Research Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2019) Volume 9, Issue 67
Assessment of prescription patterns and drug use across the Kurdistan region.
Rawaz Tawfeeq*, Tarin Tahssen Obied, Aram Ommar
Hawler Medical University, Erbil, Iraq
- *Corresponding Author:
- Rawaz Tawfeeq
Hawler Medical University
Erbil, Iraq
E-mail: rawaz.dlzar@pha.hmu.edu.krd
Accepted date: April 26, 2019
Citation: Rawaz Tawfeeq et.al. Assessment of prescription patterns and drug use across the Kurdistan region. Asian J Biomed Pharmaceut Sci. 2019;9(67):7-12.
DOI: 10.35841/2249-622X.67.19-193
Visit for more related articles at Asian Journal of Biomedical and Pharmaceutical SciencesAbstract
Errors in drug prescriptions are the most common preventable medication errors encountered in clinical practices worldwide. The aim of this research is to examine the pattern of prescriptions and drug use in the Kurdistan region and to determine whether the drug prescribing was based on rational therapeutic consideration. A cross sectional-observational study was conducted in the Kurdistan region of Iraq over a period of five months. A total of 1000 prescriptions were selected randomly from different pharmacies and data obtained from each prescription. In these prescriptions a total of 2878 medications were prescribed. The percentage of medications including antibiotics, supplement, non-steroidal antiinflammatory drugs and other painkillers 51.8%, 44.2%, 31.8%, and 21.8% per encounter respectively. The average number of drugs per prescription was 2.8. Drugs prescribed by generic name were 27% and more than 98 per cent of prescriptions were handwritten. The duration of therapy was mentioned in 56.5% of prescriptions. However, the dose and dosage form of medications were recorded 62% and 87.3% respectively. The percentage of prescriptions signed by the prescriber was 88.1%.
Keywords
Prescriptions pattern, Medications use, Kurdistan region
Abbreviations
ABX: Antibiotics; BDZ: Benzodiazepines; Cl; Clearance; DDI: Drug-Drug Interactions; GP: General Practitioner; NSAID: Non-Steroidal Anti-Inflammatory Drug; PIM: Polypharmacy and potentially Inappropriate Medication; P.O: Per os; Rx: Prescription: WHO: World Health Organization
Introduction
As a research paper so eloquently put it: "Prescription writing is a science and an art, as it conveys the message from the prescriber to the patient [1]. Therefore, it is important to underline the proficiency needed in prescription writing.
Medication errors are quite common and a portion of them could result in the occurrence of adverse events, in which 10,070 prescription orders were collected [2]. Of these prescriptions, 530 medication errors were determined. That means that there were 5.3 errors in every 100-prescription order. As a consequence five of the 530 medication errors caused an adverse event in the patient. Physician computer order entry can prevent many of these medication errors and adverse events. By using these types of prescription orders 86% of medication errors, which would result in potential adverse event, would be prevented by using computer order entry [2]. Therefore monitoring and evaluation of prescription patterns and drug usage plays an important role in identifying the drug related problems and providing feedbacks to the prescriber in order to create awareness for the effective use of the drug [3].
Drug utilization can be defined as "The study of marketing, distribution, prescription, and use of drugs in a society with special emphasis on the resulting medical, social, and economic consequences" [4].
Previously, prescribing medications was only the right of physicians with various specialties, including those in dental, or in veterinary practices. As the role of other health care experts has been expanded (pharmacists, nurses) writing a prescription is extended to them [5].
Rational and effective prescribing
Till now there is no universally agreed upon definition to describe the rational and good prescription pattern. The WHO guidelines encourage the rational use of drugs and ensures that the patient receive medication according to their needs with the right dose and sufficient duration of therapy with lowest cost possible for the patient and community [5].
Interventions that could be used to promote more rational use of medicines are: A mandated multi-disciplinary approach to develop and evaluate interventions to encourage rational use of medicines; clinical guidelines; using an essential medicine list (Essential medicine are those that satisfy the health care needs of the population); committees to insure the safe and effective use of medication for example drug and therapeutic committee; pharmacotherapy training for undergraduate medical and paramedical students; continuing in-service medical education as a licensure requirement; supervision, audit and feedback; provision of unbiased information about medicine and two useful ways to disseminate information are through drug information center and drug bulletins; public education about medicine; avoidance of perverse financial incentives example the practitioner who earn money from the sale of medicines will prescribe more expensive medicine; regulatory measure to support rational use; sufficient government expenditure to ensure availability of medicine and staff [6].
