them had family history of hypertension (HTN) and some (41.4%) of them had been treating hypertension for five years while 49.5% had been on treatment for more than five years. Of all the patients, only 6.5% had normal BP, 44.6% had preHTN, 31.5% had stage 1 HTN and 17.4% had stage 2 HTN. Mean weight of the female and male patients were 73.45 ± 12.46 kg and 74.98 ± 12.52 kg respectively. Mean height of the female and male patients were 1.61 ± 0.06 m and 1.73 ± 0.09 m respectively. Waist circumferences of the female and male patients were 0.95 ± 0.16 m and 0.94 ± 0.10 m respectively. Waist-to-Hip Ratios (WHR) of the female and male patients were 0.96 ± 0.14 and 0.94 ± 0.10 respectively. Waist-to-Height Ratios (WHtR) of the female and male patients were 0.59 ± 0.09 and 0.54 ± 0.06 respectively. Body fat parentages of the female and male patients were 39.57 ± 7.51 and 22.53 ± 8.39 respectively. Visceral fat percentages of the female and male patient were 9.05 ± 3.05 and 9.65 ± 5.08 respectively. Resting Metabolism of the female and male patients were 1436.33 ± 143.65 and 1606.43 ± 187.97. Significant associations were observed between the age and diastolic blood pressure (p=0.001), between the weight-to-height ratio and systolic blood pressure (p=0.019) and diastolic blood pressure (p=0.032) of the patients; between body muscle of the patients and diastolic blood pressure (p=0.055). In conclusion, majority of the hypertensive outpatients had family history of hypertension. There was prevalence of prehypertension and stage 1 hypertension among the patients. Most of them were overweight, obese and had high abdominal adiposity which predicts risk of metabolic diseases such as diabetes and hyperlipidemia among the hypertensive patients. Significant relationship was found between waist-to-height ratio and systolic and diastolic blood pressures, and between age and diastolic blood pressure, and between body muscle and diastolic blood pressure.
Keywords
Blood pressure, Body composition, Hypertension, Outpatients.
Introduction
Hypertension is one of the chronic non-communicable diseases which pose public health challenges in developing countries especially among the black race where it is more prevalent with early onset and clinically more severe [1]. It is an established risk factor of cardiovascular disease, premature death and devastating condition related to the cerebrovascular, cardiovascular and renal complications [2,3].
As people increase in age, adults tend to be more physically inactive and store fats in their bodies, which slow down metabolism leading to the secretion of chemicals such as cortisol, leptin and other hormones which are more likely to cause obesity [4].
Excessive calorie intake, genetics, culture and lifestyle are other predictors of increased body fat. Excess weight gain has been found to be one of the predictors of hypertension and body fat distribution predicts hypertension independently of Body Mass Index [5,6].
Body composition is the relative amount of fat and fat free mass of the body. Conventional Body Mass Index (BMI) is limited in measuring the obesity and overweight in individuals of all population group because it does not distinguish between the lean muscle and fat mass and does not account for important contributors to weight such as bone density and blood volume [7]. Body Mass Index does not account for ethnic difference in body composition and distribution of excess fat [8].
Body composition of individuals is measured mostly by the anthropometry indicators which predict the adiposity, lean body mass and size [6]. This explains the reason for using other anthropometric parameters such as waist circumference, waist-to-hip ratio and waist-to-height ratio [9,10] in addition to BMI to determine the body adiposity.
The study aimed to determine pattern of blood pressure and its association to the body composition among the hypertensive outpatients who attended Cardiology unit at University College Hospital, Ibadan.
Materials and Methods
This study was descriptive cross-sectional in design, carried out among the ninety-two (92) hypertensive outpatients comprising of 55 females and 37 males who attended Cardiology Clinic of Medical Outpatients in University College Hospital, Ibadan, Oyo State, Nigeria. The University College Hospital, (UCH) Ibadan is the premier tertiary hospital and a reference health center for healthcare delivery in Nigeria.
A semi-structured, interviewer-administered questionnaire was used to interview the participants. The past three and the current participants’ Blood Pressure (BP) readings were assessed from their case files after the patients had consulted the physician, and average BP was calculated for each patient.
