Research Article - Biomedical Research (2017) Volume 28, Issue 8
Axillary reverse mapping in breast cancer with enlarged lymph node
Wen-ju Mo, Xi-ping Zhang*, En-qi Qiao, Shang-nao Xie and Xiao-wen Ding*Department of Breast Surgery, Zhejiang Cancer Hospital, Hangzhou, Zhejiang Province, PR China
- *Corresponding Authors:
- Xiao-wen Ding
Department of Breast Surgery
Zhejiang Cancer Hospital
PR China - Xi-ping Zhang
Department of Breast Surgery
Zhejiang Cancer Hospital
PR China
Accepted date: December 30, 2016
Abstract
Objective: The research is to explore the success rate and safety of axillary reverse mapping (ARM) and the effect on the function and lymphedema of ipsilateral upper limb, and to investigate the quality-of-life of patients with breast cancer after operation, as well as to explore the related factors affecting the success rate of ARM.
Methods: In operation of 60 cases of female patients with enlarged axillary lymph nodes in breast cancer, both the ARM-nodes and the crossover stained lymph nodes with Methylthioniniun Chloride Injection and Nano Carbon Injection were performed the intraoperative frozen section examination. We investigated the ipsilateral limb function and quality-of-life of patients between the ARM success group and ARM failure group.
Results: The BMI and degree of upper limb lymphedema in ARM success group were significantly lower than in the ARM failure group (P<0.05). Multivariate analysis showed whether success of ARM was the independent risk factor of ipsilateral upper limb lymphedema (P<0.05).
Conclusion: The ARM technique can reduce the occurrence of ipsilateral upper limb edema, and can improve upper limb function as well as the quality-of-life. ARM is an independent risk factor for upper limb lymphedema after axillary lymph node dissection (ALND).
Keywords
Breast cancer, Axillary Reverse Mapping (ARM), Entirely lymph node imaging, Lymphedema
Introduction
Breast cancer is one of the most common tumors for women all over the world and a cause of 20% women’s deaths annually [1]. It was reported that in 2015, patents who were diagnosed to have breast cancer increased by over 230,000 in the United States. According to statistics, the incidence of breast cancer is similar between developed and underdeveloped countries [2]. In recent years, the identification rate of breast cancer is obviously increased with the promotion of breast cancer census and continuous improvement of early diagnosis technology, the majority of patients can obtain long-term survival after reasonable treatment.
Therefore, the prognosis of breast cancer is improved significantly. How to improve the quality-of-life of patients during improved prognosis has become the important question Surgery is an important way to treat breast cancer, however, after surgery, the lymphedema of ipsilateral upper limb has always been a common complication, greatly and seriously influenced the quality-of-life of patients [3,4]. Although the complications have significantly decreased over time with improvement of surgical techniques or methods, but the phenomenon of lymphedema still can’t be completely avoided.
The concept of axillary reverse mapping (ARM) [5,6] put forward in recent years is to mark the lymph ducts and lymph nodes of ipsilateral upper limb with different dyes. We should reserve these lymph ducts and lymph nodes when axillary lymph node dissection (ALND) or sentinel lymph node biopsy (SLNB) are underwent, the ARM technique can protect the ipsilateral limb’s lymphatic backflow, and reduce lymphedema incidence of ipsilateral upper limb after surgery of breast cancer. ARM is a new concept and technology and is considered to be a revolutionary surgical technique. ARM is a technique by which the lymphatic drainage of the upper extremity that traverses the axillary region can be differentiated from the lymphatic drainage of the breast during axillary lymph node dissection (ALND). Beek et al. have reviewed the current literatures on the ARM procedure and discussed the feasibility, safety and relevance of this technique. They think that preservation of ARM lymph nodes and corresponding lymphatics was proven to be oncologically safe in clinically node-negative breast cancer patients with metastatic lymph node involvement in the sentinel lymph node (SLN) who are advised to undergo a completion axillary lymph node dissection (ALND). The ARM procedure is technically feasible with a high visualisation rate using blue dye or fluorescence. ALND combined with ARM can be regarded as a promising surgical refinement in order to reduce the incidence of upper extremity lymphedema in selected groups of patients [7]. A Meta-Analysis, published in PLoS One by authors Han et al. which proposed that the ARM procedure was feasible during ALND. Nevertheless, it was restricted by low identification rate of ARM nodes during SLNB. ARM was beneficial for preventing lymphedema. However, this technique should be performed with caution given the possibility of crossover SLN-ARM nodes and metastatic ARM nodes. ARM appeared to be unsuitable for patients with clinically positive breast cancer due to oncological safety concern [8].