The process of rational treatment according to WHO guideline
WHO guideline defines six steps for rational treatment. Step one determines and identify the patients complain and problem. Step two defines the therapeutic objective. Step three justify whether treatment meets the patients demand or not. Step four initiates the therapy. Step five delivers the required information, instruction and warning. Step six monitors (ceases) the medication [7].
Irrational or inappropriate prescribing
Irrational use of medication in both developed and developing countries is very common and this leads to medically inappropriate, ineffective and economically inefficient use of medication in clinical practices [3].
Drug misuse is a serious worldwide issue encountered nowadays and one of the most commonly misused medications are antibiotics. Irrational use of antibiotic is one of the major challenges globally as it results in resistance of antibiotic against a wide range of bacteria and limits it is usefulness as demonstrated [8], 17% of adults do not complete the course of antibiotic, 41% of patients do not know that antibiotic abuse is harmful while 23% purchase antibiotic without prescription. Another study conducted in Jordan [9]. The study involved randomly selected Iraqi residing in Amman, among 508 participants 62% of them agreed on purchasing antibiotics without prescriptions, 29% agreed to obtain antibiotic from relatives, 90% listed viral infection as an indication of antibiotic.
Prescribing can be inappropriate or irrational for many reasons, including wrong selection of medication, Poly pharmacy or prescribing multiple medications that could interact with each other, prescribing for conditions that are self-limiting, continuing to prescribe the medication for longer duration than needed. Moreover, they involve prescribing a low dose of medication and/or taking medication for short duration in which the patient will not get the benefit from drug especially the use of antibiotics instead of continuing the course of treatment to prevent antimicrobial resistance. Also, prescribing without discussing the treatment options with the patient and taking into consideration the patient needs make an inappropriate prescription [5].
To assess the problem of irrational use of medicines, prescribing, dispensing we should regularly monitor the type of irrational use so that to develop strategies towards changing specific problem, the amount of irrational use should be assessed to determine the size of the problem and the reason why medicines are used irrationally so that effective strategies can be chosen [6].
Poly-pharmacy
The word poly-pharmacy, which initially developed more than one and half centuries ago in the medical literatures to describe certain issues related to multidrug prescription and excessive drug usage. Poly-pharmacy and inappropriate medication (PIM) use is one the most commonly encountered problem in clinical practices related to drug use. It is more common in elderly population as a subsequent of multi-morbidities in such population [10]. The term poly-pharmacy is defined, as "the concomitant use of multiple drugs or the administration of more medications that are indicated clinically, is the leading cause of DDIs, resulting in higher rate of adverse events, higher drug costs, and medication non adherence" [11].
Guidance of prescribing
Abbreviation of title: Title of medication or any pharmaceutical preparation should be written in full in order to reduce the misinterpretation that could be resulted from unofficial abbreviation. That is why unofficial abbreviations should be avoided.
Non-proprietary title: Non-proprietary titles, also known as the generic name of drug, should be used in prescribing medication. This will allow the dispenser to dispense a suitable pharmaceutical product to the patient, thereby saving delay to the patient. The only exception is when there is a significant difference in clinical effect of formulation between different manufacturers, making it essential for the patient to take the same brand of medication for example in case of some epileptic medications. In these cases the brand name or the manufacturers name should be stated.
Prescription writing and elements of prescription:
• The prescription should be written in ink so as to be inerasable with clear handwriting.
• It should be dated
• It should contain the name and address of the patient.
• It should involve the address of prescriber.
• It should be signed by ink by prescriber.
• The age and date of birth of patient should be preferably be stated and it is a legal requirement in case of prescription only medicine to state the age of children under 12 years of age [12].
In order to reduce the occurrence of errors, all prescriptions should be written in legible hand-writing with black ink. Abbreviations documented in prescription writing guidelines such as p.o. (per os) may be used, however, to reduce human errors which may occur it may be best to avoid them and document information in full format. Dangerous abbreviations such as MgSO4 (magnesium sulphate) or MSO4 (morphine sulfate) are best avoided [13].