Weight (kg), body fat and visceral fat of the participants were measured by Automated Omron device. Height (m) measured with the use of stadiometer. Waist circumference (m) and Hip circumference (m) were measured with non-stretchable tape. Waist-to-height, waist-to-hip ratio and Body Mass Index were calculated.
Blood pressure of the participants was classified into normal BP, prehypertension, Stage 1 hypertension and Stage 2 hypertension according to the recommendation of the United States Joint National Committee on Prevention, Detection, Evaluation and Treatment of high blood pressure.
The classification of blood pressure control was based on the European Society of Hypertension and the European Society of Cardiology classification (ESH/ESC, 2013). The controlled blood pressure was placed with systolic blood pressure reading of less than 140 mmHg and diastolic blood pressure readings of less than 90 mmHg [11].
The ethical approval for the study was obtained from the Institutional Review Board, Institute of Advanced Medical Research and Training (IAMRAT), University College Hospital (UCH), the University of Ibadan, Ibadan.
Overweight and obesity were defined by multiple definitions depending on the diagnostic tool employed, viz: (1) BMI>25 but <30 (overweight) and BMI ≥ 30 (obese) (WHO, 1998), (2) WC>84 for women and >102 for men, WHR ≥ 0.90 for men and ≥ 0.85 [12], (3) WHtR ≥ 0.5 and (4) percentage body fat ≥ 32.0% (overweight) and ≥ 37.1% (obese) in black females and ≥ 21.7% (overweight) and ≥ 28.3%(5) (obese) in black males [13]. Visceral fat is considered as normal (1-9), high (10-14) or very high (15-30) [14].
Data collected were analyzed with the use of Statistical Package for Social Science (SPSS) software, version 20.0. Data were expressed as mean, standard deviation, frequency and percentage. Chi square test was used to determine association between variables and the gender while logistic regression was determined to test the association between the nutritional status, body composition, systolic blood pressure and diastolic blood pressure. Level of significance was p<0.05.
Results
The study comprised of 40.2% male and 59.8% female hypertensive outpatients who had mean age of 57 ± 13.26 years and 55 ± 13.39 years respectively. More than half (50.2%) of the participants were aged 55 years and above. Large numbers (85.9%) of them were married. Seventy-six percent of the participants were either traders or retirees. Statistical significance (p=0.017) was observed in the occupational status of the participants (Table 1).
| Characteristics | Male (n=37) n (%) |
Female (n=55) n (%) |
Total (n=92) n (%) |
X2 | P value |
|---|---|---|---|---|---|
| Age (years) | |||||
| Mean (SD) | 57.1 (13.26) | 54.8 (13.39) | 55.7 (13.32) | 1.433 | 0.698 |
| Range | 23-79 | 21-82 | 21-82 | ||
| 21-37 | 2 (25.0) | 6 (75.0) | 8 (8.7) | ||
| 38-54 | 12 (37.5) | 20 (62.5) | 32 (34.8) | ||
| 55-71 | 17 (42.5) | 23 (57.5) | 40 (43.5) | ||
| ≥ 72 | 6 (50.0) | 6 (50.0) | 12 (13.0) | ||
| Marital Status | |||||
| Single | 2 (5.4) | 2 (3.6) | 4 (4.3) | 3.724 | 0.293 |
| Married | 34 (91.9) | 45 (81.9) | 79 (85.9) | ||
| Divorce/Separated | 0 (0.0) | 2 (3.6) | 2 (2.2) | ||
| Widowed | 1 (2.7) | 6 (10.9) | 7 (7.6) | ||
| Occupational Status | |||||
| Artisan | 1 (2.7) | 3 (5.5) | 4 (4.3) | 10.248 | 0.017* |
| Trader | 7 (18.9) | 28 (50.9) | 35 (38.0) | ||
| Civil servant | 9 (24.3) | 9 (16.4) | 18 (19.6) | ||
| Retiree | 20 (54.1) | 15 (27.2) | 35 (38.1) | ||
| Note: *P<0.05, SD- Standard Deviation. | |||||
Table 1: Socio-demographic status of the Patients.
