Research Article - Biomedical Research (2018) Volume 29, Issue 9
Association of MMP-1, 9, 12 and TIMP-1 gene polymorphisms in Malaysian male hypertensive subjects
Farizeh Aalam Ghomi Tabatabaee1, Ramachandran Vasudevan2*, Farzad Heidari1, Somayeh Khazaei1, Ali Etemad1 and Patimah Ismail1*
1Department of Biomedical Science, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Selangor, Malaysia
2Malaysian Research Institute on Aging, Universiti Putra Malaysia, Selangor, Malaysia
- *Corresponding Authors:
- Ramachandran Vasudevan
Malaysian Research Institute on Aging
Universiti Putra Malaysia, Malaysia
Patimah Ismail
Department of Biomedical Sciences
Faculty of Medical and Health Science
Universiti Putra Malaysia, Malaysia
Accepted date: May 29, 2017
DOI: 10.4066/biomedicalresearch.29-17-470
Visit for more related articles at Biomedical ResearchAbstract
Background: Matrix Metalloproteinases (MMPs) plays an important role in hypertensive vascular stiffness, remodeling and dysfunction. Several studies have been reported the imbalanced MMP: TIMP (tissue inhibitors of metalloproteinase-1) ratio in hypertensive subjects, indicating the depressed systematic degradation of collagenase in etiology of hypertension. The main objective of this study was to determine the candidate gene polymorphisms involved in extracellular matrix metabolism among Malaysian male subject with Essential Hypertension (EH).
Methods: A total of 133 newly diagnosed EH subjects and 129 unrelated healthy individuals were included in this study. The genomic DNA was extracted and the genotyping was done by PCR-RFLP method.
Result: The demographic characteristic of the subjects such as age, body mass index, systolic blood pressure, diastolic blood pressure, low-density lipoprotein, triglyceride and cholesterol were shown to be significantly different (p?0.05) in case subjects when compared to controls. The allelic distribution of TIMP-1 372 T/C gene polymorphism was significantly associated with hypertension (p?0.05). While, MMP-1: rs1799750, MMP-9: rs3918242 and rs17576 and MMP-12: rs2276109 polymorphisms did not differ significantly (p?0.05).
Conclusion: Hence, the rs4898 polymorphism of TIMP-1 may be considered as a possible genetic biomarker and a risk factor predictor for EH among Malaysian male subjects.
Keywords
MMP1, MMP9, MMP12, TIMP1, Essential hypertension, Polymorphism
List of Abbreviations
MMPs: Matrix Metalloproteinases; TIMP: Tissue Inhibitors of Metalloproteinase-1; ECM: Extracellular Matrix; EH: Essential Hypertension; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure.
Introduction
Extracellular Matrix (ECM) act as network within the endothelial cells that provide elasticity and shape to the arteries [1]. Degradation of the ECM is fundamental in many aspects, both physiologically and pathologically [2,3]. The Matrix Metalloproteinases (MMPs) belong to the large family of the zinc-dependent endopeptidases involved in degradation of connective tissues and ECM proteins [4]. Their activity is well documented in major vascular complications particularly in hypertension [5]. The dysregulation can cause aggravated ECM degradation, which in turn provokes vascular smooth muscle cell migration, proliferation and inflammatory cells invasion to the vessel wall, bringing about vascular remodeling and stiffness [6]. Abnormal ECM metabolism has been reported in hypertensive subjects [5]. Where, decrease in MMP activity is accompanied by dysregulation of its inducer and activator proteins [7]. The plasma concentration of tissue inhibitors of metalloproteinase-1 (TIMP-1) was shown to be associated with arterial stiffness, greater systolic and diastolic dysfunction in hypertensive patients [8-11]. Multiple genetic and environmental factors involved in the development of hypertension [12]. Estimation of about 30-70% of genetic heritability believed to play a key role in blood pressure regulation [13]. Recently, some studies have evaluated the association of MMP gene polymorphisms with hypertension [14,15]. Several studies have been carried out on association between MMP gene single nucleotide polymorphisms (SNPs) and Cardiovascular Disease (CVD) in many populations, with conflicting results (Table 1). Some of these SNPs have been associated with higher Blood Pressure (BP) in hypertensive patients [16,17]. Data regarding TIMP-1 372 T/C polymorphism are scarce. The study of ischemic patients showed this SNP effects the drug responsiveness to nitrates in men [18]. Furthermore, higher plasma concentration of TIMP-1 was associated with T allele [19] in septic patients. To the best of our knowledge there were no former data available in respect to p MMP-1, 9, 12 and TIMP-1 gene polymorphisms, in relation to EH in Malaysian population. This initiated us to determine the possible association of MMP-1, 9, 12 and TIMP-1 polymorphisms in Malay male EH subjects.
