Research Article - Biomedical Research (2017) Volume 28, Issue 4
Biomechanical comparison between anterior cervical discectomy with fusion and without fusion
Andrei Stefan Iencean1,2 Stefan Mircea Iencean3* and Ion Poeata2,31Gr T Popa University of Medicine and Pharmacy Iasi, Universitatii St., Iasi, Romania
2Department of Neurosurgery, N Oblu Emergency Hospital Iasi, Ateneului St. Iasi, Romania
3Department of Neurosurgery, Gr T Popa University of Medicine and Pharmacy Iasi, Universitatii St., Iasi, Romania
- *Corresponding Author:
- Iencean Stefan Mircea
Department of Neurosurgery
Gr T Popa University of Medicine and Pharmacy Iasi, Romania
Accepted on September 15, 2016
Abstract
The aim of this study is to compare patients undergoing one level anterior cervical discectomy without fusion versus anterior cervical discectomy with fusion. The study included forty-eight patients operated at either C5-C6 level or at the C6-C7 level: a group of anterior cervical microdiscectomy without fusion performed at one level on 24 consecutive patients was matched to a second group of 24 patients with single-level of anterior cervical discectomy with fusion, based on level, age and sex. The kinematic analysis included the range of motion, intervertebral angulations, anteroposterior translation and disc height assessed for the cervical functional spinal units at the operated level and adjacent levels. At the operated level the range of motion and the translation were minimal in the anterior cervical discectomy without fusion group, both for the C5-C6 and C6-C7 levels, and absent in the cervical discectomy with fusion group. The superior adjacent levels range of motion and the translation were greater in the ACDF group compared with the ACD group. The clinical results of anterior cervical microdiscectomy without fusion and anterior cervical discectomy with fusion were comparable. In cervical microdiscectomy without fusion the elastic fibrous intradiscal scar at the operated level allows a small degree of mobility and the adjacent cervical levels are not overstressed. No need for anterior cervical discectomy with fusion to trait a single level cervical disc herniation than in selected cases.
Keywords
Anterior cervical discectomy without fusion, Anterior cervical discectomy with fusion, Elastic fibrous intradiscal scar, Intervertebral translation.
Introduction
Cervical disc herniation is a common pathology of the cervical spine and the surgical treatment can be Anterior Cervical Discectomy without fusion (ACD), Anterior Cervical Discectomy and Spinal Fusion (ACDF), posterior cervical discectomy, anterior or posterior foraminotomy, percutaneous cervical nucleoplasty or cervical artificial disc replacement. Anterior Cervical Discectomy without fusion (ACD) and Anterior Cervical Discectomy with Fusion (ACDF) are common approaches among spine surgeons for most cervical herniated discs [1,2].
The anterior cervical decompression with fusion with a bone graft harvested from the iliac crest began to be used during the years 1955-1959, and since 1975 anterior microdiscectomy without fusion for cervical disc herniation was introduced. Many variations of the cervical anterior approaches have been presented over the last six decades such as: microdiscectomy; discectomy and fusion (autologous or homologous graft; intersomatic spacer-metallic, biological polymers; bone inductors; with plates) [2-4].
These surgical treatments lead to the decompression of compressed neural elements and the stability of the cervical spine, without abnormal movements. Most spine surgeons consider that the anterior cervical discectomy without fusion must be limited to one space, rather than multiple spaces. Also it is believed that the anterior cervical discectomy with fusion may lead to acceleration of degenerative changes at the immediately adjacent discal levels secondary to abnormal spinal motion [5-7]. The cervical intervertebral disc should not be entirely removed in anterior cervical discectomy without fusion and the cartilaginous endplates should be left intact, but the entire cervical disc should be removed and the vertebral body endplates must be decorticated in anterior cervical discectomy with fusion. Most spine surgeons consider that the results of these two types of approaches (ACD and ACDF) are comparable both in terms of the decompression and the cervical stability [8-10]. The healing after the microdiscectomy without fusion leads to an intradiscal fibrous scar and not a real bone fusion because the cartilaginous endplates should be left intact in ACD.
We tried to determine the kinematic differences of anterior cervical discectomy without fusion versus anterior cervical discectomy with fusion in a prospective study.
Material and Methods
We performed a prospective kinematic comparative study between 2011 and 2015 of patients undergoing one level anterior cervical discectomy without fusion versus anterior cervical discectomy with fusion. The study included forty-eight patients operated at either C5-C6 level or at the C6-C7 level: a group of anterior cervical microdiscectomy without fusion performed at one level on 24 consecutive patients was matched to a second group of 24 patients with single-level of anterior cervical discectomy with fusion based on level, age and sex.