Information on the medical history of the patients is presented by Table 2. It was observed that more than half (53.3%) of the participants had family history of hypertension and some (41.4%) of them had been treating hypertension for five years while 49.5% of them had been treating it more than five years.
| Health information | Male (n=37) n (%) |
Female (n=55) n (%) |
Total (n=92) n (%) |
X2 | P value |
|---|---|---|---|---|---|
| Family History of hypertension | |||||
| Yes | 17 (34.7) | 32 (65.3) | 49 (53.3) | 1.33 | 0.249 |
| No | 20 (46.5) | 23 (53.5) | 43 (46.7) | ||
| Year of Diagnosis | |||||
| <1year | 5 (62.5) | 3 (37.5) | 8 (8.8) | 9.43 | 0.093 |
| 1-5years | 14 (36.8) | 24 (63.2) | 38 (41.4) | ||
| 6-10years | 7 (25.9) | 20 (74.1) | 27 (29.4) | ||
| 11-15years | 1 (25.0) | 3 (75.0) | 4 (4.4) | ||
| 16-20years | 4 (80.0) | 1 (20.0) | 5 (4.5) | ||
| >20years | 6 (60.0) | 4 (40.0) | 10 (11.2) | ||
| Presence of other ailment(s) with Hypertension |
|||||
| Yes | 19 (52.8) | 17 (47.2) | 36 (39.1) | 3.881 | 0.049* |
| No | 18 (33.1) | 38 (67.9) | 56 (60.9) | ||
| Patients’ Purpose of taking Medication | |||||
| For Hypertension only | 22 (33.3) | 44 (66.7) | 66 (71.7) | 5.377 | 0.068 |
| For Hypertension and other ailments | 14 (56.0) | 11 (44.0) | 25 (27.2) | ||
| Not taking medication | 1 (100.0) | 0 (0.0) | 1 (1.1) | ||
| Patients’ BP Control level | |||||
| ≤ 140/90 mmHg | 15 (31.9) | 32 (68.1) | 47 (51.1) | 2.755 | 0.097 |
| ≥ 140/90 mmHg | 22 (48.9) | 23 (51.1) | 45 (48.9) | ||
| Note: *p<0.05. | |||||
Table 2: Medical History of the Patients.
Table 2 presents the medical history of the participants. It was observed that large number (60.9%) of the patients had only hypertension while 39.1% of them had additional ailments to hypertension. Such ailments were; kidney diseases (13.0%), diabetes (7.6%), heart diseases (2.2%), Respiratory disease (2.2%), and other diseased conditions (such as arthritis, cancer, eye defect, goitre, ascities, oedema, pile, hepatitis, GIT problem) accounts for 14.1% (Table 3).
| Other health conditions with Hypertension | Frequency | Percentage |
|---|---|---|
| Kidney disease | 12 | 13 |
| Diabetes | 7 | 7.6 |
| Heart disease | 2 | 2.2 |
| Respiratory disease | 2 | 2.2 |
| Others (athritis, cancer, eye defect, goitre, ascities, oedema, pile, hepatitis, GIT problem) |
13 | 14.1 |
| Without other ailment(s) | 56 | 60.9 |
Table 3: Other Health conditions with Hypertension among Hypertensive Patients.
A statistical significance (p=0.049) was observed between the patients who had only hypertension and the patients who had hypertension with other diseases (Table 2). On medication, 71.7% of the patients took medications prescribed by the physicians for high blood pressure only while 27.2% of the patients took the medications for both hypertension and other diseases and very few (1.1%) did not take medication as at the time of the study.
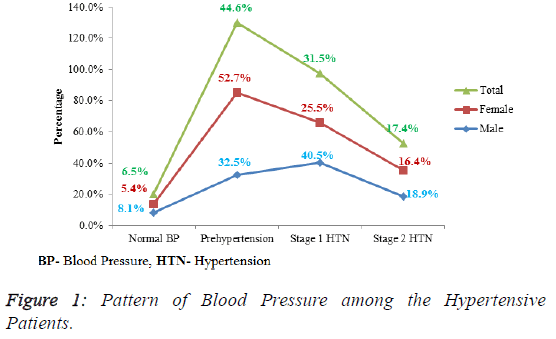
The blood pressure pattern of the patients is presented by Figure 1. Only 6.5% (male=8.1%, female5.4%) of the patients had normal blood pressure; 44.6% (male= 32.5%, female=52.7%) had prehypertension, 31.5% of the patients (male=18.9%, female=25.5%) had stage 1 hypertension and 17.4% (male=18.9%, female=16.4%) had stage 2 hypertension. Half (51.2%) of the patients had their blood pressure controlled while 48.9% of the patients had their blood pressure uncontrolled (Table 3).