At present, the most controversial issues of the technique are that, whether it is safe to protect ARM-nodes (or vessels), whether will affect the curative effect of breast cancer and whether it really can reduce ipsilateral limb’s lymphedema to achieve the purpose of protect limb’s function. Now, the previous studies can’t answer this question well. Therefore, we collected 60 patients of having invasive breast cancer with axillary lymph node enlargement during clinical examination, and use two different colors’ tracer dyes at the same time in the operation. Preoperative lymphoscintigraphy by Nano Carbon Injection was injected into the ipsilateral areola region by clockwise markering and intraoperative lymphoscintigraphy by Methylthioniniun Chloride Injection were injected into the subcutaneous and intramuscular of the ipsilateral upper-inner limb by reverse markering (named axillary reverse mapping, ARM). To explore the feasibility and safety of ARM, as well as the influence of ARM to upper limb lymphedema and the quality-of-life of breast cancer patient after surgery.
Materials and Methods
General information
Selected 60 female patients from our hospital between Aug 2010 and Aug 2013, who had been diagnosed as invasive breast cancer and intended to carry out ALND surgery, preoperative examination detected that all those patients had allillary lymph node enlargement of ipsilateral side (physical examination or B ultrasound examination), TNM clinical stage T1-3N1M0, they had not been radiotherapy and chemotherapy before surgery, with average age of 51.34 ± 10.65 years old (the youngest is 30 and the oldest is 65), the median age is 51 (Table 1). The average body mass index (BMI) is 23.97 ± 2.67, the minimum BMI is 18.91, the maximum BMI is 29.75 and the median BMI is 23.69. The medical ethical committee of our hospital approved the investigation of using ARM for breast cancer patients. All patients received information regarding the entire procedure. Before surgery, all patients signed to agree for ARM and some related investigation, they were underwent relevant subsequent treatments according to NCCN guideline for breast cancer standardized treatment. Nano Carbon Injection (25 mg/each bottle) was purchased from Lummy pharmaceutical Limited company (Chongqing, China). Methylthioniniun Chloride Injection (2 ml/each bottle) were purchased from Yongkang Pharmaceutical Co., Ltd (Beijing, China).
| Characteristic | n=60 |
|---|---|
| Age (years) | 51.34 ± 10.65 |
| BMI(kg/m2) | 23.97 ± 2.67 |
| pT stage | |
| T1 | 39 |
| T2 | 19 |
| T3 | 2 |
| pN stage | |
| 0 | 38 |
| 1 | 17 |
| 2 | 5 |
| 3 | 0 |
| Estrogen receptor | |
| Positive | 26 |
| Negative | 34 |
| Progesterone receptor | |
| Positive | 25 |
| Negative | 35 |
| Her-2 neu receptor | |
| Positive | 17 |
| Negative | 35 |
| Unknown | 8 |
| Vessel violation | |
| Yes | 21 |
| No | 39 |
| Multifocal | |
| Yes | 2 |
| No | 58 |
| Histological type and grading | |
| Invasive ductal cancer. Grade 1 | 9 |
| Invasive ductal cancer. Grade 2 | 30 |
| Invasive ductal cancer. Grade 3 | 8 |
| Other types | 13 |
Table 1: The clinical and pathological features.
Surgery methods
Based on the methods of references before surgery [9], injected Nano Carbon Injection (a kind of black dye) in ipsilateral areola skin and subcutaneous (clockwise markering lymph ducts and lymph nodes, entirely lymph node imaging, the tracer is black), during surgery, separated the skin flap of the breast to show the axilla, injected a kind of blue dye (Methylthioniniun Chloride Injection) about 2 ml in inside skin of ipsilateral upper-inner limb. subcutaneous and muscle (ARM), then raised the upper limb to increase lymph backflow, after that, continued to dissect the axilla and carefully searched, the lymph ducts and lymph nodes with blue stained should be reserved as far as possible, the lymph nodes with blue stained (ARM-nodes) should be removed and marked separately to do pathological examination. At the same time, dissected clockwise markering lymph nodes (including I, II stage lymph nodes), dissected together if they were crossover or suspicious appearance, marked and then send to do pathological examination; ARM will succeed if finds blue stained lymph ducts or lymph nodes during surgery. ARM will fail if not clearly identifies blue stained lymph ducts or lymph node, and then carry out axillary I, II stage lymph node dissection.
