- Biomedical Research (2013) Volume 24, Issue 3
Bacterial tonsillar microbiota and antibiogram in recurrent tonsillitis.
Babaiwa U.F.1*, Onyeagwara N.C.2, Akerele J.O.1
1Department of Pharmaceutical Microbiology, Faculty of Pharmacy, University of Benin, Benin City .Nigeria.
2Department of Surgery, School of Medicine University of Benin, Benin City, Nigeria.
- *Corresponding Author:
- Babaiwa U.F
Department of Pharmaceutical Microbiology
Faculty of Pharmacy, University of Benin
Benin City, Nigeria.
Accepted date: December 27 2012
Citation: Babaiwa UF, Onyeagwara NC. Akerele JO. Bacterial tonsillar microbiota and antibiogram in recurrent tonsillitis. Biomedical Research 2013; 24 (3): 298-302.
Abstract
The study of bacterial flora implicated in patients with recurrent tonsillitis in a Teaching, Tertiary Institution was carried out; to identify the main organisms responsible for tonsillitis, their sensitivity and resistance to antibiotics. At tonsillectomy,swabs of Surface and core tonsillar materials were taken and cultured, bacteria isolated were identified and their antibiogram determined using standard laboratory techniques. The most frequently isolated organisms were Staphylococus aureus (70%) which was found to be the principal causative agent across all ages. Streptococus pyogenes and Psuedomonas aeruginosa accounted for 14% and 2% respectively and were most frequently isolated in children from 0-6years.This study demonstrated a marked difference between surface and deep core microflora of the tonsil in 20 patients, while in 40 patients there were no significant difference. All bacterial isolates were resistant to amoxicillin, amoxicillin /clavulanic acid and erythromycin to different degrees. Ciprofloxacin, gentamicin and cotrimoxazole; were moderately effective against the aetiologic tonsilar agents. Continuous surveillance on antimicrobial susceptibility of tonsillar materials is essential for detection of emerging trends and use of appropriate therapeutic interventions.
Keywords
Tonsilitis, antibiotics, antibiogram, Streptococus pyogenes and Psuedomonas aeruginosa
Introduction
The tonsils are two tissue balls located at the back of the throat, usually associated with the control of infections in humans; they are susceptible to infection by: viruses, bacteria, Chlamydia and fungi; a condition known as tonsillitis [1].
Acute tonsillitis is one of the most common manifestations of the upper respiratory tract infections. It is common in children and considered to be the third most frequently diagnosed disease in paediatric medicine. The highest incidence occurs between 4-5years; while school children between the ages of 6 and 12years are highly predisposed. Its occurrence in elderly has been described as unusual [2].
Most patients who present with symptoms of acute tonsillitis experience only a limited disease course, a substantial portion of them receive pharmacologic treatment .The treatment of choice is Penicillin .Other antibiotics used in treatment, are amoxicillin, amoxicillin-clavulanic acid, macrolides, clindamycin or cephalosporines [3]. Research shown that antibiotics are prescribed for approximately three quarter of patients with tonsillitis in the United States of America( USA) [4].
The prophylactic use of these drugs has not fully prevented and eradicated bacterial invasion, recrudesces occur requiring tonsillectomy, a procedure performed on approximately 800,000 patients annually [5-7].
Increasing data from reports suggest that bacteria, other than Beta haemolytic Streptococci may cause tonsillitis [8,9].
The microorganisms that cause this infection are undergoing constant changes with respect to their isolation and bio physiological features. Typically, patients who undergo tonsillectomy by way of intervention have been treated with multiple courses of antibiotics that failed to eradicate the infection completely or have had multiple recurrences of a presumed ‘new’ infection.
As part of the efforts to unravel the causes of these treatment failure and frequent recrudesces this study is designed to identify the etiologic bacteria from tonsillar tissues of patients that have undergone tonsillectomy, following recurrent tonsillitis and determine their antibiogram.
Method
Study design.
This was a prospective study of consecutive patients undergoing tonsillectomy for recurrent tonsillitis at the University of Benin Teaching Hospital (UBTH) Benin City, Nigeria. Approval for this study was obtained from UBTH Institutional ethical review board and verbal informed consent was obtained from all patients after being briefed about the study.