| Gene variants | Diseases | Population/References | No. of subjects | p- value |
|---|---|---|---|---|
| MMP-9-C1562T | CAD | Brazilian Caucasian [20] | ||
| IS in T2DM | Tunisian [21] | 388 | NS | |
| CHD | Caucasian [22] | 471 | S | |
| Gestational hypertension | Czech Caucasian [23] | 158 | NS | |
| Hypertension | Northeastern Han Chinese [24] | 1765 | NS | |
| MMP-9-C1562T | AF | Chinese Han [25] | 881 | S |
| CAD | Polish [26] | 180 | NS | |
| CVD | Turkish [27] | 209 | NS | |
| EH | Turkish [15] | 224 | NS | |
| Hypertension | North-Eastern Han Chinese [24] | 1765 | NS | |
| MMP-9- R279Q | AF | Chinese Han [25] | 881 | NS |
| Stable CAD+ hypertension | Norwegians [28] | 1205 | NS | |
| Hypertension | Indonesian Javanese [14] | 100 | NS | |
| MMP-12-82A/G | AAA | Italian [29] | 846 | NS |
| IS in T2DM | Tunisian [21] | 388 | S | |
| CAD | Mexican Mestizo [30] | 300 | S | |
| Hypertension | Northeastern Han Chinese [24] | 1765 | S | |
| TIMP-1-372 T/C | Ischemic patients | Czech [18] | 537 | S |
| AAA | CAUCASIAN [31] | 279 | NS |
Table 1. Conflicting results of genetic variants of MMP and TIMP-1 genes in various populations.
Materials and Methods
Study subjects
Upon the ethical approval from the National Medical Research Register of Malaysia (NMRR) (Ref. No.: NMRR-12-1062-12), the case subjects were recruited from ''Klinik Kesihatan Senawang'', Seremban. A total of 300 subjects were approached for sample collection, out of which 38 samples were eliminated during the analysis due to outlier or skewness and genotyping errors. Overall, 133 newly diagnosed hypertensive patients with SBP (Systolic Blood Pressure) ≥ 140 mmHg and/or DBP (Diastolic Blood Pressure) ≥ 90 mmHg, Malay male aged ≥ 18 were included in our study. Patients with history of acute myocardial infarction, renal failure, cardiac failure, diabetes or those with medical conditions that can cause secondary form of hypertension were excluded. Furthermore, 129 healthy cases with SBP/ DBP˂140/90 mmHg and no family history of hypertension, diabetes, heart disease, high cholesterol, renal and kidney failure were considered as controls. The control subjects were selected from Seremban occupancies. The semi-assisted questionnaire prepared in Malay and English was given to each subject and based on their preference and the compliance to the inclusion criteria, informed consent was obtained from all the subjects. The socio-demographic information such as age, smoking habits and family history of disease were attained to assist the selection procedure. The blood pressure of the subjects were measured by Automated BP Meter (Omron, Japan), at the sitting position on the right arm after at least 5 min of sitting, however the average of two readings was calculated for the SBP and DBP.
Sampling and biochemical analysis
Five ml of peripheral blood was collected by a qualified phlebotomist and transferred to the EDTA tube (Becton Dickinson, NJ). The plasma was separated by centrifugation and stored under -80°C for further biochemical analysis. While, biochemical data of the patients were obtained from their medical records, lipid profile of the controls was measured by Roche Hitachi-911 Chemistry Analyzer (Hitachi, Japan) along with the kit supplied by Roche Diagnostics (Mannheim, Germany).
Genotyping methods
The FlexiGene® DNA kit (Qiagen Inc., Chatsworth, CA, USA) was used for genomic extraction from buffy coat. The quality and concentration of the extracted DNA was verified by the Q3000 UV Spectrophotometer and its analytical software V3.3.1 (Quawell, San Jose, CA, USA). Polymerase chain reaction technique was applied to amplify the genomic DNA using the primers synthesized by Focus Biotech Sdn Bhd (Table 2). The amplification of PCR products of MMP-1-1607 1G/2G (rs1799750), MMP-9-1562C˃T (rs3918242) and R279Q (rs17576), MMP-12-82A/G (rs2276109) and TIMP-1 gene 372 T/C (rs4898) polymorphisms were separately carried out in the total PCR reaction volume of 25 μl using PrimeG (Techne, Bibby Scientific, UK) thermo-cycler. The reaction mixture consisted of 7-8 μl of Prime Taq Premix (2X) (GenetBio, Korea), 0.5 to 0.7 μM of each prime, 100 ng of DNA. The amplified products were later digested with 3-4 Units of their respective REs (New England Biolabs, Beverly, USA) along with the provided NEB buffer in the total volume of 10 μl. The incubation of the RFLP product was done on 37°C for 30 min to 1 h according to the protocol provided by the manufacturer. The primers and enzymatic digestion specifications for screening of the variants using PCR- RFLP method are presented in Table 2. The sequencing result of the selected amplified products of the respective genes was confirmed with BLAST. These samples then served as positive controls in the later experiments. The non-template controls were also ran in all the experiments. The RFLP products were separated by 2-4% agarose gel in electrophoresis tank (Origins, Elchrom Scientific AG, Switzerland) at 100 v. The agarose gels were later stained by soaking into EtBr (0.5 μl/ml concentration; Bio-Rad, California, USA) and visualized by Alpha Imager (AlphaInnotech, San Leandro, USA). For validation, about 10% of randomly selected samples were genotyped using the same conditions and the results were 100% in concordance with previous results.