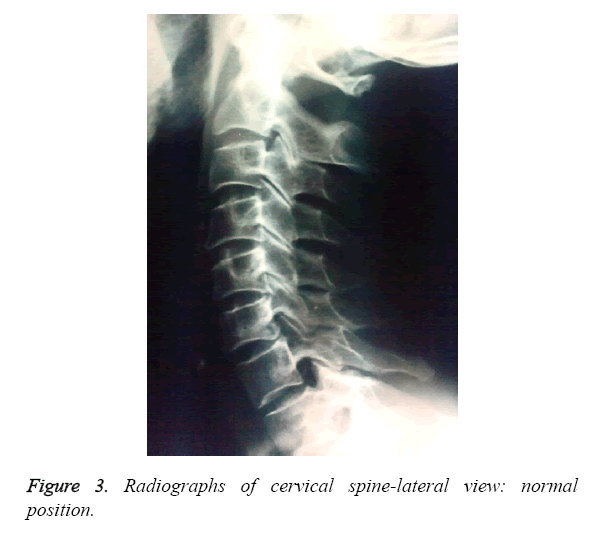
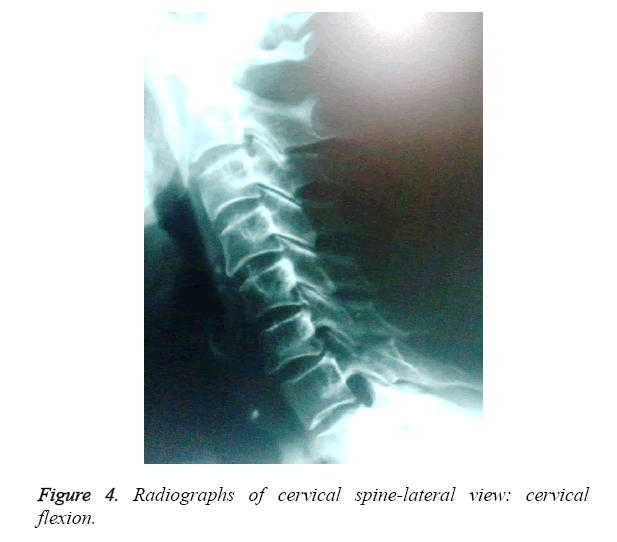
Inclusion criteria for the ACD and ACDF groups: all patients included for the ACD and ACDF groups presented with clinical symptoms due to one level herniated cervical disc; all patients had preoperative complete general and neurological examination, they had preoperative MRI and plain radiographs of the cervical spine anterio-posterior, lateral neutral, flexion and extension obtained preoperatively. As exclusion criteria: the patients with clinical or imagistic evidence (MRI, X-rays) of additional diseased cervical spine, history of cervical spinal injury were excluded from the study. Also the patients with cervical instability at the level of disc herniation, which need a possible fusion and fixation, were excluded from the group of ACD patients.
The same surgical team performed ACD: microdiscectomy with the cartilaginous endplates left intact and anterior foraminotomy and ACDF too: the entire disc removed, the vertebral body endplates decorticated and used a Peek cage and no fixation with plate and screws.
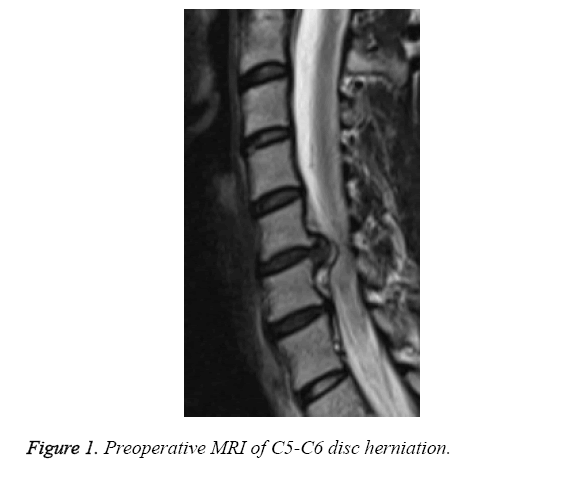
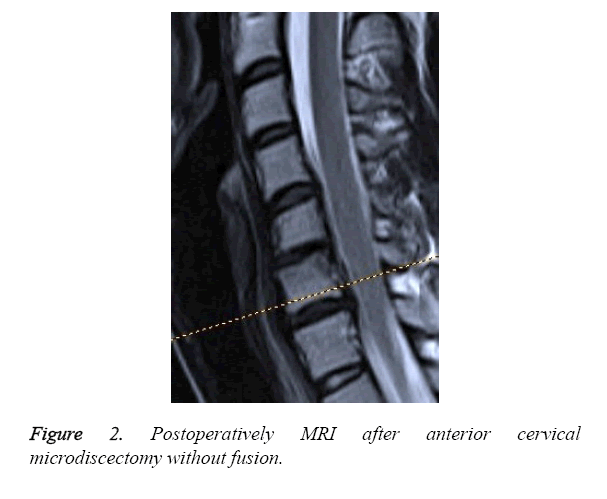
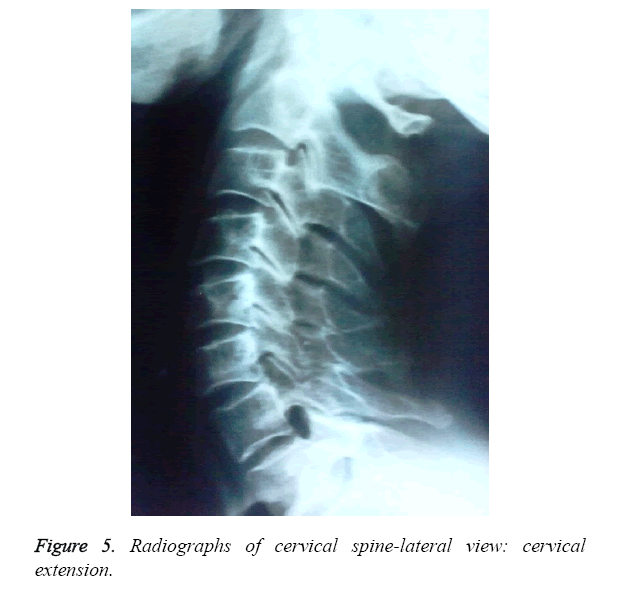
The patients had cervical MRI at one year postoperatively and lateral neutral, flexion and extension cervical x-rays at one year intervals postoperatively (Figures 1-5). The study selection criteria and outcome measures were identical, with the exception being the surgical technique: anterior cervical microdiscectomy without fusion and anterior cervical discectomy with fusion.