Measurement method of lymphedema in ipsilateral upper limb
According to the international most often adopted method of measuring limb cross section diameter’s change, that is, by a tape to measure ipsilateral wrist’s transverse striation, forearm, elbow transverse striation, upper limb and shoulder’s cross section diameter, take maximum value of difference in same position of bilateral upper limb, and then to evaluate edema degree.
Measure upper limb’s activity function
Compared to contralateral limb, by upper limb function measuring tray to measure ipsilateral upper limb’s bending, stretching, adduction, abduction, inward and outward turning functions, recorded one time every 3 months, taking an average value of the 4 times recorded value.
Survey of life quality
Evaluated life quality according to simplified Chinese version FACT-B [10,11], once time every 3 months, taking an average value of the 4 times recorded value.
Statistical analysis
Respectively carried out test of normality to age, BMI and the difference of bilateral upper limb section diameter to verify that they consistent with normal distribution; by two sample t test to respectively analyzed the relationship of age, BMI, difference of bilateral limbs’ cross section diameter, activity function and life quality of ARM success and failure two groups; Used Logistic regression, eliminated age, BIM and other possible confounding factors, and then analyzed the influence of success and failure of ARM to difference of bilateral limbs’ cross section diameter. There was statistical difference as P<0.05.
Results
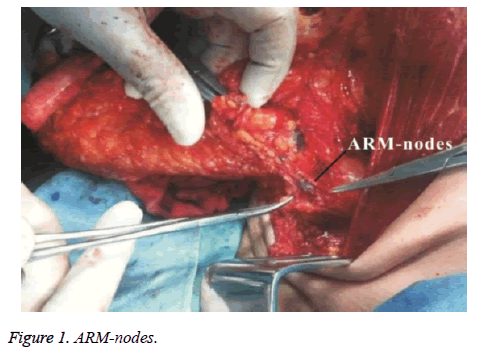
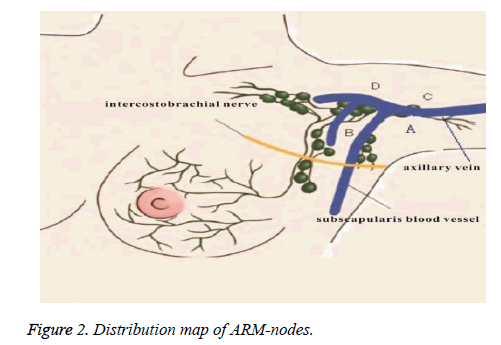
In 60 patients, there were 38 patients with successful ARM, accounting for 63.3%, and 17 patients with failed ARM, accounting for 28.3%, take about 5-10 minutes for testing ARM-nodes or lymph ducts. In 38 patients with successful ARM, 27 patients were detected blue stained lymph nodes (ARM-nodes, Figure 1), the majority of patients owned one node, and small number of patients owned 2-3 nodes, with an average of 1.12 ± 0.78, total of 31 ARM-nodes. Routine pathological examination showed that one ARM-nodes had isolated cancer nest and the remaining ARM-nodes were negative (Table 2); Most ARM-nodes were located in angle area 2 cm away of axillary vein and subscapular artery outside (Figure 2: A Area), and small part was located in axillary vein top level or the area near to head vein into axillary vein (Figure 2: C, D areas).
| Position of ARM-nodes | Case number (%) | The number of metastatic lymph node (%) |
|---|---|---|
| Region A | 70.3 (19/27) | 3.7 (1/27, isolated cancel nest) |
| Region C | 22.2 (6/27) | 0 |
| Region D | 7.4 (2/27) | 0 |
Table 2: Position and metastatic proportion of ARM-nodes.
The remaining 11 patients were detected blue stained lymph nodes only and not detected blue stained lymph nodes. The other 5 patients (5/60, 8.3%) were respectively detected one lymph node with crossover dying or the dying was indistinct, pathological examination detected that 2 nodes were lymph node metastatic carcinoma, and the remaining 3 lymph nodes were negative. The most of lymph nodes with crossover dying or suspicious appearance were located in the side of lateral thoracic vessels and outside of subscapular artery (Figure 2: A, B Areas).
