Case Report - Journal of Gastroenterology and Digestive Diseases (2017) Volume 2, Issue 3
Biliary atresia associated by situs anomalies: 3 case reports.
Ashjaei Bahar*, Mirsharifi Alireza
Department of Pediatric Surgery, Pediatric Center of Excellence, Tehran University of Medical Sciences, Iran
- *Corresponding Author:
- Bahar Ashjaei
Assistant professor Department of Pediatric Surgery Pediatric Center of Excellence Tehran University of Medical Sciences Iran.
Tel: +989123805401, +989213805401, +982166911030
E-mail: ashjaei@tums.ac.ir
Accepted date: December 02, 2017
Citation: Bahar A, Alireza M. Biliary atresia associated by situs anomalies: 3 case reports. J Gastroenterol Dig Dis. 2017;2(3):5-7.
Abstract
Biliary atresia is an obliterative process caused by an unknown pathogenesis. Biliary atresia has an estimated incidence of 1/8000 to 1/20000 reported different sources. Hepatoportoentrostomy (Kasai) has been introduced as a choice of biliary atresia treatment which causes long time survival with a native liver and jaundice free clinical state. Biliary atresia can be the cause of cholestatic jaundice in neonates and infants. It can be due to idiopatic, destructive, viral, inflammatory process, ischemic, toxic and remodeling arrest in extrahepatic and intrahepatic bile ducts. Situs inversus is a rare finding in neonates; however biliary atresia is seen to be associated by situs anomalies. Other congenital and gastrointestinal anomalies like malrotation, duodenal atresia, tracheoesophageal fistula and esophageal atresia, biliary atresia were found in 58% of these patients. Here, we present 3 case reports.
Keywords
Jaundice, Biliary atresia, Hepatic biliary tract.
Introduction
Biliary atresia is an obliterative process caused by an unknown pathogenesis. Biliary atresia has an estimated incidence of 1/8000 to 1/20000 reported different sources [1-3]. Hepatoportoentrostomy (Kasai) has been introduced as a choice of biliary atresia treatment which causes long time survival with a native liver and jaundice free clinical state [3]. Although post operational enteric bile flow is necessary for a Kasai to consider it a success, there are different factors which (…) With regard to this, bile flow restored in our three cases. In 11 to 20% of cases diagnosed by biliary atresia, other congenital anomalies are seen. Biliary atresia is resulted by destructive idiopathic, inflammatory process which is described as a fibrosis and obliteration of intra and extra hepatic biliary tract.
Case 1
A 35-days-old male infant presented with jaundice which was associated with poor feeding and history of 36 weeks of gestational age. Other findings include acholic stool and situs inversus and VSD. Patient was product of a twin pregnancy which the other twin's findings were normal except LBW (1900 g versus 2700 g in patient). In maternal history there was two history of abortion priorly. Lab data showed bilirubin 7.1 (Direct: 3.4), RBC 2.23 million/ml, Hemoglobin 8.5 g/dl, hematocrit 20.9. Also other anomalies such as cystic fibrosis, a1 antitrypsin deficiency was ruled out. Kasai operation was undertook for the patient and post operating findings revealed improvement in jaundice as comes below (Table 1).
| Age | Total Bilirubin (mg/dl) | Direct bilirubin (mg/dl) |
|---|---|---|
| 35 days | 7.1 | 3.4 |
| 45 days (post op.) | 6.9 | 2.8 |
Table 1: Post-operative findings revealed improvement in jaundice.
Case 2
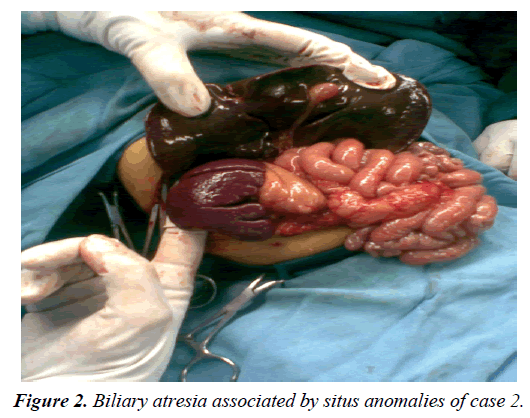
A 70-days-old male infant was referred due to prolonged jaundice since 4th day of birth. In history acholic stool and dark yellow urine was prominent. Baby was a production of caesarean section delivery with a birth weight of 3750 g. In physical exam there was no organomegaly or stigmata of cirrhosis but severe jaundice and hydrocele was notably seen. Frequent serum bilirubin check showed a range of 12 mg/ dl (total bilirubin) and 3.5-6.5 mg/dl (direct bilirubin). Liver enzymes check revealed 3-20 fold of normal range and alkaline phosphatase was revealed as 1773, 2950 and 3088 respectively. PT and PPT was prolonged even with administration of vitamin K. HIDA scan was suggestive for extrahepatic biliary atresia. In addition, abdominal ultra-sonography was reported liver in left, stomach in right, polysplenia and levocardia which is strongly suggestive for situs inversus. Hepatosplenomegaly was reported in ultrasonographic evaluation. Since congenital biliary atresia was established, Kasai operation was planned for the patient. Surgical report revealed enlarged nodular liver was positioned in midline mildly shifted to left, also undeveloped and fibrotic sclerotic gallbladder and extrahepatic biliary duct was seen. Pathology reported evidences of large bile duct obstruction. Further evaluation revealed Hepatitis Activity Index (HAI) stage 6 and grade 4.