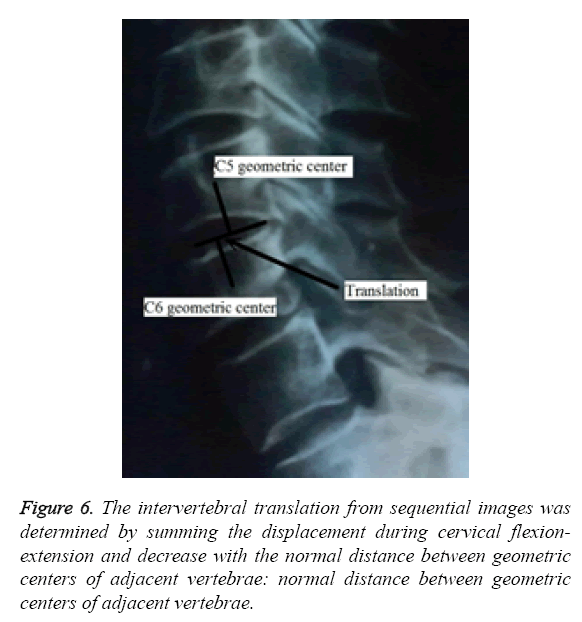
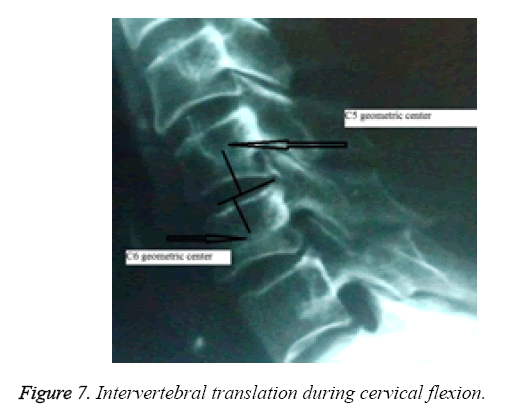
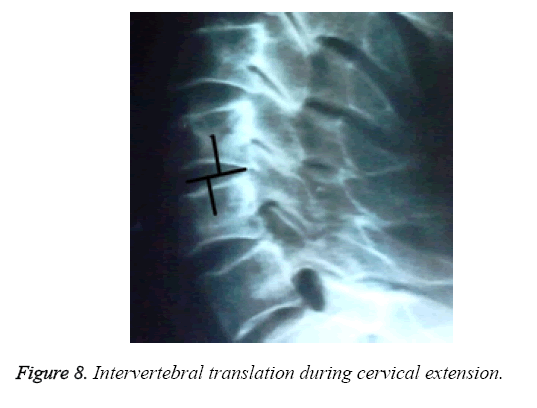
The kinematic analysis included the range of motion, intervertebral angulations, antero-posterior translation and disc height assessed for the cervical functional spinal units at the operated level and adjacent levels. The intervertebral translation studied during flexion and extension movements was the sum of the anterior and posterior translations of the cervical spine (Figures 6-8) [11]. The measurements of preoperative and postoperative anterior-posterior translation of the operated level and of the superjacent levels were compared between the groups of ACD and ACDF. Thus the translations of C3C4 level and C4C5 level were compared for the C5C6 operated level with the same level translation between the groups of ACD and ACDF. Likewise the translations of C3C4 level, C4C5 level and C5C6 level were compared for the C6C7 operated level between the two groups. The intervertebral translations were measured in millimeters on the converted digital radiographies using DICOM viewer software. These parameters were studied in the matched patients from both groups using the statistical averages, standard deviations, the paired Student's t-test and p-value for statistical significance.
