Research Article - Biomedical Research (2017) Volume 28, Issue 4
Birth defects of children in women received in vitro fertilization-embryo transfer (IVF-ET): A meta-analysis
Jian Wang1*, Yaqun Yin2, Shanfang Jiang1
1Reproductive Medicine Centre, Dong Guan Tungwah Hospital, Dongguan, Guangdong, PR China
2Department of Obstetrics, Dong Guan Tungwah Hospital, Dongguan, Guangdong, PR China
Accepted on September 27, 2016
Abstract
To elucidate the birth defects of children in women received In Vitro Fertilization-Embryo Transfer (IVF-ET) by conducting a meta-analysis. We conducted a systematic literature search to identify original studies of birth defects in IVF-ET before Feb 2016. Eligible studies were retrieved via both computer searches and manual review of references. The summary difference estimates between groups were calculated based on the Weighted Mean Difference (WMD) with its 95% Confidence Interval (CI). Sensitivity and publication analyses were performed after the pooled analysis. A total of 15 original studies of 189376 new born were included in this study. Meta-analysis showed an increased level of birth defects rate in women received IVF-ET (Z=8.67, P<0.01). There was no significant publication bias in the included studies (P for Begg’s test=0.86, P for egger’s test=0.16). Congenital malformation in IVF-ET group was significantly higher than that in the control group (P<0.05) and the level of OR was 1.29 (95% CI, 1.20, 1.41). Our results demonstrated that there was an increased level of birth defects rate in women received IVF-ET.
Keywords
In vitro fertilization-embryo transfer, Birth defects, Meta-analysis.
Introduction
The rate of birth defects following In Vitro Fertilization Embryo Transfer (IVF-ET) varies from 3.4 to 9.0% [1-3]. The comparison of intracytoplasmic sperm injection and IVF children taking part in an identical follow-up study did not show any increased risk of major malformations in the intracytoplasmic sperm injection group [4]. Control selection (national or clinical control) from a different population creates the problem of differences in screening methods [5], management of pregnancy, and perinatal care between cases and controls [1,2]. In both cases, only stratification procedures reveal the influence of assisted reproductive technology on the incidence of birth defects. However, the results between studies were inconsistent [6-8]. In response, we conducted the first meta-analysis by pooling together the results from all published original studies. Our purpose was to examine the rate of birth defects in women received IVF-ET.
Materials and Methods
Literature search
We aimed to identify all publications reporting the rate of birth defects in women received IVF-ET. Our literature search was conducted with a systematic literature search before July 2014. The study was in accordance with Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines [9]. The databases included PubMed, MEDLINE, Springer link, Science Direct, Chinese National Knowledge Internet (CNKI) and EMBASE. The search strategies in our analysis were as following:
In-vitro fertilization or reproduction techniques or intracytoplasmic sperm injection) and (children or child or infant or neonatal) and (birth defects or chromosomal aberrations or chromosome abnormal or congenital malformations. There was no any language restriction of our literature retrieve, while the trial objective should restrict as human. In order to screening additional relevant data, all the potential related references after paper were manually searched. The manual retrieve procedure was performed by two independent investigators. Any ambiguity among the researchers was resolved by consensus and original data.
Criteria for inclusion and exclusion
The mainly included criteria for our study were as following: (i) the study should be an original research, which mentioned the women received IVF-ET and numeric rate of the birth defects. (ii) The primary outcome was presented as birth defects, which can be collected to make a pooled quantitative analysis. (iii) There was controlled group and corresponding quantitative data in original study. The exclusion criteria were: (i) there was no usable data reported. (ii) Duplicates data. (iii) Reviews narrate or comments. (iv) Letters to editors, abstracts in conference or non-peer-reviewed journals.
Data extraction
Two reviewers independently extracted information from each article using standard forms, the extracted data concerned first author, year of publication, location of the study, sample size in controlled group and IVF-ET group, mentioned outcome measures and baseline characteristics. When more than one data were presented in the same study, we separately treated them as different study once the data were no cross effect between different controlled group or IVF-ET group. Any disagreements were resolved by consensus. The primary outcome was urinary nerve growth factor.
