- Biomedical Research (2016) Volume 27, Issue 3
Association of health-related quality of life with cardiovascular risk factors and subclinical atherosclerosis in non-diabetic asymptomatic adults.
Ovidiu Mitu*, Mihai Roca, Maria-Magdalena Leon, Andreea Gherasim, Mariana Graur, Florin MituFaculty of Medicine, I Medical Department, University of Medicine and Pharmacy “Grigore T. Popa” Iasi, 16 Universitatii St, Iasi, 700115, Romania
- *Corresponding Author:
- Ovidiu Mitu
I Medical Department,
University of Medicine and Pharmacy “Grigore T. Popa”
Romania
Accepted date: February 24, 2016
Abstract
Health-related quality of life (QoL) questionnaires represent easy-administered and useful tools in the medical clinical evaluation. An impaired health status seems to be associated with future cardiovascular (CV) events, but its role is not yet well established in asymptomatic subjects. The aim of our prospective study was to determine whether low values of health status (assessed by SF-36 questionnaire) were associated with CV or metabolic risk factors and future outcomes or with subclinical atherosclerosis in an urban population without CV diseases. We have evaluated 111 asymptomatic individuals, aged 35-75 years, 33.3% males. Each patient completed the SF-36 health survey and was evaluated comprehensively regarding CV risk factors; biochemical markers and the risk for developing CV or diabetes in the future by using SCORE and FINDRISC risk charts. Subclinical atherosclerosis was evaluated by measuring carotid intima-media thickness, ankle-brachial index, left ventricular mass index by echocardiography and aortic pulse wave velocity (PWV). After statistical analysis, female sex and obesity were correlated with low QoL levels. Age, blood pressure or other biochemical values were not associated with a decrease in QoL. Unlike SCORE, increased FINDRISC results were linked to low values both in mental and physical scores. Among subclinical atherosclerotic markers, only high values of PWV were related to a decrease of SF-36 survey on different scales. In conclusion, we recommend the use of easilyadministered health status questionnaires in asymptomatic subjects since they bring additional data on CV and metabolic changes, starting with subclinical stages. Thus, early preventive measures could be initiated.
Keywords
Health-related quality of life; SF-36; Cardiovascular; Subclinical atherosclerosis; Asymptomatic; Diabetes mellitus.
Introduction
The evaluation of general health status, either functional or physical, by simple methods has become of great interest in the last years. One of the most widely used tools is the healthrelated quality of life (QoL) questionnaire, the Short Form 36 Health Survey (SF-36) that was assigned for use in multiple domains, e.g. health policy evaluations, research, medical clinical practice as well as for general population [1]. It is a generic measure which contains multiple indicators of health and has been widely accepted because of its easiness in understanding, completion and interpretation of the results. Moreover, taking into account its wide accessibility and by developing general population norms, SF-36 health survey has become the main health status measure in medical studies [2,3]. It has been used for estimating and comparing numerous diseases in various medical fields such as: cardiovascular diseases, cancer, chronic obstructive pulmonary disease, psychiatric disorders, stroke, gastro-intestinal diseases, trauma or rheumatologic diseases [4]. SF-36 survey is structured in 36 multiple-choice items, each one receiving a score which sums into eight scales that finally form two major measures for the assessment of physical health and mental health. Higher scores are correlated with better health status.
Cardiovascular (CV) diseases represent the main cause of mortality worldwide with a prevalence that is continuously increasing. Prevention measures are needed urgently in order to detect the individuals that are at high risk for developing CV diseases. Thus, based on solid studies, various international societies have developed risk charts for the assessment of subjects’ CV risk profile, the most known being SCORE risk chart (Systematic Coronary Risk Evaluation) applicable for European countries or the Framingham risk score for North America. They take into consideration the main risk factors such as age, sex, cigarette smoking, blood pressure and cholesterol, but there are numerous others that contribute to CV disease progression-obesity, diabetes mellitus or chronic kidney disease [5]. However, in more than 30% of cases, an acute CV event (e.g. myocardial infarction, stroke) represents the first clinical manifestation of atherosclerotic burden. These are the reasons why prevention should be applied to all individuals even if they are asymptomatic, free of any CV diseases or diabetes. Recent and modern methods are now able to detect atherosclerotic alterations starting with subclinical stages and have been shown to predict future CV events. However, it is not very clear which patients may benefit at most from the use of these investigations since they are not widespread, are time-consuming or expensive.