| Gene: variant | Forward Primer (FP) Reverse Primer (RP) |
Restriction enzyme | PCR product (bp) |
|---|---|---|---|
| MMP-1: rs1799750 | FP-5'TGACTTTTAAAACATAGTCTATGTTCA-3' | AluI | 269 |
| FP-5'TGACTTTTAAAACATAGTCTATGTTCA-3' | |||
| MMP-9: rs3918242 | FP-5′-GCCTGGCACATAGTAGGCCC-3′ | SphI | 435 |
| RP-5′-CTTCCTAGCCAGCCGGCA TC-3′ | |||
| MMP-9: rs17576 | FP-5′-GAGAGATGGGATGAACTG-3′ | MspI | 439 |
| RP-5′-GTGGTGGAAATGTGGTGT-3' | |||
| MMP-12: rs2276109 | FP-5′-GTCAAGGGATGATATCAGCT-3′ | PvuII | 137 |
| RP-5′-CTTCTAAACGGATCAATTCAG-3′ | |||
| TIMP-1: rs4898 | FP-5’-GCACATCACTACCTGCAGTC-3’ | BssSI | 175 |
| RP-5’-GAAACAAGCCCACGATTTAG-3’ |
Table 2. The primers and enzymatic digestion specifications for screening of the variants.
Results
Clinical characteristics
The clinical characteristics of the study subjects are represented in Table 3. The age of hypertensive subjects ranged between 23 to 65 years old with the mean of 49.10 ± 8.49 y, while the age of controls subjects varied between 18 to 63 y with the mean of 43.04 ± 12.24. The percentage of smoking in case and control subjects was 34.6% and 10.9%, respectively. The mean value of age, Body Mass Index (BMI), SBP, DBP, Low Density Lipoprotein (LDL), Triglycerides (TG) and Total Cholesterol (TC) were significantly higher in EH group as compared to the controls (P<0.05). Not much of difference could be seen when comparing the mean value of High Density Lipoprotein (HDL) between the case and control subjects (P>0.05).
| Factor | EH patients (133) | Controls (129) | p-value |
|---|---|---|---|
| Age (years) | 49.10 ± 8.49 | 43.04 ± 12.24 | 0.000* |
| BMI (kg/m2) | 28.96 ± 5.25 | 25.94 ± 5.28 | 0.000* |
| SBP (mm Hg) | 154.91 ± 10.93 | 119.86 ± 9.32 | 0.000* |
| DBP (mm Hg) | 95.28 ± 5.78 | 76.78 ± 8.64 | 0.000* |
| Smoking (Yes/No) | 34.60% | 10.90% | - |
| LDL (mmol/ L) | 3.19 ± 0 .93 | 2.76 ± 0.95 | 0.000* |
| HDL (mmol/ L) | 1.04 ± 0.22 | 1.05 ± 0.26 | 0.703* |
| TG (mmol/ L) | 1.64 ± 0.73 | 1.40 ± 0.76 | 0.011* |
| TC (mmol/ L) | 5.05 ± 1.11 | 4.74 ± 1.21 | 0.033* |
Table 3. Clinical and biochemical parameter of EH patients and control subjects.
Genotyping
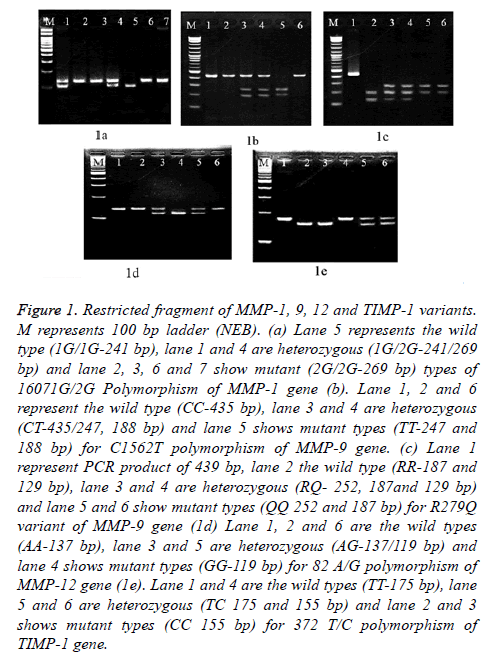
All the MMP and TIMP-1 gene variants were separated on 2-4% gel electrophoresis. Figure 1, illustrated the genotyping results of restricted fragments of the selected variants viewed under UV light.
Figure 1: Restricted fragment of MMP-1, 9, 12 and TIMP-1 variants. M represents 100 bp ladder (NEB). (a) Lane 5 represents the wild type (1G/1G-241 bp), lane 1 and 4 are heterozygous (1G/2G-241/269 bp) and lane 2, 3, 6 and 7 show mutant (2G/2G-269 bp) types of 16071G/2G Polymorphism of MMP-1 gene (b). Lane 1, 2 and 6 represent the wild type (CC-435 bp), lane 3 and 4 are heterozygous (CT-435/247, 188 bp) and lane 5 shows mutant types (TT-247 and 188 bp) for C1562T polymorphism of MMP-9 gene. (c) Lane 1 represent PCR product of 439 bp, lane 2 the wild type (RR-187 and 129 bp), lane 3 and 4 are heterozygous (RQ- 252, 187and 129 bp) and lane 5 and 6 show mutant types (QQ 252 and 187 bp) for R279Q variant of MMP-9 gene (1d) Lane 1, 2 and 6 are the wild types (AA-137 bp), lane 3 and 5 are heterozygous (AG-137/119 bp) and lane 4 shows mutant types (GG-119 bp) for 82 A/G polymorphism of MMP-12 gene (1e). Lane 1 and 4 are the wild types (TT-175 bp), lane 5 and 6 are heterozygous (TC 175 and 155 bp) and lane 2 and 3 shows mutant types (CC 155 bp) for 372 T/C polymorphism of TIMP-1 gene.