Study sample
All patients who presented to otolaryngology Department from August 2010-December 2011, for tonsillectomy following recurrent tonsillitis were included. All patients who came for tonsillectomy due to obstructive (not infectious), reasons were excluded. Seventy five patients including forty males and thirty five females with recurrent tonsillitis were used. Their ages range from 2-46years, mean age was 6years.
Specimen collection and analysis
All specimens were collected at the time of surgery .After the induction of anaesthesia independent sterile swab sticks were rubbed vigorously on the right and left tonsillar surface of each patient to obtain culture specimen. Immediately after the tonsillectomy independent sterile swabs sticks were rubbed on the interior of the right and left tonsils to obtain the tonsillar deep culture. A total of 300 swabs from 75 patients were collected and immediately streaked onto different agar plates (blood agar, chocolate agar and Mac Conkey agar). The plates were observed for culture growth after 24hours of aerobic incubation. Susceptibility test of the isolates was carried out with agar diffusion assay according to the modified Kirby Bauer method [10]. The antibiotics used were selected based on the current first line drugs in the guideline of antibiotics usage in the study area.
The diameter of zones of inhibition obtained, were interpreted using the CLS I standard [11].
Results
The 75 patients enrolled in the study included 40 males and 35 females; mean age of 6years; age range 2- 46years. Fifty (50) patients were being treated with amoxicillin clavulanic acid, 10 patients with erythromycin antibiotics prior to admission. 15 patients had no antibiotics prior to admission. The recorded duration of symptoms was between 1-8years.
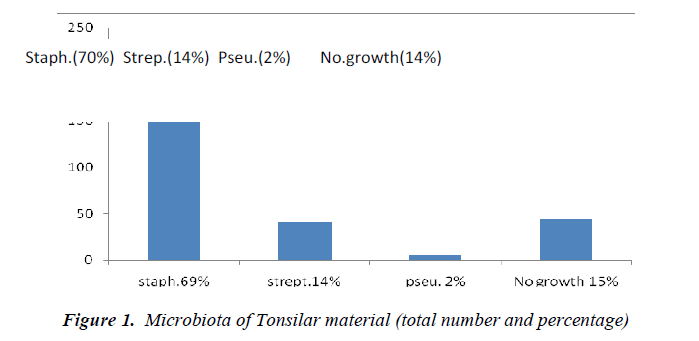
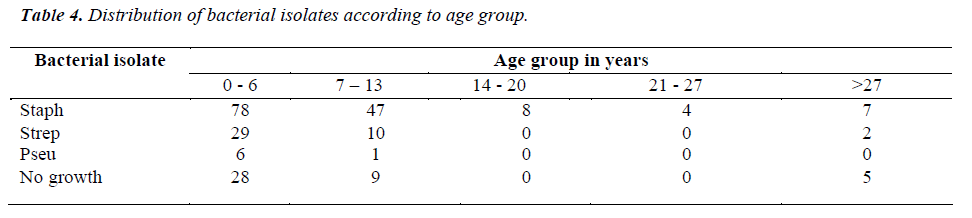
The most commonly isolated microorganisms (Figure 1) were Staphylococcus aureus (70%) Streptococcus pyogenes (14%) and Pseudomonas aeruginosa (2%). A total of 42 (14% ) cultured specimen showed no growth. This study demonstrated a marked difference between the surface and the deep-seated microflora in 20 patients. However, deep and surface culture isolates were found to be identical in 40 patients. In 6 patients the result of their right and left deep core tonsillar materials showed no growth. There was no growth from the tonsilar material obtained from six of the patients.
Discussion
This study has shown the aerobic bacteria in tonsillar tissues of patients who presented for tonsillectomy in a Teaching hospital and their antibacterial susceptibility pattern. Staphylococcus aureus was found to be the principal causative agent of tonsillitis in all age groups from this study. We found in this study a high incidence of Staphylococcus aureus (70%),as against Streptococcus pyogenes (14%),which were the traditional and often encountered etiologic agent in tonsillar infection. Our data are similar to some earlier reports where Staphylococcus aureus was the most frequently isolated organisms accounting for 29.3% followed by Streptococcus pyogenes 23.4% [12,13]. The microorganisms most frequently isolated among patients (0-6years) were Pseudomonas aeruginosa (100%) and Streptococus pyogenes (29%).