A modest health-related QoL seems to be associated with CV risk factors in patients already diagnosed with heart disease [6]. However, in the asymptomatic population, there is little research that tried to determine the same relation. Thus, the aim of our study was to determine whether low values of health-related quality of life (assessed by SF-36 questionnaire) are associated with the presence of CV risk factors or with subclinical atherosclerosis in an asymptomatic, free of CV disease, urban population.
Methodology
Study population
Our current prospective study includes 111 naïve patients that were investigated in our cardiology department. They were randomized and referred to us through general practitioners, all subjects having urban residence.
All participants must have fulfilled the following inclusion criteria: aged 35-75, living in the urban area, women not being pregnant and, most important, not having a known disease or not having followed any treatment in the last 6 months for any CV, metabolic, renal, respiratory or cerebral diseases. The study was approved by the University Ethics Committee and all subjects have agreed and signed at the beginning an informed consent in order to take part in this study.
SF-36 health survey
The health-related QoL was assessed by using SF-36 health survey questionnaire. It contains 36 multiple-choice items and each question receive a score on a scale 0-100 (from the worst to the best possible health status) which are summarized and form eight scales regarding: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE), mental health (MH). Finally, the eight domains are converted into two major summary measures-the physical component summary (PCS) and the mental component summary (MCS). Lower scores are associated with poor health status.
SF-36 health survey is a registered trademark of Medical Outcomes Trust, USA, and a non-commercial license agreement was issued for the use of this questionnaire in the current study. SF-36 has already been tested and validated in the Romanian population, generating general population norms [7]. Population norms were used to compare our final scores, for all scales the norm being set at 50 as limit of normality [4]. In our study, the questionnaire was self-administered.
Cardiovascular risk factors
All patients were assessed according to the following clinical CV risk factors: age, sex, obesity defined by body mass index (BMI), systolic and diastolic blood pressure taken at rest and heart rate. We used the World Health Organization classification for BMI ranges for adults: normal weight – 18.5-24.9 kg/m2; overweight –25-29.9 kg/m2; obesity class 1– 30-34.9 kg/m2; obesity class 2–35-39.9 kg/m2; obesity class 3- ≥ 40 kg/m2.
We have analyzed the biochemical markers that have clinical CV relevance: lipid profile (total cholesterol, HDL, LDL, nonHDL and triglycerides), fasting plasma glucose, inflammatory status (fibrinogen), uric acid, total serum proteins, liver function profile assessed by transaminases (AST, ALT and GGT) and renal function assessed by glomerular filtration rate (GFR) using CKD-EPI formula for calculation.
Individually, we have applied the SCORE risk chart for determining the 10-year risk of CV mortality in our sample of asymptomatic population. For the risk of developing diabetes mellitus in the future, we have applied to each patient the most worldwide used questionnaire, the FINDRISC score, which is based on eight very simple multiple-choice questions. If the values in both scores (SCORE, respectively FINDRISC) are high, the risk of developing CV diseases or diabetes in the future is increased.
Subclinical atherosclerosis
Since the subjects had no previous diagnosis of any CV diseases, subclinical atherosclerosis was quantified by multiple modern methods. All investigations were performed by a single specialist with the same device.
Carotid intima media-thickness (IMT) was obtained by carotid ultrasound and interpreted according to the Mannheim criteria [8]. We took into consideration the highest value obtained from both sides. To evaluate peripheral artery obstruction, anklebrachial index (ABI) was calculated using systolic blood pressure readings from posterior tibial and dorsalis pedis, respectively brachial arteries. Arterial stiffness was evaluated by using an Arteriograph™ device and we retained for final analysis the aortic pulse wave velocity (PWV), systolic blood pressure (SBPao), pulse pressure (PPao) as well as aortic and brachial augmentation indexes (AIXao, respectively AIXbr) as subclinical markers. By performing cardiac echography, we were interested in the left ventricle ejection fraction (EF), left ventricle mass index (LVMI) and we observed the presence of aortic atheromatosis.
Statistical analysis
Data analysis was performed using SPSS 20.0 (Statistical Package for the Social Sciences, Chicago, Illinois). For continuous variables, data were presented as mean ± standard deviation (SD), these being compared by t-test for independent samples. Pearson’s correlation analysis was applied to assess the relationship between variables, calculating correlation coefficient (r). A two-sided p value <0.05 was considered significant for all data analyses. As well, the initial SF-36 data processing was performed by using the Health Outcomes Scoring Software 4.0.