Carried out normality test to age, BMI and the difference of bilateral limbs’ cross section diameter of 52 patients with successful or failed ARM (2 patients were lost to follow-up among 38 patients with successful ARM, and 1 patient was lost to follow-up among 17 patients with failed ARM), P average was >0.05 to verify that they consistent with normal distribution. The two sample t test found that both BIM and bilateral limbs’ cross section diameter of ARM success group were lower than that of failure group, P<0.05, had statistical difference, the age of two groups had no difference, P>0.05 (Table 3).
| Indexes | ARM | Case number | Mean | Standard deviation | t | P |
|---|---|---|---|---|---|---|
| BMI | Failure | 16 | 25.35 | 2.38 | 2.66 | 0.01 |
| Success | 36 | 23.31 | 2.58 | |||
| Circumference Difference of Bilateral Upper Limb | Failure | 16 | 1.73 | 0.62 | 4.18 | 0.01 |
| Success | 36 | 1.12 | 0.4 | |||
| Age (years) | Failure | 16 | 52.62 | 10.39 | 0.58 | 0.56 |
| Success | 36 | 50.74 | 10.88 |
Table 3: Analysis of influence factors of different ARM conditions.
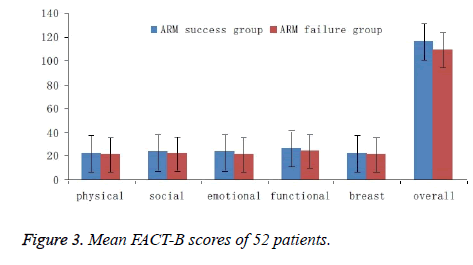
Used Logistic regression, eliminated BIM, age and other confounding factors and found that ARM success or not was independent risk factor of ipsilateral upper limb lymphedema, P=0.02, OR value=6.39. What means that the risk degree of upper limb lymphedema after undergoing out ALND when ARM fails is 6.4 times of undergoing out ALND when ARM succeeds. There was no significant statistical difference between two groups of patient in the quality-of-life and ARM success group only had slight superiority. In upper limb activity function, ARM success group’s results were close to statistical significance only in abduction (P=0.062) and outward turning (P=0.083), and the remaining aspects had no significant difference (Figure 3 and Table 4).
| Angles of activity limitation | ARM Success group | ARM Failure group | P |
|---|---|---|---|
| Bend | 8.9 ± 10.4 | 9.0 ± 10.8 | 0.892 |
| Stretch | 6.4 ± 7.9 | 7.1 ± 8.3 | 0.532 |
| Adduction | 4.1+6.5 | 3.4 ± 4.9 | 0.153 |
| Abduction | 11.0 ± 17.1 | 14.1 ± 19.2 | 0.062 |
| Internal rotation | 4.6 ± 9.0 | 5.2 ± 7.3 | 0.164 |
| External rotation | 2.7 ± 10.4 | 3.6 ± 8.7 | 0.083 |
Table 4: Changes of activities and functions in 52 patients after ARM operation.
Discussion
ALND is main reason of causing upper limb lymphedema, sensory disturbance and movement dysfunction complications of breast cancer after surgery. Although SLNB is gradually becoming standard treatment of early breast cancer with the improvement of awareness, avoid part of patients be underwent out ALND and bring life quality improvement after surgery, but multiple clinical studies show that, the upper limb lymphedema and dysfunction also can’t be completely avoided even only undergo out SLNB [12-14]. Besides, ALND is an important part of breast cancer surgery and still has extensive surgical indications in the hospitals without SLNB experience and breast cancer patients with positive SLNB. It is particularly important to how to reduce postoperative complications, including lymphedema of ipsilateral upper limb, and improve patient’s life quality at the time of getting accurate axillary lymph nodes information. The proposal of ARM theory is possible to partially solve the problem.