In 20 patients, there was significant difference in bacterial isolates obtained from the tonsillar core (where most of the sites were colonised with more than one organism) compared with that on the surface that were seldomly colonised by more than one organism. This is in line with previous studies where pathogenic microorganisms from the interior of the tonsil were different compared with surface bacteria in 48 patients [14]. rface and core isolates were however, found to be similar in 40 patients; contrary to previous studies.
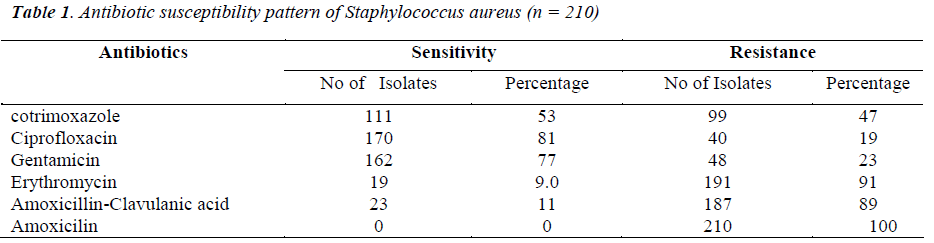
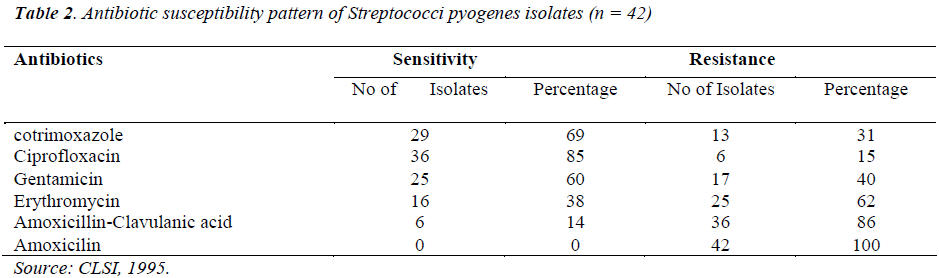
The susceptibility of the three principal microorganisms isolated showed that 81% of Staphylococus aureus was susceptible to ciprofloxacin,77% to gentamicin, but were conspicuously resistant to amoxicillin and amoxicillin – clavulanic acid combination;these are drugs that have been routinely used in the management of recurrent tonsillitis in this environment. This observation is similar to that obtained by previous studies; where Staphylococus aureus had sensitivity of 88%, 73% to ciprofloxacin and gentamicin respectively [15]. It was also observed that Streptococus pyogenes was sensitive to ciprofloxacin (85%), cotrimoxazole 69%),gentamicin (60%) and moderately sensitive to erythromycin (38%), but resistant to amoxicillin and its combination with clavulanic acid (Table 11). is is contrary to previous studies, where a sensitivity of close to 100% was recorded for amoxicillin .The observed resistance of Staphylococcus aureus and Streptococuss species to erythromycin could be partly explained by the fact that erythromycin was used as an alternative treatment of choice for infection caused by these agents in patients with hypersensitivity to penicillin [16].
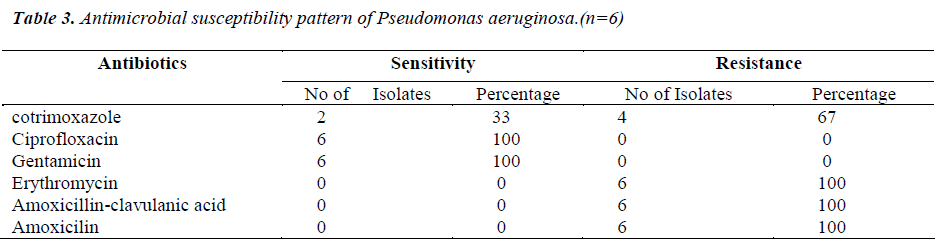
The susceptibility profile showed that ciprofloxacin and gentamicin should be the treatment of choice for the recurrent tonsillitis in this area of study,as previously observed by workers where Pseudomonas aeruginosa and other aetiologic agents were highly sensitive to gentamicin and ciprofloxacin [17]. The use of ciprofloxacin in children should be seldom encouraged since this is contraindicated in such group of patients. The use of amoxicillin or amoxicillin –clavulanic acid combination as first choice drugs in recurrent tonsillitis should be discouraged as our data have shown increasing resistance of the aetiologic agents in recurrent tonsiltitis in our setting. Our study has shown the imperative of continuous surveillance of antimicrobial susceptibility generally and in particular of tonsillar materials for early detection of emerging resistance trends and adjustment and usage of appropriate therapeutic interventions. Efforts would be made to evaluate possible anaerobic infectious agents associated with tonsilar materials in our future investigations. The possible role of fungi and viruses was not within the purview of this study.