Results
Sample characteristics
In the 111 analyzed subjects, the mean age was 51.87 ± 10.64 years, with one third being men. Most persons from this sample of apparently-healthy urban individuals were overweight, only 22.52% had a BMI <25 kg/m2, confirming the obesity tendency encountered nowadays. Arterial blood pressure was in normal ranges, as well as resting heart rate. Regarding usual biochemical markers, the asymptomatic urban population proved to be dyslipidemic, with total cholesterol, LDL and non HDL values over the superior limit. Moreover, women were more dyslipidemic while men had a more impaired hepatic function. As for subclinical atherosclerosis, the determined markers were in normal ranges. The obtained average values obtained by SCORE and FINDRISC risk charts classified the patients into the intermediate risk class for CV and metabolic diseases. All average descriptive values as well as target values are marked in table 1.
| Variable | Mean (n=111) |
Normal values | Women (n=74) |
Men (n=37) |
p value |
|---|---|---|---|---|---|
| Age (years) | 51.87 ± 10.64 | 50.91 ± 10.09 | 53.78 ± 11.56 | 0.182 | |
| BMI (kg/m²) | 28.84 ± 5.36 | <25 | 28.97 ± 5.95 | 28.56 ± 3.77 | 0.708 |
| SBP (mmHg) | 127.71 ± 17.15 | <140 | 126.81 ± 19.15 | 129.51 ± 12.27 | 0.436 |
| DBP (mmHg) | 81.62 ± 12.80 | <90 | 80.39 ± 14.00 | 84.08 ± 9.69 | 0.153 |
| HR (beats/min) | 67.78 ± 10.50 | <80 | 69.28 ± 9.83 | 64.78 ± 1126 | 0.033 |
| Total cholesterol (mg/dl) | 212.79 ± 44.99 | <200 | 216.85 ± 49.02 | 204.65 ± 34.78 | 0.179 |
| HDL cholesterol (mg/dl) | 51.54 ± 14.06 | >50 | 52.56 ± 14.00 | 49.38 ± 14.16 | 0.264 |
| LDL cholesterol (mg/dl) | 132.93 ± 40.21 | <130 | 138.23 ± 44.31 | 122.10 ± 27.63 | 0.048 |
| nonHDL cholesterol (mg/dl) | 161.23 ± 43.59 | <160 | 164.29 ± 48.12 | 155.26 ± 32.40 | 0.306 |
| Triglycerides (mg/dl) | 142.29 ± 81.75 | <150 | 130.30 ± 69.32 | 166.34 ± 98.93 | 0.028 |
| Plasma glucose (mg/dl) | 97.48 ± 12.62 | <106 | 94.90 ± 11.97 | 102.64 ± 12.55 | 0.002 |
| Fibrinogen (mg/dl) | 368.76 ± 77.80 | <400 | 380.35 ± 80.86 | 347.16 ± 67.62 | 0.038 |
| Uric acid (mg/dl) | 4.44 ± 1.63 | <6 | 3.84 ± 1.37 | 5.56 ± 1.44 | 0.001 |
| Serum proteins (g/dl) | 7.41 ± 0.59 | >7 | 7.40 ± 0.48 | 7.47 ± 0.57 | 0.479 |
| AST (mg/dl) | 24.33 ± 8.75 | <40 | 22.98 ± 8.14 | 27.09 ± 9.22 | 0.018 |
| ALT (mg/dl) | 26.88 ± 14.87 | <40 | 22.39 ± 11.05 | 35.90 ± 17.52 | 0.001 |
| GGT (mg/dl) | 35.87 ± 24.61 | <45 | 30.73 ± 24.50 | 45.90 ± 21.93 | 0.002 |
| GFR (ml/min/1.73m²) | 88.30 ± 16.39 | >90 | 86.55 ± 16.72 | 91.62 ± 15.28 | 0.126 |
| SCORE risk | 2.91 ± 2.71 | * | 2.17 ± 1.93 | 4.37 ± 3.40 | 0.001 |
| FINDRISC risk | 10.53 ± 4.53 | ** | 10.27 ± 4.43 | 11.05 ± 4.72 | 0.393 |
| IMT (mm) | 0.86 ± 0.12 | <0.90 | 0.82 ± 0.12 | 0.92 ± 0.11 | 0.001 |
| ABI | 1.06 ± 0.08 | >0.90 / < 1.40 | 1.07 ± 0.10 | 1.05 ± 0.05 | 0.587 |
| PWV (m/s) | 8.21 ± 1.74 | <10 | 8.33 ± 1.93 | 7.99 ± 1.20 | 0.334 |
| AIXao (%) | 36.57 ± 15.38 | >30 | 39.41 ± 15.27 | 31.49 ± 15.27 | 0.012 |