Table 4 shows the Body Mass Index (BMI) of the participants. It was found that many (64.1%) of the patients were either overweight (36.8%) or obese (27.2%). Overweight (64.7%) and obesity (80.0%) were higher among the female patients than among the male counterparts. The Body Mass Index (BMI) of the patients was statistically significant across the gender (p=0.006).
| Body Mass Index (BMI) (Kg/m2) | Male (n=37) n (%) |
Female (n=55) n (%) |
Total (n=92) n (%) |
X2 | P value |
|---|---|---|---|---|---|
| 18.5-24.99 | 20 (60.6) | 13 (39.4) | 33 (35.9) | 10.299 | 0.006* |
| 25.0-29.99 | 12 (35.3) | 22 (64.7) | 34 (36.9) | ||
| ≥ 30.0 | 5 (20.0) | 20 (80.0) | 25 (27.2) | ||
| Note: *p<0.05. | |||||
Table 4: Body Mass Index of the Patients.
Table 5 presents the relationship between anthropometry index and the blood pressure of the hypertensive patients. The mean weights of the female and male patients were 73.45 ± 12.46 kg and 74.98 ± 12.52 kg respectively. The mean height of females was 1.61 ± 0.06 m and that of male patients was 1.73 ± 0.09 m. Waist circumferences of the female and male patients were 0.95 ± 0.16 m and 0.94 ± 0.10 m respectively.
| Index | Mean | St. Dev | Max | Min | Systolic BP P value |
Diastolic BP P value |
|---|---|---|---|---|---|---|
| Age | ||||||
| Female | 54.76 | 13.39 | 82 | 21 | 0.976 | 0.001* |
| Male | 57.11 | 13.26 | 79 | 23 | ||
| Weight (kg) | ||||||
| Female | 73.45 | 12.46 | 106.3 | 50.1 | 0.273 | 0.496 |
| Male | 74.98 | 12.52 | 101.1 | 50.7 | ||
| Height (m) | ||||||
| Female | 1.61 | 0.06 | 1.75 | 1.46 | 0.373 | 0.735 |
| Male | 1.73 | 0.09 | 1.92 | 1.53 | ||
| BMI (kg/m2) | ||||||
| Female | 28.17 | 4.39 | 35.8 | 20.1 | 0.244 | 0.765 |
| Male | 25.09 | 3.93 | 34.5 | 18.6 | ||
| WC (m) | ||||||
| Female | 0.95 | 0.16 | 1.37 | 0.42 | 0.173 | 0.22 |
| Male | 0.94 | 0.1 | 1.11 | 0.74 | ||
| WHR | ||||||
| Female | 0.96 | 0.14 | 1.37 | 0.42 | 0.239 | 0.599 |
| Male | 0.94 | 0.1 | 1.11 | 0.74 | ||
| WHtR | ||||||
| Female | 0.59 | 0.09 | 0.78 | 0.25 | 0.019* | 0.032* |
| Male | 0.54 | 0.06 | 0.65 | 0.44 | ||
| Body Fat (%) | ||||||
| Female | 39.57 | 7.51 | 50.7 | 19.7 | 0.596 | 0.165 |
| Male | 22.53 | 8.39 | 39.5 | 6.5 | ||
| Visceral fat (%) | ||||||
| Female | 9.05 | 3.05 | 18 | 2 | 0.303 | 0.094 |
| Male | 9.65 | 5.08 | 22 | 2 | ||
| Body Muscle | ||||||
| Female | 26.01 | 4.79 | 51.7 | 19.2 | 0.244 | 0.055* |
| Male | 33.94 | 5.18 | 46.1 | 22.5 | ||
| RM | ||||||
| Female | 1436.33 | 143.65 | 1835 | 1162 | 0.892 | 0.463 |
| Male | 1606.43 | 187.97 | 1974 | 1141 | ||
| SBP | ||||||
| Female | 139.24 | 15.37 | 115 | 177 | - | - |
| Male | 144.41 | 15.76 | 115 | 176 | ||
| Diastolic BP | ||||||
| Female | 84.42 | 9.901 | 65 | 117 | - | - |
| Male | 88.08 | 8.64 | 70 | 105 | ||
| Note: *p<0.05, WHR- Waist-to-hip ratio, WHtR- Waist-to-height ratio, WC-Waist Circumference, RM- Resting Metabolism, SBP- Systolic Blood Pressure, DBP-Diastolic Blood Pressure | ||||||
Table 5: Relationship between Anthropometric Index and Blood Pressure of the Hypertensive Patients.