All patients gave their written informed consent before the start of the study and the ethics committee approved the study protocol.
Results
A total of forty-eight patients were analysed, included in two groups in pairs, each group of 24 patients of anterior cervical discectomy without fusion and with fusion performed at one level during four years. Table 1 presents the demographic data of these patients. The distribution of patients by age, sex and level of disc herniation is not significant because the cases were selected to match according to the type of surgery.
| Age | ACD / ACDF C5-C6 | ACD / ACDF C6-C7 | |||
|---|---|---|---|---|---|
| M | F | M | F | ||
| 36-39 | 2 | 1 | 1 | 1 | |
| 40-49 | 3 | 1 | 3 | 2 | |
| 50-58 | 2 | 2 | 3 | 2 | |
| Total | 8 | 4 | 7 | 5 | |
Table 1. Demographic data of patients for each group of discectomy (in pairs).
The clinical results of these two types of approaches were comparable. The values of the intervertebral translations one year postoperatively at C3-C4, C4-C5 and C5-C6 levels during cervical flexion and extension at patients operated at C5-C5 disc herniation for ACD and ACDF groups are presented in Table 2. Table 3 presents the values of the intervertebral translations one year postoperatively at C3-C4, C4-C5, C5-C6 and C6-C7 levels during cervical flexion and extension at patients operated for C6-C7 disc herniation for ACD and ACDF groups.
| Operated Level | Measured Levels | Discectomy without fusion (D) | Discectomy with fusion (DF) | ||||
|---|---|---|---|---|---|---|---|
| Preoperative Translation | Postoperative Translation | ΔD | Preoperative Translation | Postoperative Translation | ΔDF | ||
| C5-C6 | C3-C4 | 1.9 mm | 2.3 mm | 0.4 mm | 1.9 mm | 2.4 mm | 0.5 mm |
| C4-C5 | 1.8 mm | 2.0 mm | 0.2 mm | 2.1 mm | 2.4 mm | 0.3 mm | |
| C5-C6 | 1.3 mm | 0.5 mm | -0.8 mm | 1.3 mm | 0.0 mm | -1.3 mm | |
| C5-C6 | C3-C4 | 1.9 mm | 2.5 mm | 0.6 mm | 1.9 mm | 2.6 mm | 0.7 mm |
| C4-C5 | 2.2 mm | 2.5 mm | 0.3 mm | 2.0 mm | 2.4 mm | 0.4 mm | |
| C5-C6 | 1.7 mm | 0.2 mm | -1.5 mm | 1.7 mm | 0.0 mm | -1.7 mm | |
| C5-C6 | C3-C4 | 2.2 mm | 2.7 mm | 0.5 mm | 2.2 mm | 2.9 mm | 0.7 mm |
| C4-C5 | 2.1 mm | 2.5 mm | 0.4 mm | 2.1 mm | 2.6 mm | 0.5 mm | |
