Case Report - Current Pediatric Research (2017) Volume 21, Issue 3
Atypical presentation of Kawasaki disease in an Indian infant with intestinal pseudo-obstruction
Aniruddha Ghosh, Soumya Roy and Arunaloke Bhattacharya
Department of Pediatric Medicine, Institute of Child Health, Kolkata, West Bengal, India.
- *Corresponding Author:
- Aniruddha Ghosh
Department of Pediatric Medicine
Institute of Child Health, 11
Dr. Biresh Guha Street, Kolkata
700017, West Bengal, India.
Tel: +91 9432802876
E-mail: aniruddha179@gmail.com
Accepted date: May 23, 2017
Abstract
Acute abdomen in Kawasaki disease (KD) has been reported to occur in 1.4 to 4.6% of cases. Around 2 to 3% of patients with KD present with features of intestinal pseudo-obstruction. Vasulitis of the mesenteric artery with consequent ischaemia of the gut and dysfunction of the myenteric plexus has been linked to the pathogenesis of intestinal pseudo-obstruction in KD. The treatment of the acute abdomen in KD, whether conservative or surgical, is a matter of debate. However review of the available literature showed more consensuses towards conservative management with intravenous immunoglobulin (IVIg) and gut rest. We describe the case of a five months old male infant who presented with high fever, vomiting and prominent abdominal distension. He was ultimately diagnosed as a case of KD with intestinal pseudo-obstruction and successfully managed with conservative treatment.
Keywords
Immunoglobulin, Intestinal obstruction, Kawasaki disease, Pseudoobstruction.
Introduction
The diagnosis of Kawasaki Disease (KD) is established by the presence of fever of at least 5 days duration and four out of the five following criteria without any other explanation for the illness. The five principal criteria are: (i) Bilateral conjunctival injection; (ii) Changes in oropharyngeal mucosa including injected pharynx, injected or dry fissured lips, strawberry tongue; (iii) edema or erythema of hands or feet, desquamation beginning periungualy; (iv) Rash mainly truncal, non-vesicular, polymorphous; and (v) Cervical lymphadenopathy. Children with fever and less than four of the other features are classified to be having "incomplete" or "atypical" KD [1]. Acute abdomen in KD, although rare, is a well-recognised feature. It ranges from bowel infarction, focal colitis, intestinal obstruction due to ischemic strictures, and intestinal pseudoobstruction one hand to gallbladder hydrops with cholestasis, appendicular vasculitis and hemorrhagic duodenitis on the other [2,3]. We describe the case of a five months old male infant who presented with high fever, vomiting and prominent abdominal distension. He was ultimately diagnosed as a case of KD with intestinal pseudo-obstruction.
Case Report
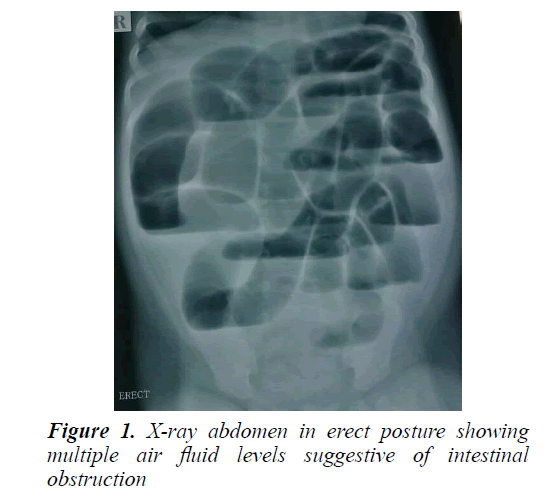
Five months old male baby was admitted with complaints of high grade fever for the last five days along with progressive abdominal distension and recurrent vomiting for the last two days. On examination, he was running a high fever with tachycardia and irritability. The abdomen was distended and diffusely tender with absence of peristaltic sounds. Initial investigations showed haemoglobin 11 g/dl, total leukocyte count (TLC) 10200/cm3 (86% neutrophilic preponderance), platelet count of 7,40,000/cm3 , CRP 60 mg/dl, sodium 130 mEq/L and potassium of 4.1 mEq/L. The renal and hepatic parameters were normal. Investigations for fever (microscopy as well as antigen test for malaria, dengue serology, Weil Felix test, IgM for scrub typhus, blood culture, urine routine examination and culture, Widal test, etc.) were non-contributory. In the mean-time, a straight x ray of the abdomen had been done which showed multiple air fluid levels, consistent with intestinal obstruction (Figure 1). Electrolytes, thyroid profile were normal. Ultrasonogram of the abdomen showed dilated bowel loops.
The child was put on intravenous fluids, with no oral feeds and a nasogastric tube was placed under continuous suction. Intravenous ceftriaxone and amikacin were started prophylactically. On the third day of admission, the baby showed frank bilateral non purulent conjunctival injection, oral mucositis (red tongue and oral mucosa) and skin peeling from the fingers. An echocardiography was done which showed dilatation of the left circumflex coronary artery and perivascular brightness in the left anterior descending as well as right coronary artery. A diagnosis of incomplete KD was made and intravenous immunoglobulin (IVIg) infusion at 2 g/kg was started, along with aspirin 50 mg/kg. Within 24 h, fever and abdominal distension disappeared, with improvement of general condition and return of intestinal peristaltic activity. The nasogastric tube was removed and repeated blood tests after 72 h of completion of immunoglobulin therapy showed TLC 8200/cm3, platelets 580000/cm3 and CRP 8 mg/dl. Ultrasonography of the abdomen was found to be within normal limits. He was discharged on day 8 of admission on aspirin 5 mg/kg and advice of follow-up. After 6 weeks repeat echocardiogram showed regression of dilation of affected coronary artery.