Waist-to-Hip Ratios (WHR) of the female and male patients were 0.96 ± 0.14 m and 0.94 ± 0.10 m respectively. Waist-toheight ratios (WHtR) of the female and male patients were 0.59 ± 0.09 m and 0.54 ± 0.06 m respectively. Body fats (%) of the female and male patients were 39.57 ± 7.51 and 22.53 ± 8.39 respectively.
Visceral fat (%) of the female and male patients were 9.05 ± 3.05 and 9.65 ± 5.08 respectively. Resting Metabolisms of the female and male patients were 1436.33 ± 143.65 and 1606.43 ± 187.97. Significant associations were observed between the age and diastolic blood pressure (p=0.001), between the waist to- height ratio and systolic blood pressure (p=0.019); waist-toheight ratio and diastolic blood pressure (p=0.032) of the patients. Body muscle of the patients had significant association with the diastolic blood pressure (p=0.055).
Discussion
Treatment of the modifiable risk factors of hypertension such as dyslipidemia, abdominal obesity and diabetes is the primary goal of hypertensive patients in order to reduce the long-term risk of cardiovascular morbidity and mortality [15-17]. The age of most (78.3%) of the hypertensive patients in this study was within 38 to71 years, showing that both young adults and older adults are suffering from high blood pressure. This supports the results of the studies conducted by other researchers [13,17,18].
This study found significant association between Diastolic Blood Pressure (DBP) and age among the hypertensive outpatients. It supports the findings in which it was reported rise in diastolic blood pressure with increased age among the Pakistan adults in the comparative study conducted among three populations at Metrovill [19]. Tziomalos et al. observed that the relationship between DBP at admission and outcome appears to be more prominent in hypertensive patients and higher DBP at admission predict in-hospital mortality in patients with acute ischemic stroke. This shows the relative effects of increased diastolic blood pressure among the hypertensive patients [20].
Having more than half of the hypertensive patients in this study with family history of hypertension, reveals that hypertension is a hereditary disease which has been confirmed by many studies in Nigeria and abroad [20-22]. However, this is in contrast to the finding of Deji et al. [16] who reported that family history was not a risk factor of hypertension among the Yoruba adults in the similar study location, South-West, Nigeria where our study was conducted.
It was observed in this study that about half of the hypertensive patients in Nigeria had been visiting hospital for treatment more than five years. The number of these patients (49.5%) is greater than 25.8% reported by Deji et al. [16]. The increase can be due to poor adherence of the hypertensive patients to their medication or the patients engaging in lifestyles which prevent adequate blood pressure control among the hypertensive patients. It could also reveal the state of the health system in Nigeria. Although, the level of blood pressure control in this study shows that half of the patients had their blood pressure controlled (≤ 140/90 mmHg), but it was evident that majority of the hypertensive outpatients who participated were having prehypertension and stage 1 hypertension [23].
The prevalence of prehypertension (44.6%) observed in this study was closed to the level (45.5%) reported by Chimezie et al. in their cross-sectional study among adults in Umuahia, South-East Nigeria; less than 58.7% prevalence observed by Isezuo in Northern Nigeria and more than 37.2% reported by Mengistu in Ethiopia; 32.3% reported by Hu L [5] in China and 26.1% reported by Gyamfi et al. in Ghana [21]. Prehypertension has been reported to be the risk factor of hypertension, cardiovascular mortality and morbidity, a 3.5- fold increase in myocardial infarction, atherosclerosis, small vascular damage, coronary artery calcification, vascular remodeling, and left ventricular hypertrophy [24-27]. Prehypertension has been found to be strongly linked with the family history of hypertension, dietary pattern, lack of exercise, abdominal adiposity and markers of genetic predisposition to high blood pressure including parental hypertension or diabetes [12,28].