16071G/2G Polymorphism of MMP-1 gene
Table 4, represents the genotype and allele frequencies of MMP and TIMP-1 variants. There were no significant association in relation to genotype (p=0.954) and allele frequencies (p=0.925) between the cases and controls. We found high percentage of mutant (control: 46.5% and EH: 46.6%) and heterozygous (control: 45% and EH: 45.9%) in both the study groups.
C1562T and R279Q variants of MMP-9 gene
Concerning the C1562T variant, there could be no significant association detected in relation to genotype or allelic distribution of the subjects. The percentage of CC, CT and TT genotypes were 29.5%, 68.2% and 2.3% in controls compared to cases (33.1%, 63.9% and 3%). No significant differences in the genotypic distributions were observed in either group (p>0.05). Looking into genotypic and allelic frequencies of the R279Q polymorphism, the allelic frequency showed no significant difference between the hypertensive and control subjects (p=0.925). The percentage of the A (R) allele was 68.2% and 68.8% among controls and hypertensive subjects, respectively. Whereas, the percentage of the G (Q) allele was 31.8% in controls and 31.2% in cases (Table 4).
| Genotypes and alleles | Control subjects (n=129) n (%) | EH patients (n=133) n (%) | p- value | Odd ratio (95% CI) |
|---|---|---|---|---|
| MMP-1 1607 1G/2G | ||||
| 1G/1G | 11 (8.5%) | 10 (7.5%) | ||
| 1G/2G | 58 (45%) | 61 (45.9%) | ||
| 2G/2G | 60 (46.5%) | 62 (46.6%) | 0.954 | |
| 1G | 80 (31.1%) | 81(30.4%) | ||
| 2G | 178 (68.9%) | 185 (69.6%) | 0.925 | 0.974 (0.672-1.412) |
| MMP-9 C1562T | ||||
| CC | 38 (29.5%) | 44 (33.1%) | ||
| CT | 88 (68.2%) | 85 (63.9%) | ||
| TT | 3 (2.3%) | 4 (3.0%) | 0.751 | |
| C | 164 (64.1%) | 173 (65%) | ||
| T | 94(35.9%) | 93(35%) | 0.856 | 1.041 (0.729-1.487) |
| MMP-9 R279Q | ||||
| RR | 61 (47.2%) | 69 (51.9%) | ||
| RQ | 54 (41.9%) | 45 (33.8%) | ||
| 14 (10.9%) | 19 (14.3%) | 0.367 | ||
| R | 176 (68.2%) | 183 (68.8%) | ||
| Q | 82 (31.8%) | 83 (31.2%) | 0.925 | 1.027 (0.710-1.485) |
| MMP-12 82A/G | ||||
| AA | 122 (94.6%) | 125 (94.0%) | ||
| AG | 7 (5.4%) | 7 (5.3%) | ||
| GG | 0 | 1 (0.8%) | 0.614 | |
| A | 251(97.3%) | 257(96.9%) | ||
| G | 7 (2.7%) | 9 (3.4%) | 0.801 | 0.796 (0.292-2.171) |
| TIMP-1 372 T/C | ||||
| T | 140 (54.3%) | 118 (44.3%) | ||
| C | 118 (45.7%) | 148 (55.7%) | 0.023* | 0.672 (0.476-0.948) |
Table 4. Genotypic and allelic distribution of MMP and TIMP-1 variants.
82A/G polymorphism of MMP-12 gene
Table 4, illustrates the genotypic and allelic distribution of the 82A/G polymorphism of MMP-12 gene in the studied group. There was no significant difference in distribution of the genotypes and alleles between the hypertensives and controls. The percentage of 82A/G genotypes were 94%, 5.3% and 0.8% and 94.6% and 5.4% respectively for hypertensives and control subjects. We did not detect any GG in the controls. The percentage of A allele in controls and hypertensives were 97.3% and 96.9% respectively. Whereas, the percentage of G allele in control and the hypertensives were 2.7% and 3.4% respectively.
372 T/C polymorphism of TIMP-1 gene
The frequency of the T allele was 44.3% and 54.3% respectively in case and controls. Whereas, the frequency of C allele was 55.7% and 45.7% in case and controls, respectively. The allelic frequency of 372 T/C variant of TIMP-1 gene was significantly different in case and control subjects (p=0.023).
Discussion
Clinical and biochemical characteristics
Hypertension is associated with abnormalities in lipid profile level resulted from lipid metabolism alteration [32]. Several studies have been reported the association of lipid profiles in the hypertensive subjects with disagreeing results [15,33,34]. We evaluated association of clinical and biochemical characteristics with EH, which are tabulated in Table 3.