| AIXbr (%) | -1.96 ± 30.63 | <-10 | 3.93 ± 30.31 | -12.34 ± 28.53 | 0.009 |
| SBPao (mmHg) | 128.34 ± 20.86 | <135 | 128.66 ± 23.43 | 127.79 ± 15.49 | 0.841 |
| PPao (mmHg) | 46.57 ± 11.51 | *** | 48.17 ± 11.86 | 43.74 ± 10.31 | 0.060 |
| EF (%) | 67.66 ± 6.22 | >50 | 67.32 ± 6.32 | 68.33 ± 6.06 | 0.431 |
| LVMI (g/m²) | 101.48 ± 23.30 | <115 (men); <95 (women) | 96.27 ± 21.29 | 112.02 ± 23.90 | 0.001 |
| Aortic atheromatosis (%) | 71.17 | 63.5 | 86.5 | 0.014 | |
| Data are expressed as mean ± SD or in %. BMI: Body mass index; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; HR: Heart rate; HDL: High-density lipoprotein; LDL: Low-density lipoprotein; AST: Aspartate transaminase; ALT: Alanine transaminase; GGT: Gamma-glutamyltransferase; IMT: Intima-media thickness; AIXao/AIXbr–Aortic/brachial augmentation index; PPao: Aortic pulse pressure; LVMI: left ventricular mass index. *<1–low risk ≥1–<5 – moderate risk ≥5–<10 – high risk ≥10–very high risk **0-14–low-moderate risk 15-20–high risk 21-30–very high risk ***PP depends since it is the difference between SBP and DBP |
|||||
Table 1. Characteristics and average values of the study group (total and per gender)
Responses and internal consistency for SF-36 scales
All 111 participants responded to all questions of the health survey. Table 2 shows the overall means and standard deviations of the eight scales obtained by using SF-36 official software. The lowest results were obtained when assessing the vitality (VT=57.66) and bodily pain (BP=59.00) while the social functioning (SF=75.56) seemed to be the strongest point of the interviewed population. After summing the scales and applying the normative data, we obtained the two summaries data: PCS = 46.26 ± 7.75 and MCS = 46.90 ± 9.78.
| Scale | PF | RP | BP | GH | VT | SF | RE | MH | PCS | MCS |
| Mean | 71.71 | 68.92 | 59.00 | 59.57 | 57.66 | 75.56 | 68.77 | 67.17 | 46.26 | 46.90 |
| SD | 21.78 | 33.75 | 24.40 | 18.58 | 17.63 | 20.25 | 36.04 | 18.39 | 7.75 | 9.78 |
| Cαc | 0.85 | 0.72 | 0.87 | 0.75 | 0.76 | 0.65 | 0.69 | 0.77 |
Table 2. SF-36 score values obtained in our study.
The internal consistency of the survey was found acceptable, with Cronbach’s alpha coefficients varying from 0.65 for social functioning to 0.87 for bodily pain.
Relationship between SF-36 scales and CV risk factors
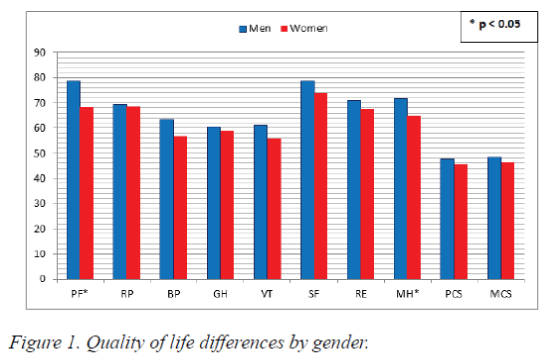
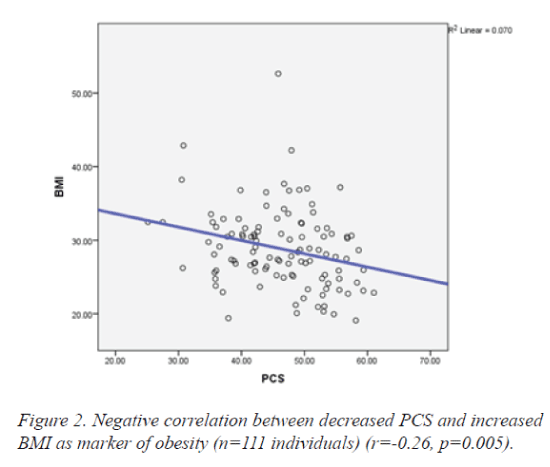
Age did not correlate with any of the SF-36 questionnaire parameters. As for sex, women reported lower levels of QoL on all scales, but with statistical significance only for PF (78.78 vs. 68.17, p = 0.012) and MH (71.78 vs. 64.86, p=0.05) (Figure 1). Furthermore, obesity (defined by BMI) was negatively correlated with almost all health-survey parameters and particularly with RP (r=-0.22; p=0.02), GH (r=-0.20; p=0.03) and PCS (r=-0.26; p=0.005). This means that an overweight or obese person tends to present a decreased QoL (especially physical components) as the BMI is rising (Figure 2).