Case 3
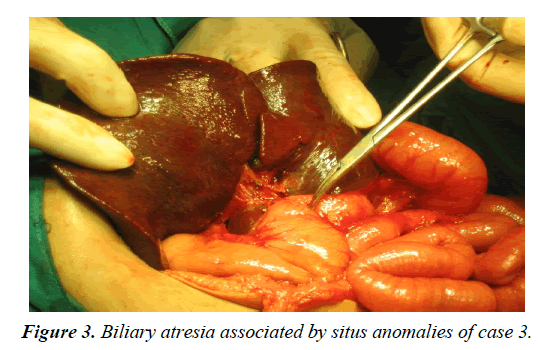
A 60-days-old male infant is presented with jaundice since 3rd day of birth. Acholic stool and dark yellow urine was detected in following day of admission. He was a product of NVD who had good conditions at the beginning of life. Imaging techniques such as chest X-ray and abdominal sonography revealed multiple anomalies in liver spleen and heart. Hepatosplenomegaly was reported in ultrasonographic evaluation. Bilirubin (total and direct) was 9.9 and 4.4 respectively at the admission. A moderate raise in AST, ALT and alkaline phosphatase was obvious. Whereas PT, PTT was in normal range. HIDA scan was suggestive for extrahepatic biliary atresia and left sided liver. Kasai operation was performed and wedge excisional biopsy was done which supported the diagnosis of biliary atresia. Although serum bilirubin level remains above the normal range, It showed significantly decrease as see below.
Discussion
Biliary atresia can be the cause of cholestatic jaundice in neonates and infants. It can be due to idiopatic, destructive, viral, inflammatory process, ischemic, toxic and remodeling arrest in extrahepatic and intrahepatic bile ducts. Cholestatic jaundice can cause fibrosis and cirrhosis in the liver of the affected infant [4-8].
Situs inversus is a rare finding in neonates; however biliary atresia is seen to be associated by situs anomalies. All the professions do accept that the main treatment is hepatoportoenterostomy (Kasai) in this association kasai could be more challenging. What is more, the operation should be performed as soon as possible after diagnosis. Success of treatment is based on native liver survival and necessarily patent biliary flow.
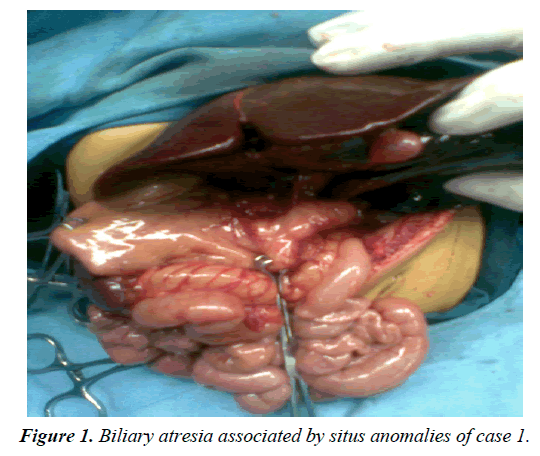
We have two kinds of extrahepatic biliary atresia in children. Non-syndromic extrahepatic biliary atresia is not associated with any other congenital anomalies and presents later than syndromic extrahepatic biliary atresia. Syndromic extrahepatic biliary atresia presents at first week of age and is associated with other congenital anomalies [9]. Jaundice was presented at the first week of age in all of our 3 cases (Figures 1-3).
Conclusion
In a single center, of 28 years retrospective study 10.2% of cases of extrahepatic biliary atresia had congenital splenic anomalies which we found it in all of our 3 cases with the higher rate of prenatal disease in their mothers but we did not find this relation in any of our cases [10].
In one study which was reported from South Korea in 24 years 45 patients with situs inversus were evaluated. Other congenital and gastrointestinal anomalies like malrotation, duodenal atresia, tracheoesophageal fistula and esophageal atresia, biliary atresia were found in 58% of these patients [11].
References
- Ashcraft K, Miyano T, Patrick J, et al. Biliary tract disorders and portal hypertension. Ashcraft's pediatric surgery. 2009:557-67.
- Bahar FAM, Shahmirzadi SM. Embryonal biliary atresia with levocardia and situs inversus: A case report. Iran J Pediatr. 2007:383-87.
- Oldham I. Principles and practice of pediatric surgery. Biliary Atresia. 2005:1457- 490.
- Balistreri WF, Grand R, Suchy FJ, et al. Biliary atresia: Current concepts and research directions. Hepatol. 1996;23(6):1682-92.
- Yoon PW, Bresee JS, Olney RS, et al. Epidemiology of biliary atresia: A population based study. Pediatr. 1997;99(3):376-82.
- Schreiber RA, Leinman REK. Genetics, immunology, and biliary atresia: An opening or a diversion? J Pediatr Gastroenterol Nutr. 1993;16:111-3.
- Klippel CH. A new theory of biliary atresia. J Pediatr Surg. 1972;7:651-4.
- Balistreri WF. Schiff's disease of the liver. Lippincott–Raven Press, Philadelphia, USA. 1999:1357-512.
- Schreiber RA, Kleinman RE. Biliary atresia. J Pediatr Gastroenterol Nutr. 2002;35:S11-6.
- Davenport M, Tizzard SA, Underhill J, et al. The biliary atresia splenic malformation syndrome: A 28-year single-center retrospective study. J Pediatr. 2006;149:393-400.
- Lee SE, Kim HY, Jung SE, et al. Situs anomalies and gastrointestinal abnormalities. J Pediatr Surg. 2006;41:1237-42.