| C5-C6 | 1.5 mm | 0.4 mm | -1.1 mm | 1.5 mm | 0.0 mm | -1.5 mm | |
| C5-C6 | C3-C4 | 1.9 mm | 2.3 mm | 0.4 mm | 1.9 mm | 2.7 mm | 0.8 mm |
| C4-C5 | 2.0 mm | 2.4 mm | 0.4 mm | 2.0 mm | 2.5 mm | 0.5 mm | |
| C5-C6 | 1.9 mm | 0.7 mm | -1.2 mm | 1.6 mm | 0.0 mm | -1.6 mm | |
| C5-C6 | C3-C4 | 1.9 mm | 2.4 mm | 0.5 mm | 1.9 mm | 2.8 mm | 0.9 mm |
| C4-C5 | 2.1 mm | 2.5 mm | 0.4 mm | 2.1 mm | 2.6 mm | 0.5 mm | |
| C5-C6 | 1.3 mm | 0.4 mm | -0.9 mm | 1.3 mm | 0.0 mm | -1.3 mm | |
| C5-C6 | C3-C4 | 1.7 mm | 2.1 mm | 0.4 mm | 1.7 mm | 2.5 mm | 0.8 mm |
| C4-C5 | 2.2 mm | 2.4 mm | 0.2 mm | 2.1 mm | 2.4 mm | 0.3 mm | |
| C5-C6 | 2.1 mm | 0.3 mm | -1.8 mm | 1.3 mm | 0.0 mm | -1.3 mm | |
| C5-C6 | C3-C4 | 1.8 mm | 2.3 mm | 0.5 mm | 1.9 mm | 2.6 mm | 0.7 mm |
| C4-C5 | 2.1 mm | 2.3 mm | 0.2 mm | 2.2 mm | 2.6 mm | 0.4 mm | |
| C5-C6 | 1.9 mm | 0.8 mm | -1.1 mm | 1.2 mm | 0.0 mm | -1.2 mm | |
| C5-C6 | C3-C4 | 1.8 mm | 2.3 mm | 0.5 mm | 1.8 mm | 2.7 mm | 0.9 mm |
| C4-C5 | 2.1 mm | 2.4 mm | 0.3 mm | 2.1 mm | 2.5 mm | 0.4 mm | |
| C5-C6 | 1.6 mm | 0.6 mm | -1.0 mm | 1.3 mm | 0.0 mm | -1.3 mm | |
| C5-C6 | C3-C4 | 1.9 mm | 2.4 mm | 0.5 mm | 1.9 mm | 2.6 mm | 0.7 mm |
| C4-C5 | 2.1 mm | 2.3 mm | 0.2 mm | 1.9 mm | 2.2 mm | 0.3 mm | |
| C5-C6 | 1.6 mm | 1.0 mm | -0.6 mm | 1.1 mm | 0.0 mm | -1.1 mm | |
| C5-C6 | C3-C4 | 2.2 mm | 2.5 mm | 0.3 mm | 2.1 mm | 2.7 mm | 0.6 mm |
| C4-C5 | 1.9 mm | 2.2 mm | 0.3 mm | 1.9 mm | 2.3 mm | 0.4 mm | |
| C5-C6 | 1.7 mm | 0.5 mm | -1.2 mm | 1.5 mm | 0.0 mm | -1.5 mm | |
| C5-C6 | C3-C4 | 1.8 mm | 2.4 mm | 0.6 mm | 1.8 mm | 2.7 mm | 0.9 mm |
| C4-C5 | 2.1 mm | 2.5 mm | 0.4 mm | 2.1 mm | 2.6 mm | 0.5 mm | |
| C5-C6 | 1.8 mm | 0.4 mm | -1.4 mm | 1.6 mm | 0.0 mm | -1.6 mm | |
| C5-C6 | C3-C4 | 2.1 mm | 2.6 mm | 0.5 mm | 2.1 mm | 2.9 mm | 0.8 mm |
| C4-C5 | 1.9 mm | 2.2 mm | 0.3 mm | 1.9 mm | 2.3 mm | 0.4 mm | |
| C5-C6 | 1.3 mm | 0.3 mm | -1.0 mm | 1.3 mm | 0.0 mm | -1.3 mm | |
| Δ(mm)=Postoperative translation-Preoperative translation | |||||||
Table 2. The preoperative and postoperative intervertebral translations during cervical flexion and extension for operated C5-C6 disc herniation: discectomy without fusion and discectomy with fusion.