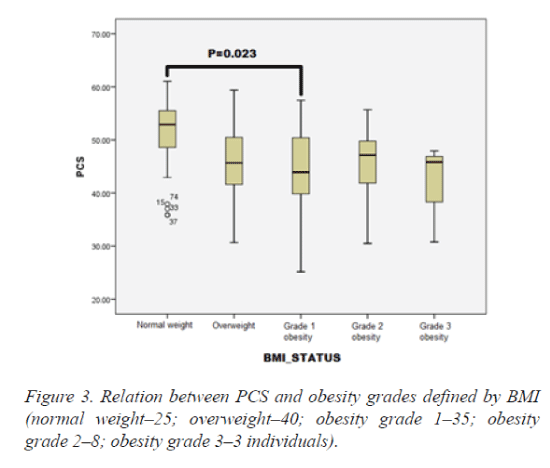
Moreover, by diving BMI into classes according to the definition, PCS proved to be significantly lower in subjects with obesity grade 1 (35 individuals) as compared to normal weight individuals (25 individuals) (Figure 3). Moreover, the PCS remained decreased in all classes of obesity. Heart rate, systolic and diastolic blood pressure presented no correlations with changes in health-related QoL.
Regarding biochemical markers, the only significant association was found between low levels of RE and increased levels of triglycerides (r=-0.20; p=0.033). The other lipid values (total cholesterol, LDL, HDL, nonHDL) as well as plasma glucose, fibrinogen, hepatic enzymes or GFR presented no correlation with SF-36 scales.
No significant relation was found between SF-36 results and future CV risk determined by SCORE risk chart. However, lower results in QoL scale responses were associated with an increased risk of developing diabetes in the future as assessed by using FINDRISC risk chart. This is particularly available for GH (r=-0.26; p=0.006) and SF (r=-0.21; p=0.025) scales and, even though the statistical significance was not reached, the same correlation was found for the two major summary measures-PCS (r=-0.14; p=0.1) and MCS (r=-0.13; p=0.1).
Relation between SF-36 scales and subclinical atherosclerosis
Carotid IMT presented no significant correlations with SF-36 results neither after dividing the study population into two subgroups according to the 0.9 mm limit. Likewise, echocardiographic measurements-EF, LVMI or aortic atheromatosis – were not associated with relevant changes in the QoL survey results. No relevant results were obtained by using ABI.
However, aortic stiffness parameters seemed to correlate better with general health status. Increased aortic PWV was associated with lower levels on all survey scales and especially with RP (r=-0.28; p=0.004). Furthermore, both augmentation indexes presented good relation with SF-36 health survey, especially with SF (for AIXbr: r=-0.20; p=0.036; respectively AIXao: r=-0.20; p=0.037). Moreover, by dividing subjects into two groups according to the PWV pathological limit (<10 m/s and ≥ 10 m/s), health status proved to be severely altered in the group with increased arterial stiffness with statistical significance for RP (p=0.012), GH (p=0.044), SF (p=0.045), RE (p=0.05) and PCS (p=0.05) (Table 3).