ARM is to map upper limb’s lymph ducts and lymph nodes, and reserves these lymph ducts and lymph nodes in ALND, but the premise of this method is that the reserved lymph ducts and nodes (ARM-nodes) have no metastatic cancer cell, what makes the technology have most controversy [14-17]. Asian scholar Han [18] and other scholars studied and thought that, it is safe and feasible to reserve ARM-nodes in ALND unless the clinical N stage is higher. Gobardhan et al. [19] studied to find that ARM-nodes metastatic rate of patient with metastatic lymph node in axilla also increased obviously. So, it is still necessary to do further study to ARM surgery’s operability and safety. Therefore, we designed to carry out clockwise markering lymph nodes by Nano Carbon before surgery for 60 breast cancer patients with axillary lymph node enlargement, during surgery, injected Methylthioniniun Chloride Injection in upper-inner limb subcutaneous and muscle, and reverse mapping to lymph ducts and node of backflow to axilla from upper limb. During surgery, dissected clockwise markering imaging lymph node as far as possible, tried to protect reverse imaging lymph ducts, the reverse imaging lymph nodes were separately send to do examination, in addition, separately send the lymph nodes (breast and upper limb’s unobstructed lymph nodes) with crossover dying or suspicious appearance to do pathologic examination. On the one hand, ensure to more thoroughly dissect the lymph nodes from breast to axilla; on the other hand, can better study the possibility of ARM-nodes involved by tumor; finally, clockwise markering combined with reverse mapping can do special study to breast and upper limb’s unobstructed lymph nodes. The results showed that ARM success rate was 63.3% and similar with literature [20,21], what means that ARM technology is feasible. In 31 ARM-nodes of 27 patients with successful ARM, only one ARM-nodes was detected isolated cancel nest (the patient’s pathology report after surgery showed that the lymph node state was N2), what shows that it is safe basically to reserve ARM-nodes or lymph ducts in early breast cancer. On the other hand, our study showed that in 5 breast and upper limb’s lymph nodes (unobstructed lymph nodes) with crossover dying, 2 nodes were lymph node metastatic carcinoma (the postoperative pathologic stage is N1 and N2 respectively), in view of the possibility of unobstructed lymph nodes tumor involving was larger (especially with higher N stage), the reservation to breast and upper limb’s unobstructed lymph nodes needs a cautious attitude.
Compared with weight measurement, it was a more objective and generally accepted method through measuring patient’s BMI to reflect the degree of obesity. The results showed that, the BMI value of ARM success group was higher than that of ARM failure group, the difference had statistical significance. The reason may be that obese patient’s axillary fat tissue is rich, lymph ducts is abundant, diameter is smaller and position is hidden, besides, the coarse fat particles and lymph nodes are mixed and relatively difficult to identify and reserve. Conversely, for the patient with thin body, the lymph ducts are small relatively, the diameter is coarse relatively, location is shallow and lymph node is obvious, relatively easy to be developed and found. Therefore, ARM success rate of obese patient is lower.
At present, there is no a unified standard for the definition of upper limb lymphedema, this paper uses a relatively common method, namely, measure unified place of bilateral limbs and take difference, the greater of difference, the more obvious of edema. The study found that the upper limb’s lymphedema degree of patients with successful ARM and reserved upper limb’s backflow lymph ducts were lighter than those of the patients with failed ARM. Use Logistic regression, eliminated the influence of age and BIM confounding factors, to find that ARM success or not is independent risk factor of ipsilateral upper limb lymphedema, P=0.02, OR value=6.39. What means that the risk degree of upper limb lymphedema after surgery of undergoing out ALND after ARM failure was 6.4 times of ALND of reserving ARM-nodes. Boneti et al. [22] studied to authenticate that, the reservation of ARM lymph nodes can safely and effectively reduce incidence of upper limb lymphedema, however, based on the need of study, we didn’t reserve ARM lymph nodes but only reserved lymphatic vessels, what can be expected that, the reservation of ARM lymph nodes can effectively reduce incidence and degree of upper limb edema.
Our study carried out follow-up investigation to patient’s upper limb function and the quality-of-life, and the results showed that there was no significant statistical difference between two groups of patients in the quality-of-life, ARM success group only slightly showed the superiority. In upper limb’s activity function, except ARM success group’s results in abduction and outward turning were similar to statistical significance, the other aspects had no significant differences. The reasons may be: firstly, the case number was too little; secondly, the following-up time was not enough; thirdly maybe that ARM success group reserves upper limb lymph ducts but not reserves ARM-nodes because need to study the possibility of ARM-nodes involved by tumor. But even so, ARM success group also showed the trend of improving upper limb’s activity function and the quality-of-life in some degree.
In a word, it is safe and feasible basically to develop ARM for early breast cancer patients, it is expected to reduce upper limb lymphedema, improve ipsilateral limb function and the qualityof- life. The method is simple to operation, only needs about 5-10 minutes on average and easy to be mastered, its limitations are that ARM success rate may be greatly different based on different cognition and proficiency of different surgeons. ARM development still needs high-quality doctors to strictly grasp ARM indications [19].
Ethic Approval
The ethics committee approved our hospital for the study reported. Before surgery, all patients signed to agree for ARM and some related investigation.
References
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013; 63: 11-30.
- Reis-Filho JS, Milanezi F, Steele D, Savage K, Simpson PT. Metaplastic breast carcinomas are basal-like tumours. Histopathology 2006; 49: 10-21.
- Ronka R, von Smitten K, Tasmuth T, Leidenius M. One-year morbidity after sentinel node biopsy and breast surgery. Breast 2005; 14: 28-36.