| Operated level | Measured levels | Discectomy without fusion (D) | Discectomy with fusion (DF) | ||||
|---|---|---|---|---|---|---|---|
| Preoperative translation | Postoperative translation | ΔD | Preoperative translation | Postoperative translation | ΔDF | ||
| C6-C7 | C3-C4 | 1.9 mm | 2.2 mm | 0.3 mm | 1.8 mm | 2.6 mm | 0.8 mm |
| C4-C5 | 2.1 mm | 2.3 mm | 0.2 mm | 2.2 mm | 2.6 mm | 0.4 mm | |
| C5-C6 | 1.4 mm | 1.5 mm | 0.1 mm | 1.7 mm | 2.0 mm | 0.3 mm | |
| C6-C7 | C6-C7 | 0.4 mm | 0.0 mm | -0.4 mm | 0.6 mm | 0.0 mm | -0.6 mm |
| C3-C4 | 1.7 mm | 2.0 mm | 0.3 mm | 1.8 mm | 2.5 mm | 0.7 mm | |
| C4-C5 | 1.9 mm | 2.3 mm | 0.3 mm | 1.8 mm | 2.3 mm | 0.5 mm | |
| C6-C7 | C5-C6 | 1.3 mm | 1.5 mm | 0.2 mm | 1.3 mm | 1.5 mm | 0.2 mm |
| C6-C7 | 0.7 mm | 0.2 mm | -0.5 mm | 0.7 mm | 0.0 mm | -0.7 mm | |
| C3-C4 | 1.9 mm | 2.3 mm | 0.4 mm | 1.8 mm | 2.6 mm | 0.8 mm | |
| C4-C5 | 2.2 mm | 2.6 mm | 0.4 mm | 2.1 mm | 2.6 mm | 0.5 mm | |
| C5-C6 | 1.7 mm | 1.9 mm | 0.2 mm | 1.9 mm | 2.1 mm | 0.2 mm | |
| C6-C7 | 1.1 mm | 0.1 mm | -1.0 mm | 1.1 mm | 0.0 mm | -1.1 mm | |
| C6-C7 | C3-C4 | 1.7 mm | 1.9 mm | 0.2 mm | 1.9 mm | 2.7 mm | 0.8 mm |
| C4-C5 | 1.9 mm | 2.3 mm | 0.4 mm | 1.8 mm | 2.4 mm | 0.6 mm | |
| C5-C6 | 1.5 mm | 1.7 mm | 0.2 mm | 1.4 mm | 1.7 mm | 0.3 mm | |
| C6-C7 | C6-C7 | 0.9 mm | 0.2 mm | -0.7 mm | 0.8 mm | 0.0 mm | -0.8 mm |
| C3-C4 | 1.8 mm | 2.1 mm | 0.3 mm | 1.9 mm | 2.6 mm | 0.7 mm | |
| C4-C5 | 1.9 mm | 2.3 mm | 0.4 mm | 1.7 mm | 2.3 mm | 0.6 mm | |
| C6-C7 | C5-C6 | 1.4 mm | 1.6 mm | 0.2 mm | 1.5 mm | 1.8 mm | 0.3 mm |
| C6-C7 | 1.3 mm | 0.2 mm | -1.1 mm | 1.1 mm | 0.0 mm | -1.1 mm | |
| C3-C4 | 2.1 mm | 2.3 mm | 0.2 mm | 2.2 mm | 2.7 mm | 0.5 mm | |
| C4-C5 | 2.1 mm | 2.5 mm | 0.4 mm | 2.0 mm | 2.5 mm | 0.5 mm | |
| C5-C6 | 1.4 mm | 1.5 mm | 0.1 mm | 1.4 mm | 1.6 mm | 0.2 mm | |
| C6-C7 | 0.7 mm | 0.2 mm | -0.5 mm | 0.7 mm | 0.0 mm | -0.7 mm | |
| C6-C7 | C3-C4 | 1.9 mm | 2.4 mm | 0.5 mm | 1.8 mm | 2.5 mm | 0.7 mm |
| C4-C5 | 1.8 mm | 2.2 mm | 0.4 mm | 1.9 mm | 2.4 mm | 0.5 mm | |
| C5-C6 | 1.7 mm | 1.8 mm | 0.1 mm | 1.7 mm | 1.9 mm | 0.2 mm | |
| C6-C7 | C6-C7 | 1.2 mm | 0.3 mm | -0.9 mm | 1.2 mm | 0.0 mm | -1.2 mm |
| C3-C4 | 1.7 mm | 1.9 mm | 0.3 mm | 1.8 mm | 2.2 mm | 0.4 mm | |
| C4-C5 | 1.9 mm | 2.1 mm | 0.2 mm | 1.9 mm | 2.4 mm | 0.6 mm | |
| C6-C7 | C5-C6 | 1.3 mm | 1.4 mm | 0.1 mm | 1.2 mm | 1.4 mm | 0.2 mm |
| C6-C7 | 0.8 mm | 0.2 mm | -0.6 mm | 0.9 mm | 0.0 mm | -0.9 mm | |
| C3-C4 | 1.8 mm | 2.3 mm | 0.4 mm | 1.9 mm | 2.5 mm | 0.6 mm | |
| C4-C5 | 2.0 mm | 2.5 mm | 0.5 mm | 2.1 mm | 2.6 mm | 0.5 mm | |
| C5-C6 | 1.4 mm | 1.6 mm | 0.2 mm | 1.5 mm | 1.7 mm | 0.2 mm | |
| C6-C7 | 1.2 mm | 0.1 mm | -1.1 mm | 1.3 mm | 0.0 mm | -1.3 mm | |
| Δ(mm)=Postoperative translation-Preoperative translation | |||||||
Table 3. The preoperative and postoperative intervertebral translations during cervical fexion and extension for operated C6-C7 disc herniation: discectomy without fusion and discectomy with fusion.