| SF-36 scale | PWV<10 m/s (n=89) |
PWV ≥ 10 m/s (n=22) |
p value |
| PF | 73.10 ± 21.98 | 65.00 ± 19.93 | 0.12 |
| RP | 72.55 ± 32.95 | 51.32 ± 32.78 | 0.012 |
| BP | 59.75 ± 24.96 | 55.37 ± 21.70 | 0.470 |
| GH | 61.11 ± 18.68 | 52.11 ± 16.54 | 0.044 |
| VT | 58.04 ± 17.33 | 55.79 ± 19.38 | 0.610 |
| SF | 77.31 ± 18.89 | 67.11 ± 24.72 | 0.045 |
| RE | 71.74 ± 35.26 | 54.39 ± 37.20 | 0.048 |
| MH | 68.09 ± 17.82 | 62.74 ± 20.83 | 0.25 |
| PCS | 46.85 ± 7.85 | 43.38 ± 6.63 | 0.05 |
| MCS | 47.50 ± 9.14 | 43.97 ± 12.30 | 0.15 |
Table 3. Health status differences in the presence of subclinical atherosclerosis (PWV ≥ 10 m/s).
Discussion
In the current study including 111 individuals with no CV or metabolic medical history, we aimed to analyze whether a poor health status was associated with the presence of CV risk factors, easily-determined biochemical values or, more important, with markers of subclinical atherosclerosis. We found important and useful correlations between some risk factors (sex, obesity, triglycerides), risk charts (FINDRISC) and subclinical atherosclerosis (assessed by PWV) and decreased QoL. This is one of the few studies that tried to investigate the possible association between health related QoL and biomarkers and, up to our present knowledge, the first study that aimed to assess a possible relation between altered health status and advanced subclinical atherosclerosis measured by multiple methods in an urban asymptomatic population. Thus, in clinical practice, by asking an apparently normal health individual to complete an easy questionnaire such as SF-36, we may trigger out possible subclinical atherosclerotic alterations that predispose the patient to a supplementary CV risk.
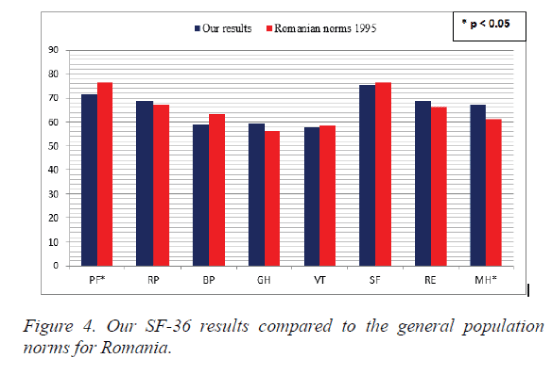
By comparing our results with the norms for the general Romanian population [7], the results were rather similar except for PF which was weaker in our study (71.71 vs. 76.51, p=0.03) and MH status that proved to be stronger in our free of disease individuals (67.17 vs. 61.19, p=0.001) (Figure 4). No population restrictions were made when SF-36 questionnaire was administered to the general Romanian sample in 1995, while our study limited the group only to apparently healthy individuals. Moreover, Mihaila et al. included subjects older than 18 while we have limited only the CV risk category, aged 35-75 years. These differences may explain partly why PF is superior in the Romanian general population (76.51 vs. 71.71, p=0.03). However, our sample performed better in MH (67.17 vs. 61.19, p=0.001) probably due to the non-inclusion in our study of persons affected by severe chronic diseases which may affect the mental status (e.g. CV, cerebral or metabolic ones) which was not the case in the survey that generated the Romanian SF-36 norms.
Our analyses revealed that some patient characteristics were significantly correlated with health-related QoL. Firstly, women reported lower QoL scores than men. Similar results were obtained in most other studies both in women with CV diseases as well as without CV diseases, suggesting that women were more prone to be rather affected by diseases [9]. Franco et al. proved over 10000 people that increasing age was correlated with poor physical health but higher mental health scores in both men and women (p<0.001) probably due to a general physical deterioration age-induced but possessing better internal adaptation to negative situations and life experiences [10]. In our study, no statistical association was found between age and health status even though our results had the same tendency as those mentioned above (for PCS: r=-0.04; p=0.6; respectively for MCS: r=0.07; p=0.4).
Obesity represents a major public health issue and is associated with high risk of CVD, diabetes, sleep diseases or psychological disorders. In our research, we have shown that health status is constantly dropping as the BMI (best marker of obesity) is increasing. This is particularly available for the physical component, logically explained by the limitations caused by the weight excess. Though PCS was constantly decreased in the overweight and obese subjects, the relative small number of individuals may explain why the statistical significance was obtained only for normal weight compared to obesity grade 1. Moreover, only 11 individuals had a BMI over 35 kg/m². Our results are consistent with those obtained in the literature, but with the particularity that in our study the population has no CV diseases at the moment of the examination which is mainly favorable for early initiation of preventive measures. Tan et al. showed on almost 5000 patients that the decrease in PCS due to obesity was achieved in women, while only men presented an association between obesity and MCS [11].