- Leidenius M, Leivonen M, Vironen J, von Smitten K. The consequences of long-time arm morbidity in node-negative breast cancer patients with sentinel node biopsy or axillary clearance. J Surg Oncol 2005; 92: 23-31.
- Thompson M, Korourian S, Henry-Tillman R, Adkins L, Mumford S. Axillary reverse mapping (ARM): a new concept to identify and enhance lymphatic preservation. Ann Surg Oncol 2007; 14: 1890-1895.
- Noguchi M. Axillary reverse mapping for breast cancer. Breast Cancer Res Treat 2010; 119: 529-535.
- Beek MA, Gobardhan PD, Schoenmaeckers EJ, Klompenhouwer EG, Rutten HJ, Voogd AC, Luiten EJ. Axillary reverse mapping in axillary surgery for breast cancer: an update of the current status. Breast Cancer Res Treat 2016; 158: 421-432.
- Han C, Yang B, Zuo WS, Zheng G, Yang L, Zheng MZ. The Feasibility and Oncological Safety of Axillary Reverse Mapping in Patients with Breast Cancer: A Systematic Review and Meta-Analysis of Prospective Studies. PLoS One 2016; 11: e0150285.
- Nos C, Lesieur B, Clough KB, Lecuru F. Blue dye injection in the arm in order to conserve the lymphatic drainage of the arm in breast cancer patients requiring an axillary dissection. Ann Surg Oncol 2007; 14: 2490-2496.
- Gao YQ, Fang Y, Yang X, Wang J. Quality-of-life among Chinese women with breast cancer after modified radical mastectomy and immediate breast reconstruction: A comparative study. Chin J Clin Oncol 2014; 41: 729-733.
- Xiao H, Feng T, Duan YL. Effect of different rehabilitation exercise on quality-of-life and upper limb function in elderly patients with breast cancer after operation. Chin J Geront 2013; 33: 5535-5537.
- Wilke LG, McCall LM, Posther KE, Whitworth PW, Reintgen DS, Leitch AM, Gabram SG, Lucci A, Cox CE, Hunt KK, Herndon JE 2nd, Giuliano AE. Surgical complications associated with sentinel lymph node biopsy: results from a prospective international cooperative group trial. Ann Surg Oncol 2006; 13: 491-500.
- Sakorafas GH, Peros G, Cataliotti L, Vlastos G. Lymphedema following axillary lymph node dissection for breast cancer. Surg Oncol 2006; 15: 153-165.
- Pavlista D, Eliska O. Relationship between the lymphatic drainage of the breast and the upper extremity: a postmortem study. Ann Surg Oncol 2012; 19: 3410-3415.
- Pavlista D, Koliba P, Eliska O. Axillary reverse mapping--chance to prevent lymphedema in breast cancer patients. Ceska Gynekol 2011; 76: 355-359.
- Boneti C, Korourian S, Diaz Z, Santiago C, Mumford S. Scientific Impact Award: Axillary reverse mapping (ARM) to identify and protect lymphatics draining the arm during axillary lymphadenectomy. Am J Surg 2009; 198: 482-487.
- Deng H, Chen L, Jia W, Chen K, Zeng Y. Safety study of axillary reverse mapping in the surgical treatment for breast cancer patients. J Cancer Res Clin Oncol 2011; 137: 1869-1874.
- Han JW, Seo YJ, Choi JE, Kang SH, Bae YK, Lee SJ. The efficacy of arm node preserving surgery using axillary reverse mapping for preventing lymphedema in patients with breast cancer. J Breast Cancer 2012; 15: 91-97.
- Gobardhan PD, Wijsman JH, van Dalen T, Klompenhouwer EG, van der Schelling GP. ARM: axillary reverse mapping-the need for selection of patients. Eur J Surg Oncol 2012; 38: 657-661.
- Britton TB, Solanki CK, Pinder SE, Mortimer PS, Peters AM. Lymphatic drainage pathways of the breast and the upper limb. Nucl Med Commun 2009; 30: 427-430.
- Noguchi M, Noguchi M, Nakano Y, Ohno Y, Kosaka T. Axillary reverse mapping using a fluorescence imaging system in breast cancer. J Surg Oncol 2012; 105: 229-234.
- Boneti C, Badgwell B, Robertson Y, Korourian S, Adkins L, Klimberg V. Axillary reverse mapping (ARM): initial results of phase II trial in preventing lymphedema after lymphadenectomy. Minerva Ginecol 2012; 64: 421-430.