On the body composition of the hypertensive patients, many of the patients who participated in this study had increased waistto- height ratio, waist circumference, waist-to-hip ratio, Body Mass Index, body fat and visceral fat more than the normal recommendations for both male and female adults. This study observed that many of the patients were overweight and had abdominal adiposity. The association of abdominal adiposity with cardiovascular and metabolic diseases such as Type 2 diabetes and hypertension had been observed by many studies [29]. The excess weight and body fat observed among the hypertensive patients can be due to the sedentary lifestyle which many retirees and traders were known [15]. They tend to sit down for long period of time without expending the calorie consumed.
This study found significant association of systolic and diastolic blood pressures with waist-to-height ratio and body muscle. This is in agreement with the findings of Roberta et al. who reported linear correlation between waist-to-height ratio and blood pressure in their study which was conducted among the factory male workers in São Paulo State, Brazil. Alena also observed association between waist-height ratio and systolic blood pressure in his cross sectional study conducted among the migrants of Russian and Kurdish women in Finland [30]. Waist-to-height ratio has been found to be more sensitive to predict metabolic risk than BMI and to allow similar boundary value for different ethnic groups. It has been found to be the best anthropometric predictor of hypertension [31].
Conclusion
This study establishes that majority of the hypertensive outpatients had family history of hypertension. There is prevalence of prehypertension and stage 1 hypertension among the patients. Most of the patients were overweight, obese and had high abdominal adiposity which predicts risk of metabolic diseases such as diabetes and hyperlipidemia among the hypertensive patients. Significant relationship was found between waist-to-height ratio and systolic and diastolic blood pressures, and between age and diastolic blood pressure, and between body muscle and diastolic blood pressure.
Limitation of this Study
The cross-sectional design of this study affects its causal inference. This study was unable to assess the lifestyles (such as, dietary intake, smoking, alcohol consumption, physical activity and stress) of the hypertensive patients which could predict the cause of excess weight gain and abdominal adiposity which anthropometry measured. Further study is needed to measure the lifestyles and biochemical parameters (such as lipid profile and blood sugar) of the patients should be measured to determine the risk factors of hypertension and their relationship with prehypertension.
Recommendation
Hypertensive outpatients are advised to seek medical advice on how to lose weight, see the dietitian for appropriate diet regimen for their health condition, engage in appropriate physical exercise, avoid intake of saturated fat and psychological stress which could predispose them to adiposity.
References
- Behradmanesh S, Nasri P. Serum cholesterol and LDL-C in association with level of diastolic blood pressure in Type 2 diabetic patients. J Renal Inj Prev. 2012;1:23-6.
- Miura K. Strategies for prevention and management of hypertension throughout life. J Epidemiol. 2004;14:112-17.
- Tewodros W, Yewondwossen T, Patrick H, et al. Patterns of complications seen in patients with Hypertension admitted to Tikur Anbessa Hospital: A retrospective analysis. Ethiopi Med J. 2015;2:51-6.
- Abah JA. Relationship between blood pressure and body composition of active and inactive students of Ahmadu Bello University, Zaria, Nigeria. Master’s thesis submitted to Ahmadu Bello University, Zaria, Nigeria. 2011:1-84.
- Hu L, Huang X, You C, et al. Prevalence and risk factors of prehypertension and hypertension in Southern China. PLoS ONE. 2017;12:e0170238.
- World Health Organisation. Obesity: Preventing and managing the global epidemic. World Health Organization, Geneva.1998.
- Bogin B, Varela-Silva MI. The body mass index: The good, the bad and the horrid. Bulletin de la Societe Suisse d’Anthropologie. 2012;18:5-11.
- World Health Organisation. Waist circumference and waist-hip ratio. Report of WHO expert consultation, Geneva. 2008.
- Ejike, Chukwunonso ECC, Chinwendu E, et al. Obesity determined by different measures and its Impact on the health-related quality of life of young-adult Nigerians. Asian J Clin Nutr. 2015;7:64-75.