Quality assessment
The eligibility of each study was assessed independently by two investigators. We assessed the methodological quality of the studies by means of the previously published recommendations for systematic reviews of observational studies. The key points of the current checklist included the following terms: maintenance of comparable groups, baseline of demography, study design, aim of the study, discussion of possible confounders, data collection and bias. Any study that met fewer than four criteria present should be excluded.
Statistical analysis
All the statistical procedure were performed in STATA software version 12.0 (STATA, College Station, TX, USA). The Weighted Mean Difference (WMD) was used in the evaluation of difference baseline of pregnancy women between controlled group and IVF-ET group. Moreover, the Odds Ratio (OR) also used in the evaluation of ratio of birth defects rate. The 95% Confidence Interval (CI) of OR was calculated to identify the study outcome variation. It is considered statistically significant for outcome measure when the 95% CI excluded zero. Heterogeneity was assessed by the Cochran’s Q test, with a 10% significance level.
On the other hand, the I2 statistic was adopted to interpret the degree of heterogeneity. A fixed effect model was performed in the data comparison section unless the heterogeneity degree was I2>50%, in which case a random effects approach was used to adjust for the combined estimate. Potential publication bias was assessed by Egger’s line regression and Begg’s funnel plot. Sensitivity analysis was performed by excluding the older studies. For all Meta analyses, two side p<0.05 was considered statistically significant.
Results
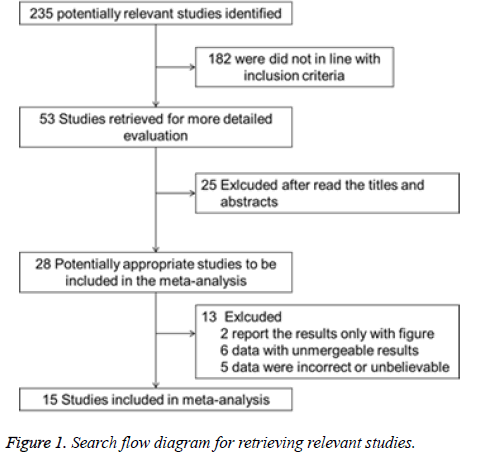
A total of 235 articles were retrieved initially, there were 182 papers were not in line with our inclusion criteria, 25 relative papers were exclusion after read the titles and abstracts. 2 papers of remained 28 studies report the results only with figure, 6 papers report the data with unmergeable results, and data in the other 5 studies were incorrect or unbelievable due to their primary designs. Finally, we identified a total of 15 original studies of 189376 new born mentioned birth defects rate in women received IVF-ET according to our above mentioned criteria [10-24].
A detail flow diagram of our search and selection was shown in Figure 1. Characteristics and quality assessment of these studies are summarized in Table 1.