We found significant difference in the mean of age, BMI, SBP, DBP, LDL, TG and TC (p<0.05) between hypertensives and control subjects. Our results are in line with the study of lipid profile measures in South Asian elderly hypertensive subjects [35]. However, we could not find a significance difference in HDL level of the study groups, where the mean difference were 1.04 ± 0.22 and 1.05 ± 0.26 for case and controls, respectively. Untreated hypertensive patients experience abnormalities in lipoprotein metabolism and have higher plasma LDL /HDL ratio [36,37]. It has been demonstrated that high triglyceride and low HDL cholesterol can serve as predictive value for CVD outcome and high TG/ HDL ratio is associated with arterial stiffness [38].
16071G/2G polymorphism of MMP-1 gene
A functional polymorphism resulting from an insertion of a guanosine at position-1607 in the promoter of MMP-1 gene enhances transcriptional activity [23]. While, the 2G allele reduces the risk of CHD in Caucasians [22], it also has been associated with higher MMP1 antigen level in Polish patients with coexisting CHD and T2DM [39]. We found high percentage of mutant (control: 46.5% and EH: 46.6%) and heterozygous (control: 45% and EH: 45.9%) in both the study groups. It may be explained by the fact that, there was high number of overweight and obese in both the study groups [40]. The percentage of obese and overweight was 22.5% and 26.4% in controls. While, in the cases the values were corresponding to 37.6% and 44.4%. This polymorphism was associated with BMI in Korean population aged above 50 and the 1G allele depicted as protective effect against weight gain [40]. We could only find the similar results in Japanese and Iranians myocardial infarction subjects [41,42]. Furthermore, these findings are supported by the recent study conducted on Northeastern Han Chinese hypertensive subjects [24]. Collectively, data suggest that this polymorphism is unlikely to be a risk factor or a candidate gene for the development of hypertension in various populations.
C1562T and R279Q variants of MMP-9 gene
The MMP-9, also known as gelatinase B or 92-kDa type IV collagenase, is one member of the MMP family contributes to both normal and pathological tissue remodeling [42]. The polymorphism at position-1562 caused by a single base change C → T results in the loss of binding of a nuclear protein to this region of the MMP-9 gene promoter and increased transcriptional activity [25]. The T allele was associated with higher blood pressure and arterial stiffness in hypertensives [17]. This polymorphism (rs3918242) was also studied in relation with AF, CAD and CVD [25-27]. Another polymorphism R279Q (rs17576) of MMP-9 gene located at exon 6, is A to G substitution that results in change in amino acid arginine (R) to glutamine (Q) which lowers the catalytic domain activity of the enzyme [25]. The R279Q variant was evaluated in association with carotid artery [43,44] and hypertension [14,28]. Moreover, increased plasma level of MMP-9 was associated with hypertension [45]. As a result, MMP-9 gene polymorphisms may be considered as functional candidate genes for ischemic stroke and hypertension.
Concerning the C1562T variant, there could be no significant association detected in relation to genotype or allelic distribution of the subjects. The results are well in line with other populations where, there was no significant difference in Northeastern Han Chinese and Turkish hypertensive subjects [15,24]. However, not in accordance with other studies done in isolated systolic hypertension among Han Chinese [33]. This study was the first to evaluate the association of MMP-9 C1562T polymorphism with hypertension among Malay males. MMP-9 enzyme level might be a risk factor for hypertension [45] but, C1562T variant shows no association (p>0.05) with EH susceptibility. Looking into genotypic and allelic frequencies of the R279Q polymorphism, No significant association could be seen in genotype or allele frequencies in either of the study groups (p˃0.05). Our results are in contrast with the other study reported an association of G (Q) allele with hypertension [28]. Our results are in line with the study of arterial fibrillation in hypertensive heart disease patients of Chinese Han population [25] and Indonesian Javanese hypertensive subjects [14].
82A/G polymorphism of MMP-12 gene
The MMP-12 enzyme secreted mainly by macrophages acts on variety of ECM substrates such as heparin, entactin, gelatin, fibronectin, elastin and type IV collagen [43]. This functional polymorphism located at position-82 causes an A to G substitution that affects the AP-1 binding site in the MMP-12 gene, altering the expression of the gene [46]. This polymorphism had been studied in CAD [30], AAA [29] and ischemic patients [21] and it was suggested that, A allele was associated with smaller artery lumen in CAD patients with diabetes [46]. Despite of having diverse substrate specificity [43], data relation to this polymorphism are relatively inadequate. There was no significant difference in distribution of the genotypes and alleles between the hypertensives and controls. Our results are in line with the study conducted on carotid plaque susceptibility in Han Chinese population [47]. However, they failed to find any GG genotypes in either of their study groups. Nevertheless, the results are in disagreement with the findings of the latest study in Northeastern Han Chinese [24]. It may be concluded that, 82A/G variant of MMP-12 gene was implausible to be related to EH in Malaysian male subjects.