Discussion
The worldwide incidence of atypical KD is on the rise. The incidence has been reported to be 36.2% in USA, 15% in Taiwan and 10% in Japan [4]. Park et al. observed that some other predominant clinical feature is present in association with more than 50% cases of atypical KD, which makes the diagnosis and treatment of KD difficult for the paediatrician [5]. Although minor gastrointestinal complaints like vomiting and diarrhoea are common in KD, the occurrence of an acute abdomen in KD has been rarely reported [6]. The exact incidence of acute abdomen in KD is unknown. Trapani et al. [6] reported it to be between 1.4% and 2.6% whereas Tiao et al. [4] reported it to be 4.6%. However review of the available literature indicates its greater incidence in cases of atypical KD than in typical KD. For example, Zulian et al. found that, of all the ten patients of KD who had presented with acute abdomen, nine patients were suffering from atypical KD [3].
The occurrence of surgical complications in KD is a wellrecognised feature and ranges from bowel infarction, focal colitis, intestinal obstruction due to ischemic strictures, and intestinal pseudo-obstruction one hand to gallbladder hydrops with cholestasis, appendicular vasculitis and hemorrhagic duodenitis on the other [2,3]. Intestinal pseudoobstruction has been reported to occur in up to 2% to 3% of children with KD [2,4]. Miyake et al. found features of intestinal paralysis in seven out of 310 children with KD whereas Zulian et al. found severe abdominal complaints in ten out of 219 patients [3,7].
Vasulitis of the mesenteric artery with consequent ischaemia of the gut and dysfunction of the myenteric plexus leads to the development of intestinal pseudoobstruction in KD [2,4]. But imaging of the mesenteric vessels has failed to reveal any abnormality, thereby indicating small vessel vasculitis as the possible pathogenesis [2]. However mesenteric vasculitis has been histologically proven by Beiler et al in a sample taken from an ischaemic stricture of the proximal jejunum in a child with KD [8].
Lin et al. reported that surgery was necessary to relieve the fever despite having given IVIg therapy, whereas Trapani et al observed that IVIg was needed to relieve the fever despite having done surgery [9]. Thus the treatment of the acute abdomen in KD is a matter of debate. In the case series of Zulian et al, involving ten KD patients with acute abdomen, surgical treatment was done in eight patients [3]. Franken et al. [10], Wheeler et al. [11], Tiao et al. [4], Akikusa et al. [2] and others were of the opinion that laparotomy is unnecessary and conservative management is appropriate. Trapani et al. [6] suggested that laparotomy should be performed only in cases of true obstruction where clinical and radiological signs of peritonitis are evident. They observed that intestinal obstruction in KD should be managed conservatively, without going for surgical treatment [10].
Conclusion
Our case had conjunctivitis, oral mucositis and periungul desquamation along with fever and typical echocardiographic features and was thus consistent with the diagnosis of incomplete KD. He represents a typical case where a paediatrician may wrongly refer for an emergency laparotomy. Besides delay in recognising KD will also cause delay in starting IVIg, which in turn, may cause severe cardiac complications. Hence paediatricians need to be more aware of this possible association between KD and intestinal pseudo-obstruction. This case report also shows that conservative management of the pseudoobstruction along with proper treatment of the KD, is the treatment of choice in these cases.
References
- Vijayalakshmi AM, Gomathi V. Incomplete Kawasaki syndrome in an eighty days old male infant. Indian Pediatr 2002; 39: 485-488.
- Akikusa JD, Laxer RM, Friedman JN. Intestinal pseudoobstruction in Kawasaki disease. Pediatrics 2004; 113; e504-506.
- Zulian F , Falcini F, Zancan L, et al. Acute surgical abdomen as presenting manifestation of Kawasaki disease. J Pediatr 2003; 142: 731-735.
- Tiao MM, Huang LT, Liang CD, et al. Atypical Kawasaki disease presenting as intestinal pseudo-obstruction. J Formos Med Assoc 2006; 105: 252-255.
- Park AH, Batchra N, Rowley A, et al. Patterns of Kawasaki syndrome presentation. Int J Pediatr Otorhinolaryngol 1997; 40: 41-50.
- Trapani S, Montemaggi A, Simonini G, et al. Surgical abdomen with intestinal pseudo-obstruction as presenting feature of atypical Kawasaki disease. J Paediatr Child Health 2016; 1: 5.
- Miyake T, Kawamori J, Yoshida T, et al. Small bowel pseudo-obstruction in Kawasaki disease. Pediatr Radiol 1987; 17: 383-386.
- Beiler HA , Schmidt KG, von Herbay A, et al. Ischemic small bowel strictures in a case of incomplete Kawasaki disease. J Pediatr Surg 2001; 36: 648-650.
- Li LY, Jye CT, Chia LK, et al. Surgical treatment of Kawasaki disease with intestinal pseudo-obstruction. Indian J Pediatr 2011; 78: 237-239.
- Franken EA Jr, Kleiman MB, Norins AL, et al. Intestinal pseudo-obstruction in mucocutaneous lymph-node syndrome. Radiology 1979; 130: 649-651.
- Wheeler RA, Najmaldin AS, Soubra M, et al. Surgical presentation of Kawasaki disease (mucocutaneous lymph node syndrome). Br J Surg 1990; 77: 1273-1274.