| Author | No. of women | Measurement terms | Quality | |||
|---|---|---|---|---|---|---|
| IVF-ET | Control | Selective | Comparative | Assessment | ||
| Allen [12] | 1524 | 57922 | Singletons and overall preterm birth, birth weight and birth defects | 3 | 2 | 2 |
| Katalinic [18] | 3372 | 8016 | Congenital malformations, premature birth | 3 | 2 | 2 |
| Shevell [15] | 554 | 34286 | Maternal complications, premature birth, low birth weight, congenital anomalies and chromosomal abnormalities | 4 | 2 | 2 |
| Bonduelle [14] | 977 | 538 | Malformation rate | 4 | 2 | 2 |
| Koivurova [19] | 304 | 569 | Perinatal mortality, premature birth, low birth weight, congenital malformations, neonatal morbidity rates | 4 | 2 | 2 |
| Isaksson [20] | 545 | 2853 | Maternal complications, gestational age of birth, low birth weight, congenital malformation, perinatal deaths | 3 | 2 | 2 |
| Westergaard [22] | 2245 | 2245 | Preterm birth, low birth weight, congenital malformation, perinatal deaths | 4 | 2 | 2 |
| Wennerholm [23] | 255 | 252 | Perinatal situation, the growth in the future | 3 | 2 | 2 |
| Ludwig [21] | 3372 | 30940 | Congenital malformation rate | 3 | 2 | 2 |
| Wennerholm [24] | 258 | 258 | Preterm birth, low birth weight, congenital malformation, perinatal deaths | 3 | 2 | 2 |
| Li [16] | 254 | 1205 | Birth weight and neonatal asphyxia, birth defects | 3 | 2 | 2 |
| Wang [17] | 211 | 213 | Premature birth, low birth weight and multiple pregnancy, birth defects, perinatal death | 3 | 2 | 2 |
| Huang [13] | 101 | 4435 | Premature birth, low birth weight and multiple pregnancy, birth defects, perinatal death | 3 | 2 | 2 |
| Hang [11] | 1904 | 3269 | Multiple pregnancy, abortion rate, rate of premature birth, low birth weight, congenital malformation rate | 4 | 2 | 2 |
| Yu [10] | 1933 | 24561 | Abortion rate, ectopic pregnancy rate, multiple pregnancy rate, rate of premature birth, low birth weight and birth defects | 3 | 2 | 2 |
Table 1. Characteristics of included studies.
A total of 189376 new born were involving in our study. There was no gender, age or Body Mass Index (BMI) dividing in 15 studies. Thus our study cannot make subgroup analysis based on these demographic characteristics. The range of publication year was range from 1997 to 2010.
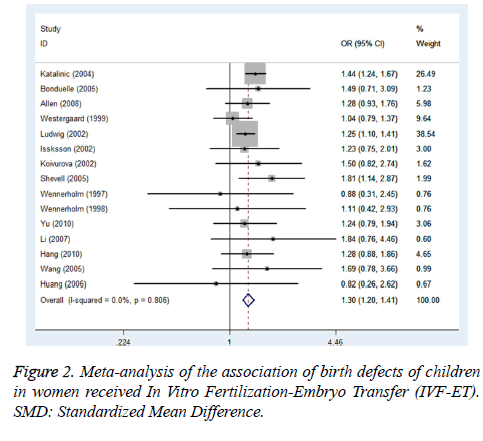
In the selected studies, women received IVF-ET seemed to have a high birth defects when compared with controlled groups (OR=1.29, 95% CI: 1.20 ~ 1.41; z=6.48, P<0.01; Figure 2).
We also conducted a sensitivity analysis to investigate the robustness of our findings. In our analysis, we excluded the oldest study published by Wennerholm in 1997.
The result showed that the difference between groups was as same as previous (OR=1.34, 95% CI: 1.26 to 1.49; z=8.67, P<0.01).
We were able to assess publication bias in the primary outcome. The degree of asymmetry was not statistically significant by both Begg’s test and Egger’s line regression (P for Begg’s test=0.71, P for egger’s test=0.38).
Discussion
The first test tube baby in the world, Louise Brown, was born on 25th July 1978 after In-Vitro Fertilization and Embryo Transfer Technique (IVF-ET) by Edwards et al. in Oldham, England [25]. A few days after the delivery of the first test tube baby in United Kingdom., an Indian team from Kolkata led by (Late) Dr. Subhas, an excellent cryobiologist and (Late) Dr. Saroj, a well-known gynaecologist–announced the birth of ‘Durga’ [26], following a test tube baby procedure, on 3rd October 1978. Developmental defects in the enamel present important clinical significance since they are responsible for aesthetic problems, dental sensitivity, dentofacial anomalies, as well as for a predisposition to dental caries [27]. In the field of public health, developmental defects in the enamel have taken on a high level of importance for being predictors of dental caries. Populations affected by these changes require as a priority preventive intervention and early treatment. There are very few epidemiological studies done on the prevalence of developmental defects in the enamel of deciduous dentition. The prevalence rates of developmental defects in the children showed great variability.