Even though we did not determine specifically, health related QoL is influenced by other risk and lifestyle factors. Physical activity has a beneficial effect over both components, physical and mental [12]. Smoking, one of the major CV risk factors, seems to have no influence over mental health, but affects the physical functioning mainly in men [10]. Abnormal sleep duration (less than 6 hours and more than 8 hours per day) is related to poorer self-perceived QoL, besides the general negative effects over health and mortality [13].
Our study did not include diabetic patients and we found no correlation between SF-36 scores and plasma glucose. However, we revealed important associations between decreased mental and physical summaries and the risk for developing diabetes in the future by using a standardized risk chart (FINDRISC). This result may be of important clinical use since an altered QoL may predict and favor the onset of diabetes in asymptomatic individuals. Other previous studies confirmed that fasting glucose was not associated with lower values of QoL compared to glycosylated haemoglobin which was significantly associated with worse health outcomes [14].
Though lipid values (total cholesterol, HDL, LDL or triglycerides) or inflammatory markers (e.g. fibrinogen) usually correlates with future CV events, we have only detected a modest correlation between high values of triglycerides and low values of emotional role (RE) scale. However, nor other studies have obtained significant correlations between lipid values and QoL scores [15].
Regarding subclinical atherosclerosis, we have compared health status with multiple methods of determining subclinical atherosclerosis: aortic atheromatosis, LVMI, ABI, carotid IMT and PWV for arterial stiffness. Among all these, only high values of PWV proved to correlate with decreased QoL, especially after diving PWV into two groups according to its pathological limit (<10, respectively ≥10 m/s). The literature data on this subject are rather limited and inconsistent. Other studies have reported positive associations between mental health status and depressive symptoms and IMT, especially in older adults [16,17]. Ohira et al. showed that thicker IMT was positively associated with anger score, stronger in men than in women. However, no correlations were obtained between depressive symptoms and IMT [18]. Another marker of subclinical atherosclerosis is coronary artery calcification (CAC) evaluated by multi-slice computer tomography. A recent published cross-sectional study showed that, out of several psychological factors, only trait anxiety was significantly correlated with CAC [19]. Moreover, Roux et al. published in 2006 a study that included more than 6500 adults with no history of CV diseases as it is the case of our research. They evaluated subclinical atherosclerosis by using CAC and physiological factors by using multiple validated scales. Their conclusion was that health status (chronic stress burden, anxiety, anger or depression) was not associated with coronary atherosclerosis in asymptomatic population [20]. Like in other studies, ABI proved no correlations with psychological markers [19]. Thus, by obtaining significant association between decreased QoL and increased PWV as marker of subclinical atherosclerosis, our results bring new and valuable data regarding CV risk, especially in a sample of asymptomatic adults.
Conclusions
Simple QoL health surveys, such as SF-36 questionnaire, could provide relevant clinical information besides the evaluation of depressive traits or other physical and mental components.
In our prospective study conducted on individuals without CV and metabolic diseases, we have shown that female sex and obesity are associated with decreased QoL score. Age, blood pressure or other biochemical markers do not present the same correlation. Decreased QoL is linked to higher risk of developing diabetes in the future, assessed by FINDRISC risk chart. Finally, out of multiple methods of determining subclinical atherosclerosis, only high values of PWV are associated with low values in the health status evaluation.
Thus, we recommend the use of easy administered health survey questionnaires, such as SF-36, in asymptomatic individuals since they bring additional information regarding CV and metabolic risk.
Acknowledgment
This paper was published under the frame of European Social Found, Human Resources Development Operational Programme 2007-2013, project no. POSDRU/159/1.5/136893.
References
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473-483.
- Reed PJ, Moore DD. SF-36 as a predictor of health states. Value Health 2000; 3: 202-207.
- Teodor D, Juganariu G, Miftode E. Use of Sf-36 Questionnaire in Evaluating the Quality Of Life of Hepatitis C Patients on Antiviral Therapy - Pilot Study. Revista de cercetaresiinterventiesociala 2014; 44: 253-265.