At the operated level the range of motion and the translation were present in the ACD group, for operated level, C5-C6 and C6-C7 and were absent in the ACDF group. The statistical averages of the preoperative intervertebral translations of C3- C4 and C4-C5 levels for operated C5-C6 level were equal each level for both type of surgery and also they are very similar for operated C6-C7 level in ACD and ACDF. The statistical analysis using Student's t-test of these postoperative intervertebral translations of superjacent levels of operated level by these two types of surgery found a p-value <0.01, therefore a very good statistical significance as shown in Table 4.
| Operated level |
Measured levels |
ACD | ACDF | Δ | Normal (mean) |
|---|---|---|---|---|---|
| C5-C6 | C3 - C4 | 2.4 | 2.675 | 0.27 | 2.1 |
| C4 - C5 | 2.35 | 2.45 | 0.10 | 2.5 | |
| C5 - C6 | 0.51 | 0 | - | 2.2 | |
| C6-C7 | C3-C4 | 2.11 | 2.45 | 0.34 | 2.1 |
| C4-C5 | 2.25 | 2.4 | 0.15 | 2.5 | |
| C5-C6 | 1.54 | 1.67 | 0.13 | 2.2 | |
| C6-C7 | 0.14 | 0 | - | 1.3 | |
| p<0.01 | |||||
Table 4. The mean values of the postoperatively intervertebral translations during cervical flexion and extension for operated C5- C6 / C6-C7 disc herniation.
The comparison of superjacent translations for the fusion at C5-C6 and C6-C7 levels found that the inferior level fusion (C6-C7) produced a higher increase in the C3-C4 level translation.
The range of motion and the translation were greater at superjacent levels in the ACDF group compared with the ACD group.
Discussion
Anterior Cervical Microdiscectomy without fusion (ACD) and Anterior Cervical Discectomy with Fusion (ACDF) are the most commonly used approaches in cervical disc herniation. Most spine surgeons consider that the clinical results of these two types of approaches are comparable, and also the postoperatively cervical stability as well [8,10,12]. Some spine surgeons consider that the anterior cervical microdiscectomy without fusion must be limited only to one space. Also most spine surgeons consider that the anterior cervical discectomy with fusion may lead to acceleration of degenerative changes at immediately adjacent discal levels secondary to abnormal spinal motion [12-14].
In this study we determined the differences in the intervertebral translations one year postoperatively after anterior cervical microdiscectomy without fusion versus anterior cervical discectomy with fusion in two groups in pairs, each of 24 patients.
The comparison of our results with the normal data showed the translation was present in the ACD group at both operated levels and the translation was absent in the ACDF group at the operated level. The absence of intervertebral translation at the operated level is explained by intervertebral fusion in the ACDF group. The presence of lower values of intervertebral translation at the operated level in the ACD group is normal and is not a spinal instability. The healing at the operated level after the ACD consists of an intradiscal fibrous scar and not a real bone fusion because the cartilaginous endplates should be left intact. This elastic fibrous intradiscal scar ensures the cervical stability and allows a small degree of mobility at the operated level in the ACD group.
In the ACD group the means of the intervertebral translation were close to normal values at superjacent levels and in the ACDF group the intervertebral translation was greater compared with the normal values and with the ACD group. Also the comparison of superjacent translations found that the C6-C7 level fusion produced a higher increase in the C3-C4 level translation than the C5-C6 level fusion, therefore the range of motion is higher at a more distant level where the amplitude of movement may be higher. These results may explain why ACDF may lead to acceleration of degenerative changes at immediately overstressed superjacent discal levels secondary to abnormal spinal motion.
In our study the clinical results of these two types of anterior cervical approaches were comparable and this result is consistent with the literature. Nandoe et al. presented the long term outcome of a large series of patients after anterior cervical discectomy without fusion and compared that to results published on the long-term outcome after ACDF.
Their results showed that ACD surgery is comparable to the results of ACDF. Also they concluded "because the superiority of any fusion procedure has never been proven, it has been suggested that fusion might not be necessary at all" [15].
Botelho et al. studied the effectiveness of ACD compared with ACDF and concluded that the clinical results of ACD and ACDF are not significantly different, the addition of the intervertebral cage can enhance clinical results and the anterior cervical plate does not change the clinical results of ACD. Also they noted that ACD produces lower rate of fusion than ACDF, but in ACD there is not a real fusion, there is an elastic fibrous intradiscal scar that ensures a very good cervical stability at the operated level [16].