We have pooled all available related evidence to discuss the birth defects of women received IVF-ET through the metaanalysis method. In this analysis, we identified that the birth defects rate were significantly higher in women received IVFET than that in controlled participants. To the best of our knowledge, there is no a comprehensive assessment of the relation mentioned birth defects of women received IVF-ET. This is the first meta-analysis of original studies on the potential difference of birth defects in women received IVFET. Our present study is a meta-analysis based on the clinical trial which included 189376 participants. As we know, prevalence study is undertaken to support the existence of association between suspected cause and disease. While the prospective cohort study does not be interfered by investigators and it is more suitable for long-term follow-up and owns high strength evidence. Whereas, RCT often needs to be end at the scheduled termination time, and the follow-up time is often shorter. On the other hand, a well-designed diagnostic study always can minimize the interference or potential confounding factors of the participants through the corrected multivariable analyses. While these function cannot be conducted in a RCT study.
Use of matched controls to evaluate the perinatal effects of IVF-ET on the incidence of major birth defects demonstrates that the risk because of the method itself is minimal. The matching procedure for establishment of a control group will clearly most closely reflect the relative risk of the assisted reproductive technology method. Differences in absolute risk of congenital abnormalities can be influenced by maternal age, certain maternal diseases, medications, toxic habits, environmental toxic effects and population variation. The different prenatal screening methods applied (e.g., nuchal translucency, chorionic biopsy) and national guiding principles concerning prenatally detected malformations can also significantly modify the perinatal outcome concerning congenital anomalies. Therefore, it is very important to collect safety data prospectively as assisted reproductive technology has been showing a dramatic increase worldwide in infertility therapy.
In summary, our meta-analysis of all relevant original studies showed a significant increase rate of birth defects in women received IVF-ET. While the further studies are also required to better confirm the findings.
Acknowledgement
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest Statement
The authors declare no conflict of interest in preparing this article.
References
- Chen H, Wang Y, Lyu Q, Ai A, Fu Y, Tian H, Cai R, Hong Q, Chen Q, Shoham Z, Kuang Y. Comparison of live-birth defects after luteal-phase ovarian stimulation vs. conventional ovarian stimulation for in vitro fertilization and vitrified embryo transfer cycles. Fertil Steril 2015; 103: 1194-1201.
- Ooki S. Birth defects after assisted reproductive technology according to the method of treatment in Japan: nationwide data between 2004 and 2012. Environ Health Prev Med 2015; 20: 460-465.
- Jwa J, Jwa SC, Kuwahara A, Yoshida A, Saito H. Risk of major congenital anomalies after assisted hatching: analysis of three-year data from the national assisted reproduction registry in Japan. Fertil Steril 2015; 104: 71-78.
- Unuane D, Velkeniers B, Deridder S, Bravenboer B, Tournaye H, De Brucker M. Impact of thyroid autoimmunity on cumulative delivery rates in in vitro fertilization/intracytoplasmic sperm injection patients. Fertil Steril 2016; 106: 144-150.
- Jawed S, Rehman R, Ali MA, Abdullah UH, Gul H. Fertilization rate and its determinants in intracytoplasmic sperm injection. Pak J Med Sci 2016; 32: 3-7.
- Jin R, Bao J, Tang D, Liu F, Wang G, Zhao Y. Outcomes of intracytoplasmic sperm injection using the zona pellucida-bound sperm or manually selected sperm. J Assist Reprod Genet 2016; 33: 597-601.
- Wei LH, Ma WH, Tang N, Wei JH. Luteal-phase ovarian stimulation is a feasible method for poor ovarian responders undergoing in vitro fertilization/intracytoplasmic sperm injection-embryo transfer treatment compared to a GnRH antagonist protocol: A retrospective study. Taiwan J Obstet Gynecol 2016; 55: 50-54.
- Torki-Boldaji B, Tavalaee M, Bahadorani M, Nasr-Esfahani MH. Selection of physiological spermatozoa during intracytoplasmic sperm injection. Andrologia 2016.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000; 283: 2008-2012.
- Yu H. The birth outcomes birth pregnancy complications of in-vitro fertilization embryo transplantation. China Med Univ 2010; 33.