- Turner-Bowker DM, Bartley PJ, Ware JE Jr. SF-36® Health Survey & “SF” Bibliography: 3rd Ed. QualityMetric Incorporated, Lincoln 2002.
- Berger JS, Jordan CO, Lloyd-Jones D, Blumenthal RS. Screening for cardiovascular risk in asymptomatic patients. J Am CollCardiol 2010; 55: 1169-1177.
- De Smedt D, Clays E, Annemans L, Doyle F, Kotseva K, Pająk A, Prugger C, Jennings C, Wood D, De Bacquer D. Health related quality of life in coronary patients and its association with their cardiovascular risk profile: results from the EUROASPIRE III survey. Int J Cardiol 2013; 168: 898-903.
- Mihaila V, Enachescu D, Badulescu M. General Population Norms for Romanian using the Short Form 36 Health Survey (SF-36). QoL Newsletter 2001; 26: 17-18.
- Touboul PJ, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, Csiba L, Desvarieux M, Ebrahim S, Hernandez Hernandez R, Jaff M, KownatorS,Naqvi T, Prati P, Rundek T, Sitzer M, Schminke U, Tardif JC, Taylor A, Vicaut E, Woo KS. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). Cerebrovasc Dis 2012; 34: 290-296.
- Xie J, Wu EQ, Zheng ZJ, Sullivan PW, Zhan L, Labarthe DR. Patient-reported health status in coronary heart disease in the United States: age, sex, racial, and ethnic differences. Circulation 2008; 118: 491-497.
- Franco OH, Wong YL, Kandala NB, Ferrie JE, Dorn JM, Kivimäki M, Clarke A, Donahue RP, Manoux AS, Freudenheim JL, Trevisan M, Stranges S. Cross-cultural comparison of correlates of quality of life and health status: the Whitehall II Study (UK) and the Western New York Health Study (US). Eur J Epidemiol 2012; 27: 255-265.
- Tan ML, Wee HL, Lee J, Ma S, Heng D, Tai ES, Thumboo J. Association of anthropometric measures with SF-36v2 PCS and MCS in a multi-ethnic Asian population. Qual Life Res 2013; 22: 801-810.
- McAuley E, Konopack JF, Motl RW, Morris KS, Doerksen SE, Rosengren KR. Physical activity and quality of life in older adults: influence of health status and self-efficacy. Ann Behav Med 2006; 31: 99-103.
- Stranges S, Dorn JM, Shipley MJ, Kandala NB, Trevisan M, Miller MA, Donahue RP, Hovey KM, Ferrie JE, Marmot MG, Cappuccio FP. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol 2008; 168: 1353-1364.
- Lee DT, Choi KC, Chair SY, Yu DS, Lau ST. Psychological distress mediates the effects of socio-demographic and clinical characteristics on the physical health component of health-related quality of life in patients with coronary heart disease. Eur J PrevCardiol 2014; 21: 107-116.
- Sevinç S, Akyol AD. Cardiac risk factors and quality of life in patients with coronary artery disease. J ClinNurs 2010; 19: 1315-1325.
- Stewart JC, Janicki DL, Muldoon MF, Sutton-Tyrrell K, Kamarck TW. Negative emotions and 3-year progression of subclinical atherosclerosis. Arch Gen Psychiatry 2007; 64: 225-233.
- Faramawi MF, Gustat J, Wildman RP, Rice J, Johnson E, Sherwin R. Relation between depressive symptoms and common carotid artery atherosclerosis in American persons ≥ 65 years of age. Am J Cardiol 2007; 99: 1610-1613.
- Ohira T, Diez Roux AV, Polak JF, Homma S, Iso H, Wasserman BA. Associations of anger, anxiety, and depressive symptoms with carotid arterial wall thickness: the multi-ethnic study of atherosclerosis. Psychosom Med 2012; 74: 517-525.
- Hernandez R, Allen NB, Liu K, Stamler J, Reid KJ, Zee PC, Wu D, Kang J, Garside DB, Daviglus ML. Association of depressive symptoms, trait anxiety, and perceived stress with subclinical atherosclerosis: results from the Chicago Healthy Aging Study (CHAS). Prev Med 2014; 61: 54-60.
- Diez Roux AV, Ranjit N, Powell L, Jackson S, Lewis TT, Shea S, Wu C. Psychosocial factors and coronary calcium in adults without clinical cardiovascular disease. Ann Intern Med 2006; 144: 822-831.