References
- Eltonjohn24.Freechilddevelopment.com 2011.
- Piedrola DM,Montiel NQ,Lopez IR, et al.Present situation of antibiotic resistances in tonsillar infections. Acta Otorrinolaringol Esp 2006; 57: 171-175.
- Gaffney RJ, Cafferrkey MT. acteriology of normal and deseased tonsils assessed by fine-needle aspiration:Haemophilus inflenzae and the pathogenesis of recurrent acute tonsillitis.Clin Otolaryngol 1998; 23: 181-185.
- Richelle JC, Jerome RH, John GB, et al. Principle of appropriate antibiotic use for acute pharygnitis in Adults. Ann Intern Med 2001; 134: 6509-6517
- Garcia de Lomas J, Gimeno C, Diez J, et al. Garcia – Ponte Ly Grupo Espanol parael Estudio de la Sensibilidad a Macrolidos en la Atencion Primaria.Sensibilidad a eritromicina y claritromicina de aislados de Streptococcus beta-hemoliticos de grupo A productores de faringoamigdalitis en la edad pediatrica:studio multicentrico en la Atencion Primaria.Enferm Infecc Microbiol Clin 1999; 17: 24-28.
- Gene A, Gonzalez-Cuevas A,Juncosa T, et al. ensibilidad antibiotica de Streptococcus pyogenes en pediatria. Eferm Infec Microbiol Clin1998; 16: 272-274.
- Bisno AL. Pharyngitis.En Principle and Practice of Infectious Disease, de Mandell GL,Bennett JE, Dolin R.Elsevier/Churchill Livingstone. 6th Ed. 2005: 752-758.
- Paradise JL. Etiology diagnosis and antimicrobial treatment of Pharyngitis and pharyngotonsillitis.Ann Otolrhinol Laryngol.1981; 90 (suppl 84): 75-78.
- Brook I.Tonsillitis,in Brook I (ed):Anaerobic Infection in Childhood, Boston, GK Hall, 1983, pp 156-175.
- Bauer AW, Kirby WM. Antibiotic susceptibility testing by standardized single disk method. Am J Clin Pathol 1966; 45: 493-496.
- National committee for clinical laboratory standards (now CLSI).Performance standard for antimicrobial disk susceptibility Test.NCCLS document M2-A8.Wayne. Pa: National committee for clinical laboratory standard.2003.
- Kocaturk S,Demiray T,Incesulu A. et al.Comparison of adenoid and tonsil core ultures in hronic adenotonsillitis. Kulak Burun Bogaz Ihtis Derg 2003; 10: 105-109.
- Mitchelmore IJ, Reilly PG, Hay AJ, et al. Tonsil surface and core cultures in recurrent tonsillitis:prevalence of anaerobes and beta-lactamase producing organisms.Eur J Clin Microbiol Infect Dis 1994; 13:542-548. Recurrent tonsillitis. The Journal of Laryngology and Otology 2007; 91: 911-913.
- Rosen G. Samuel J. Vered I. Surface tonsillar microflora versus deep tonsillar microflora in recurrent tonsillitis. The Journal of Laryngology and Otology. 2007; 91: 911-913.
- Omololu-Aso J, Kolawole DO, Omololu OO et al. Antibiotics sensitivity pattern of Staphylococcus aureus from fomites in the Obafemi Awolowo University Teaching Hospital Complex (OAUTHC) Nigeria. International Journal of Medical Sciences. 2011; 3(2): 32-36.
- Low DE. Antimicrobial drug use and resistance among respiratory pathogens in the community. Clin Infect Dis.2001; 33(suppl.3):206-213.
- Adedeji GB, Fagade OE, Oyelade AA. Prevalence of Pseudomonas aeruginosa in clinical samples and its sensitivity to citrus extract.African Journal of Biomedical Research 2007; 10 (2): 183-187.