- Hang F. The study on security of assisted reproductive technology. Huazhong Univ Sci Technol 2010; 87.
- Allen C, Bowdin S, Harrison RF, Sutcliffe AG, Brueton L, Kirby G, Kirkman-Brown J, Barrett C, Reardon W, Maher E. Pregnancy and perinatal outcomes after assisted reproduction: a comparative study. Ir J Med Sci 2008; 177: 233-241.
- Huang S, Liao C, Wei J, Chen Z. Analysis of the birth outcome of assisted reproductivete chnology. J Reprod Med 2006; 15: 241-243.
- Bonduelle M, Wennerholm UB, Loft A, Tarlatzis BC, Peters C, Henriet S, Mau C, Victorin-Cederquist A, Van Steirteghem A, Balaska A, Emberson JR, Sutcliffe AG. A multi-centre cohort study of the physical health of 5-year-old children conceived after intracytoplasmic sperm injection, in vitro fertilization and natural conception. Hum Reprod 2005; 20: 413-419.
- Shevell T, Malone FD, Idaver J, Porter TF, Luthy DA, Comstock CH, Hankins GD, Eddleman K, Dolan S, Dugoff L, Craigo S, Timor IE, Carr SR, Wolfe HM, Bianchi DW, DAlton ME. Assisted reproductive technology and pregnancy outcome. Obstet Gynecol 2005; 106: 1039-1045.
- Li F, Wu W, Zou S, Wu R, Song D. Neonatal outcome of children born after in-vitro fertilization- embryotransfer. Br J Obstet Gynaecol 2005; 13: 83-84, 88.
- Wang X, Chang Y, Zhao X. Study on the neonatal outcomes and congenital malformations in children born after in-vitro fertilization. China J Perinat Med 2005; 8: 246-250.
- Katalinic A, Rosch C, Ludwig M. Pregnancy course and outcome after intracytoplasmic sperm injection: a controlled, prospective cohort study. Fertil Steril 2004; 81: 1604-1616.
- Koivurova S, Hartikainen AL, Gissler M, Hemminki E, Sovio U, Järvelin MR. Neonatal outcome and congenital malformations in children born after in-vitro fertilization. Hum Reprod 2002; 17: 1391-1398.
- Isaksson R, Gissler M, Tiitinen A. Obstetric outcome among women with unexplained infertility after IVF: A matched case-control study. Hum Reprod 2002; 17: 1755-1761.
- Ludwig M, Katalinic A. Malformation rate in foetuses and children conceived after ICSI: results of a prospective cohort study. Reprod Biomed 2002; 5: 171-178.
- Westergaard HB, Johansen AM, Erb K, Andersen AN. Danish National In-Vitro Fertilization Registry 1994 and 1995: A controlled study of births, malformations and cytogenetic findings. Hum Reprod 1999; 14: 1896-1902.
- Wennerholm UB, Albertsson-Wikland K, Bergh C, Hamberger L, Niklasson A, Nilsson L. Postnatal growth and health in children born after cryopreservation as embryos. Lancet 1998; 351: 1085-1090.
- Wennerholm UB, Hamberger L, Nilsson L, Wennergren M, Wikland M, Bergh C. Obstetric and perinatal outcome of children conceived from cryopreserved embryos. Hum Reprod 1997; 12: 1819-1825.
- Kamel RM. Assisted reproductive technology after the birth of louise brown. J Reprod Infertil 2013; 14: 96-109.
- Kaur H, Chelmala S, Srinivasulu B, Shah TA, Devender G, Srinivasulu A. Taxonomic notes and distribution extension of Durga Dass leaf-nosed bat Hipposiderosdurgadasi Khajuria, 1970 (Chiroptera: Hipposideridae) from south India. Biodivers Data J 2014; e4127.
- Feldens CA, Dos SDA, Kramer PF, Scapini A, Busato AL, Vargas-Ferreira F. Impact of malocclusion and dentofacial anomalies on the prevalence and severity of dental caries among adolescents. Angle Orthod 2015; 85: 1027-1034.