372 T/C polymorphism of TIMP-1 gene
Tissue inhibitor of metalloproteinase-1, is a glycoprotein engaged in ECM degradation and has broad substrate specificity over most MMPs [2]. Circulating levels of TIMP-1 were associated with Left ventricular diastolic impairment in hypertensives [11]. The TIMP-1 372 T/C polymorphism (rs4898) resulted from T to C substitution at position 372, was shown to be associated with survival rate in sepsis [19] and crohn's disease [48]. However, the association between 372 T/C gene polymorphism of TIMP-1, was not determined in hypertensive subjects. The allelic frequency of 372 T/C variant of TIMP-1 gene was significantly different in case and control subjects (p=0.023).
Hitherto, this polymorphism was not analysed in relation to hypertensives and any other diseases in Malaysia. An emergent amount of studies reported imbalance in MMP activity/ inhibition in hypertension [49-51]. The TIMP-1 gene is located on the X chromosome. Due to the nature of the analysis in Xlinked gene polymorphisms, there might be larger or no difference seen in genotypic distribution of this variant regarding the gender [19,48]. In this study, the 372 T/C polymorphism of TIMP-1 was significantly associated with EH (p=0.000) among Malay males. However, future study is recommended to perceive whether the same results can be extrapolated in females as well.
Study Limitations
The current study has to be interpreted within the context of its limitations. The study provided only the evidences of the association between genetic polymorphisms of ECM metabolism genes. This study did not address the mechanism or the functionality of the variants for the selected genes. The study groups were not age matched and our study was only focused on Malay male subjects. Age-matched association study needs to be done on the other ethnics; Chinese and Indians, as well to know the genetic risk factor for the development of hypertension in Malaysian population. It is necessary to investigate a large number of polymorphisms throughout the MMP, TIMP and the other genes, to perform association with hypertension and its complications. Also replication studies with larger samples and female subjects are strongly recommended to confirm the association of MMPs gene polymorphisms with hypertension.
Conclusions
The TIMP-1 gene polymorphism (372 T/C, rs4898) can be considered as an independent risk factor or a candidate gene polymorphism for the development of hypertension among Malay male subjects.
Ethics Approval and Consent to Participate
Approved by National Medical Research Register of Malaysia (NMRR) (Ref. No.: NMRR-12-1062-12). Consent was obtained from all the subjects prior conducting this study.
Consent for Publication
Not applicable
Availability of Data and Materials
All relevant datasets supporting the conclusions of this article are available within the article.
Competing Interests
The authors declare that they have no competing interests.
Funding
This study was supported by LRGS Project Grant No. 5525400.
Author’s Contributions
RV conceived the study and FAGT participated in the experimental design, data acquisition and analysis, interpretation of results, and drafted the manuscript. FAGT and RV interpreted the results, FH, SK, AE and PI critically reviewed the study for important intellectual content. All authors approved the final version of the manuscript.
Acknowledgements
The authors would like to extend their gratitude to all the volunteers who involved in this study.
References
- Katsuda S, Kaji T. Atherosclerosis and extracellular matrix. J Atheroscler Thromb 2003; 10: 267-274.
- Dollery CM, McEwan JR, Henney AM. Matrix metalloproteinases and cardiovascular disease. Circ Res 1995; 77: 863-868.
- Vargova V, Pytliak M, Mechirova V. Matrix metalloproteinases. in matrix metalloproteinase inhibitors: specificity of binding and structure-activity relationships (2nd ed.) Switzerland 2012.
- Onal IK, Altun B, Onal ED, Kirkpantur A, Gul Oz S, Turgan C. Serum levels of MMP-9 and TIMP-1 in primary hypertension and effect of antihypertensive treatment. Eur J Intern Med 2009; 20: 369-372.
- Raffetto JD, Khalil RA. Matrix metalloproteinases and their inhibitors in vascular remodeling and vascular disease. Biochem Pharmacol 2008; 75: 346-359.
- Lemarie CA, Tharaux PL, Lehoux S. Extracellular matrix alterations in hypertensive vascular remodeling. J Mol Cell Cardiol 2010; 48: 433-439.
- Ergul A, Portik-Dobos V, Hutchinson J, Franco J, Anstadt MP. Downregulation of vascular matrix metalloproteinase inducer and activator proteins in hypertensive patients. Am J Hypertens 2004; 17: 775-782.
- Flamant M, Placier S, Dubroca C, Esposito B, Lopes I, Chatziantoniou C, Tedgui A, Dussaule JC, Lehoux S. Role of matrix metalloproteinases in early hypertensive vascular remodeling. Hyperten 2007; 50: 212-218.
- Sekton BS. Matrix metalloproteinases-an overview. Res Rep Biol 2010; 1: 1-20.
- Cesana F, Alloni M, Sormani P, Colombo G,Maloberti A, Nava S, Galbiati M, Stucchi M, Cairo M, Corradi B, Castoldi G, Giannattasio C, Mancia G. TIMP1 plasma levels are correlated with arterial stiffening process. Artery Res 2011; 5: 169.
- Lindsay MM, Maxwell P, Dunn FG: TIMP-1. A marker of left ventricular diastolic dysfunction and fibrosis in hypertension. Hyperten 2002; 40: 136-141.
- Kuneš J, Zicha J. The interaction of genetic and environmental factors in the etiology of hypertension. Physiol Res 2009; 58: 33-41.
- Doris PA. The genetics of blood pressure and hypertension: the role of rare variation. Cardiovasc Ther 2011; 29: 37-45.