- Caminha CST, Haroldo SF, Narithania SC, et al. Waist-to-height ratio is the best anthropometric predictor of hypertension, a population-based study with women from a state of northeast of Brazil. Medicine. 2017;96:102.
- World Health Organisation. Raised blood pressure, situation and trends. An article from Global Health Observatory (GHO) data, 2015.
- Zhu S, Z Wang, W Shen, et al. Percentage body fat ranges associated with metabolic syndrome risk: results based on the third National Health and Nutrition Examination Survey (1988-1994). Am J Clin Nutr. 2003;78:228-35.
- Roberta SLC, Fernando N, Antônio PF, et al. Relationship between blood pressure and Anthropometry in a cohort of Brazilian men: A cross-sectional study. Am J Hypertens. 2009;22:980-4.
- Isezuo SA, Sabir AA, Ohwovorilole AE, et al. Prevalence, associated factors and relationship between prehypertension and hypertension: a study of two ethnic African populations in Northern Nigeria. J Hum Hypertens. 2011;25:224-30.
- Chimezie GO, Stanley CN, Oluchi JC, et al. Towards prevention of hypertension in Nigeria: A study of prehypertension and its associations among apparently healthy adults in Umuahia, South-East Nigeria. Int J Prevent Med. 2015;6:61.
- Deji SA, Olayiwola IO, Fadupin GT. Assessment of nutritional status of a group of Hypertensive patients attending tertiary healthcare facilities in Nigeria. East Afr Med J. 2014;91:99-104.
- Olaitan OO, Fadupin GT, Adebiyi AA. Dietary pattern, lifestyle and nutritional status of hypertensive outpatients attending University College Hospital, Ibadan, Nigeria. Afr J Biomed Res. 2018;21:29- 36.
- Esayas KG, Yadani M, Sahilu A. Prevalence of hypertension and its risk factors in Southwest Ethiopia: a hospital-based cross-sectional survey. Integr Blood Press Control. 2013;6:111–117.
- Chandra A, Neeland IJ, Berry JD, et al. The relationship of body mass and fat distribution with incident hypertension. J Am Coll Cardiol. 2014;64:997– 1002
- Tziomalos K, Giampatzis V, Bouziana SD, et al. Elevated diastolic but not systolic blood pressure increases mortality risk in Hypertensive but not Normotensive patients with Acute Ischemic Stroke. Am J Hypertens. 2015;28:765-71.
- Gyamfi D, Obirikorang C, Emmanuel A, et al. Prevalence of pre-hypertension and hypertension and its related risk factors among undergraduate students in a Tertiary institution, Ghana. Alex J Med. 2018.
- Celik T, Yuksel UC, Fici F, et al. Vascular inflammation and aortic stiffness relate to early left ventricular diastolic dysfunction in Prehypertension. Blood Pressure. 2013;22:94-100.
- Huang Y, Wang S, Cai X, et al. Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Medicine. 2013;11:177.
- Mengistu MD. Pattern of blood pressure distribution and prevalence of hypertension and prehypertension among adults in Northern Ethipoia: disclosing the hidden burden. BMC Cardiovascular disorders. 2014;14:33.
- Sayali ER, Atish BP. Study of frequency of prehypertension and associated factors in medical students. Indian J Basic Applied Med Res. 2017;6:201-211.
- Hirani V, Zaninotto P, Primatesta P. Generalised and abdominal obesity and risk of diabetes, hypertension and hypertension-diabetes co-morbidity in England. Public Health Nutr. 2008;11:521-7.
- Alena A. (2017). The association between bmi, waist-to-height ratio and blood pressure in Russian, Somali and Kurdish Migrants residing in Finland. Master’s thesis. 2017:1-72.
- Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. 2005;56:303-307.
- Rockwood HRM, Howlett SE. Blood pressure in relation to age and frailty. Can Geriatr J. 2011;14:2-7.
- Rashed AB, Hussain A, Böhm M. Blood pressure control and predictors of uncontrolled hypertension. Bahrain Medical Bulletin. 2014;36.
- World Health Organisation. Raised blood pressure, situation and trends. An article from Global Health Observatory (GHO) data. 2015.