Kim et al. analysed the whole spine sagittal alignment after ACDF and concluded that the fusion procedure affects the spine sagittal alignment: cervical lordosis decreased especially in patients with high cervical lordosis and the sagittal vertical axis decreased [17].
Our results and the review of the literature show that ACD has comparable clinical results with ACDF in single level cervical disc herniation and ACD ensures postoperatively a very good cervical stability.
Conclusions
The clinical results of anterior cervical microdiscectomy without fusion and anterior cervical discectomy with fusion were comparable. In anterior cervical microdiscectomy without fusion the elastic fibrous intradiscal scar at the operated level allows a small degree of mobility and the adjacent cervical levels are not overstressed. Anterior cervical discectomy with fusion may lead to acceleration of degenerative changes at immediately overstressed adjacent discal levels secondary to greater intervertebral translation at these adjacent levels.
No need for anterior cervical discectomy with fusion to trait a single level cervical disc herniation than in selected cases with preoperative instability at same level. Anterior cervical microdiscectomy without fusion is a valid option in patients with one level cervical disc herniation without local instability.
References
- Sugawara T. Anterior cervical spine surgery for degenerative disease: A review.
- Neurol Med Chir 2015; 55: 540-546.
- Gebremariam L, Koes BW, Peul WC, Huisstede BM. Evaluation of treatment effectiveness for the herniated cervical disc: A systematic review. Spine 2012; 37: E109-118.
- Caruso R, Pesce A, Marrocco L, Wierzbicki V. Anterior approach to the cervical spine for treatment of spondylosis or disc herniation: Long-term results. Comparison between ACD, ACDF, TDR. Clin Ter 2014; 165: e263-270.
- Song KJ, Choi BY. Current concepts of anterior cervical discectomy and fusion: A review of literature. Asian Spine J 2014; 8: 531-539.
- Yang J, Hai Y, Pang C, Li H, Zu D, Zhu G, Xia X, Pei B. Biomechanical study on the effect of the length of cervical anterior fusion on adjacent levels. Zhonghua Wai Ke Za Zhi 2014; 52: 692-696.
- Xia LZ, Zheng YP, Xu HG, Liu P. Effect of anterior cervical discectomy and fusion on adjacent segments in rabbits. Int J Clin Exp Med 2014; 7: 4291-4299.
- Oktenoglu T, Cosar M, Ozer AF, Iplikcioglu C, Sasani M, Canbulat N,Sarioglu AC. Anterior cervical microdiscectomy with or without fusion. J Spinal Disord Tech 2007; 20: 361-368.
- van Eck CF, Regan C, Donaldson WF, Kang JD, Lee JY. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine 2014; 39: 2143-2147.
- Quintana LM. Complications in anterior cervical discectomy and fusion for cervical degenerative disc disease. World Neurosurg 2014; 82: 1058-1059.
- Rosenthal P, Kim KD. Cervical adjacent segment pathology following fusion: Is it due to fusion? World J Orthop 2013; 4: 112-113.
- Wu SK, Kuo LC, Lan HC, Tsai SW, Chen CL, Su FC. The quantitative measurements of the intervertebral angulation and translation during cervical flexion and extension. Eur Spine J 2007; 16: 1435-1444
- Lundine KM, Davis G, Rogers M, Staples M, Quan G. Prevalence of adjacent segment disc degeneration in patients undergoing anterior cervical discectomy andfusion based on pre-operative MRI findings. J Clin Neurosci 2014; 21: 82-85.
- Rihn JA, Lawrence J, Gates C, Harris E, Hilibrand AS. Adjacent segment disease after cervical spine fusion. Instr Course Lect 2009; 58: 747-756.
- Sheth JH, Patankar AP, Shah R. Anterior cervical microdiscectomy: is bone grafting and in-situ fusion with instrumentation required? Br J Neurosurg 2012; 26: 12-15.
- Nandoe Tewarie RD, Bartels RH, Peul WC. Long-term outcome after anterior cervical discectomy without fusion. Eur Spine J 2007; 16: 1411-1416.
- Botelho RV, Dos Santos Buscariolli Y, de Barros Vasconcelos Fernandes Serra MV, Bellini MN, Bernardo WM. The choice of the best surgery after single level anterior cervical spine discectomy: A systematic review. Open Orthop J 2012; 6: 121-128.
- Kim JH, Park JY, Yi S, Kim KH, Kuh SU, Chin DK, Kim KS, Cho YE. Anterior cervical discectomy and fusion alters whole-spine sagittal alignment. Yonsei Med J 2015; 56: 1060-1070.