- Arjadi F, Aziz S, Muntafiah A. Metalloproteinase-9 gene variants and risk for hypertension among ethnic Javanese. Universa Med 2014; 33: 213-220.
- Bayramoglu A, Urhan Kucuk M, Guler H, Abaci O, Kucukkaya Y, Colak E. Is there any genetic predisposition of MMP-9 gene C1562T and MTHFR gene C677T polymorphisms with essential hypertension? Cytotech 2013; 67: 115-122.
- Mahmud A, Zhou S, Ryan AW, Jerrad-dunne P, Feely J. A haplotype at the MMP-9 locus is associated with high-blood pressure and arterial stiffness in patients with essential hypertension. Artery Res 2009; 3: 17-23.
- Zhou S, Feely J, Spiers JP. Matrix metalloproteinase-9 polymorphism contributes to blood pressure and arterial stiffness in essential hypertension. J Hum Hypertens 2007; 21: 861-867.
- Vasku A, Bienertova-Vasku J, Parenica J, Pavkova Goldbergova M, Novak J, Chmelikova M, Honsova D, Lipkova J, kala P, Spinar J. Central pulse pressure and variability in matrix metalloproteinases genes and their inhibitors in patients with ischemic heart disease. Physiol Res 2014; 63: 497-507.
- Lorente L, Martin M, Plasencia F, Sole-Violan J, Blanquer J, Labarta L, Diaz C, Borreguero-Leon JM,Jimenez A, Paramo JA, Orbe J, Rodriguez JA, Salido E. The 372 T/C genetic polymorphism of TIMP-1 is associated with serum levels of TIMP-1 and survival in patients with severe sepsis. Crit care 2013; 17: 94.
- Dalepiane VLN, Silvello DN, Paludo CA, Roisenberg I, Simon D. Matrix metalloproteinase gene polymorphisms in patients with coronary artery disease. Mol Biol 2007; 505-510.
- Chehaibi K, Hrira MY, Nouira S, Maatouk F, Hamda KB, Slimane MN. Matrix metalloproteinase-1 and matrix metalloproteinase-12 gene polymorphisms and the risk of ischemic stroke in a Tunisian population. J Neurol Sci 2014; 342: 107-113.
- Ye S, Gale C R, Martyn CN. Variation in the matrix metalloproteinase-1 gene and risk of coronary heart disease. Eur Heart J 2003; 24: 1668-1671.
- Jurajda M, Kankova K, Muzik J, Unzeitig V, Drabkova M, Izakovicova-Holla L, Vacha J. Lack of an association of a single nucleotide polymorphism in the promoter of the matrix metalloproteinase-1 gene in Czech women with pregnancy-induced hypertension. Gynecol Obstet Invest 2001; 52: 124-127.
- Qi Y, Zhao H, Wang Y, Lu C, Xiao Y, Wang B, Niu W. Genetic variants of the matrix metalloproteinase family genes and risk for hypertension: a case-control study among northeastern Han Chinese. Hypertens Res 2014; 37: 944-949.
- Gai X, Lan X, Luo Z, Wang F, Liang Y, Zhang H, Zhang W, Hou J, Huang M. Association of MMP-9 gene polymorphisms with atrial fibrillation in hypertensive heart disease patients. Clin Chim Acta 2009; 408: 105-109.
- Goracy J, Goracy I, Kaczmarczyk M, Brykczynski M, Widecka-Ostrowska K, Taryma O, Ciechanowicz A. Common genetic polymorphisms and environmental risk factors in Polish patients with angiographically documented coronary artery disease. Pol J Environ Stud 2011; 20: 1491-1499.
- Yaksel M, Kuzu-Okur H, Velioaylu A, Pelin Z. Matrix metalloproteinase-9 level and gene polymorphism in sleep disordered breathing patients with or without cardiovascular disorders. Balkan Med J 2013; 30: 8-12.
- Opstad TB, Pettersen AAR, Weiss TW, Akra S, Ovstebo R, Arnesen H, Seljeflot I. Genetic variation, gene-expression and circulating levels of matrix metalloproteinase-9 in patients with stable coronary artery disease. Clin Chim Acta 2012; 413: 113-120.
- Saracini C, Bolli P, Sticchi E, Pratesi G, Pulli R, Sofi F, Pratesi C, Gensini GF, Abbate R, Giusti B. Polymorphisms of genes involved in extracellular matrix remodeling and abdominal aortic aneurysm. J Vasc Surg 2012; 55: 171-179.
- Perez HN, Vargas G, Martinez N, Martinez MA, Pena MA,Pena AL, Valente B, Posadas C, Medina A, Rodriguez JM. The matrix metalloproteinase 2-1575 gene polymorphism is associated with the risk of developing myocardial infarction in Mexican patients. J Atheroscler Thromb 2012; 19: 718-727.
- Hinterseher I, Krex D, Kuhlisch E, Schmidt KG, Pilarsky C, Schneiders W, Saeger HD, Bergert H. Tissue inhibitor of metalloproteinase-1 (TIMP-1) polymorphisms in a Caucasian population with abdominal aortic aneurysm. World J Surg 2007; 31: 2248-2254.
- Harvey JM, Beevers DG. Biochemical investigation of hypertension. Ann Clin Biochem 1990; 27: 287-296.
- Huang R, Deng L, Shen A, Liu J, Ren H, Xu DL. Associations of MMP1, 3, 9 and TIMP3 genes polymorphism with isolated systolic hypertension in Chinese Han population. Int J Med Sci 2013; 10: 840-847.
- Osuji CU, Omejua EG, Onwubuya EI, Ahaneku GI. Serum lipid profile of newly diagnosed hypertensive patients in Nnewi, South-East Nigeria. Int J Hypertens 2012; 1-7.
- Kumar A. Correlation of serum paraoxonase activities in known cases of 130 elderly hypertensive South Asian aged 56-64 years-a hospital based study. Asian Pac J Trop Biomed 2014; 4: 189-197.
- Fuh MM, Shieh SM, Wu DA, Chen YD, Reaven GM. Abnormalities of carbohydrate and lipid metabolism in patients with hypertension. Arch Intern Med 1987; 147: 1035-1038.
- Chapman MJ. Therapeutic elevation of HDL-cholesterol to prevent atherosclerosis and coronary heart disease. Pharmacol Ther 2006; 111: 893-908.
- Urbina EM, Khoury PR, McCoy CE, Dolan LM, Daniels SR, Kimball TR. Triglyceride to HDL-C ratio and increased arterial stiffness in children, adolescents, and young adults. Pediat 2013, 131: 1082-1090.
- Drzewoski J, Sliwinska A, Przybylowska K, Sliwinski T, Kasznicki J, Zurawska-Klis M, Kosmalski M, Majsterek I. Gene polymorphisms and antigen levels of matrix metalloproteinase-1 in type 2 diabetes mellitus coexisting with coronary heart disease. Kardiol Pol 2008; 66: 1042-1049.
- Nho YK, Ha E, Yu KI, Chung JH, Wook NC, Chung IS, Lee MY, Shin DH. Matrix metalloproteinase-1 promoter is associated with body mass index in Korean population with aged greater or equal to 50 years. Clin Chim Acta 2008; 396: 14-17.
- Nojiri T, Morita H, Imai Y. Genetic variations of matrix metalloproteinase-1 and -3 promoter regions and their associations with susceptibility to myocardial infarction in Japanese. Int J Cardiol 2003; 92: 181-186.
- Ghaderian SMH, Akbarzadeh NR, Tabatabaei Panah AS. Genetic polymorphisms and plasma levels of matrix metalloproteinases and their relationships with developing acute myocardial infarction. Coron Artery Dis 2010; 21: 330-335.
- Sbardella D, Fasciglione GF, Gioia M, Ciaccio C, Tundo GR, Marini S, Coletta M. Human matrix metalloproteinases: an ubiquitarian class of enzymes involved in several pathological processes. Mol Aspects Med 2012; 33: 119-208.
- Armstrong C, Abilleira S, Sitzer M, Markus SH, Beven P. Polymorphisms in MMP family and TIMP genes and carotid artery intima-media thickness. Stroke 2007; 38: 2895-2899.
- Fontana V, Silva PS, Belo VA, Antonio RC, Ceron CS, Biagi C, Gerlach RF, Tanus-Santos JE. Consistent alterations of circulating matrix metalloproteinases levels in untreated hypertensives and in spontaneously hypertensive rats: a relevant pharmacological target. Basic Clinical Pharma Toxico 2011; 109: 130-137.
- Jormsjo S, Ye S, Moritz J, Walter DH, Dimmeler S, Zeiher AM, Henney A, Hamsten A, Eriksson P. Allele-specific regulation of matrix metalloproteinase-12 gene activity is associated with coronary artery luminal dimensions in diabetic patients with manifest coronary artery disease. Circ Res 2000; 86: 998-1003.
- Li W, Jin X, Zhou Y, Zhu M, Lin X, Hu X, Wang W, Wang F, Jin G. Lack of independent relationship between the MMP-12 gene polymorphism and carotid plaque susceptibility in the Chinese Han population. Vasc Med 2012; 17: 310-316.
- Meijer MJW, Mieremet-Ooms MAC, Van Hogezand RA, Lamers C, Hommes DW, Verspaget HW. Role of matrix metalloproteinase, tissue inhibitor of metalloproteinase and tumor necrosis factor-alpha single nucleotide gene polymorphisms in inflammatory bowel disease. World J Gastroenterol 2007; 13: 2960-2966.
- Derosa G, DAngelo A, Ciccarelli L. Matrix metalloproteinase-2, -9, and tissue inhibitor of metalloproteinase-1 in patients with hypertension. Endothe 2006; 13: 227-231.
- Tayebjee MH, Nadar SK, MacFadyen RJ, Lip GY. Tissue inhibitor of metalloproteinase-1 and matrix metalloproteinase-9 levels in patients with hypertension: Relationship to tissue Doppler indices of diastolic relaxation. Am J Hypertens 2004; 17: 770-774.
- Li FL, Edmunds E, Blann AD, Beevers DG, Lip GY. Matrix metalloproteinase-9 and tissue inhibitor metalloproteinase-1 levels in essential hypertension. Relationship to left ventricular mass and anti-hypertensive therapy. Int J Cardiol 2000; 75: 43-47.