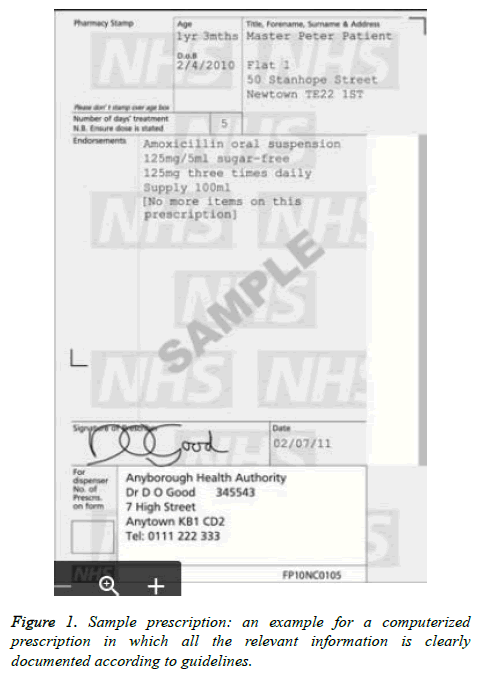
Computer-issued prescription: Based on guidance of joint GP and information technology committee, computer-issued prescription should apply to the following standard (Figure 1).
• The computer should print the date of writing the prescription, the patient’s surname, one forename, and other initials.
• The address of patient should be stated; also the patient’s date of birth is to be printed out.
• Age of children under 12 years and adults over 60 years must be printed. Age of children less than 5 years should be written in years and month.
• The prescribers’ name (who will normally sign the prescription) should be written at the bottom of prescription paper.
• Names of medication (both proprietary and non-proprietary name) must come from dictionary held in the computer memory. This reduces errors that can arise in spelling the name of medication.
• Advice should be written in full and should not interfere with clarity of prescription.
• Handwriting alteration should only be made on exceptional circumstances; it is preferable to print out a new prescription.
• Prescription for controlled drugs can be printed from computer but the prescriber signature should be handwritten [12].
Errors in prescribing are the most common preventable medication errors that occur in clinical practice in the world. Accumulated studies are conducted in different countries in order to determine the problems and then they play an important role in solving medication errors that occur.
Aim of the study
The purpose of the research is to study the pattern of drug prescribing in Kurdistan region and to determine whether the drug prescribing was based on rational therapeutic consideration.
Materials and Methods
A cross sectional-observational study was conducted across the Kurdistan region of Iraq from the provinces of Erbil, Duhok, Sulaymaniyah, Akre, Kalar. The study analyzed 1000 prescriptions over the period of five months (20.10.2017 to 20.3.2018). Prescriptions were collected randomly at different pharmacies and the pharmacists were informed to collect the prescriptions in each city. The prescriptions were collected from both public and private sector.
All the drugs prescribed were recorded including the numbers of drugs prescribed per prescription, quantity of medication prescribed, the percentage of prescription that were handwritten.
In this study we calculated the number of encounters with (antibiotic, supplement, NSAID, other painkiller) prescribed and determined whether the (duration of therapy, date of the prescription, name of the patient, address of the prescriber, sign of the prescriber, age of the patient, dose, dosage form) were involved in the prescription or not. Furthermore, the ratio of drug written in generic name to that written in brand was also determined.
Results
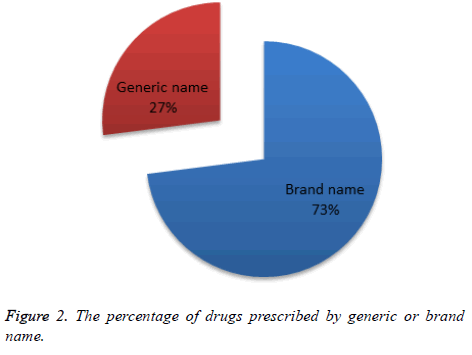
The prescriptions, which were randomly collected across the Kurdistan region, reached a total of 1000 prescriptions. From these prescriptions a sum of 2878 medications were prescribed for patients by healthcare professionals in order to treat ailments or improve the quality of life of the patient. To summarize the acquired the data, the mean number of drugs prescribed per prescription was determined to be 2.8 medications, and from these prescribed medications 27% were written in the form of their generic name, whilst the majority (73%) was prescribed in the form of their brand name (Figure 2).
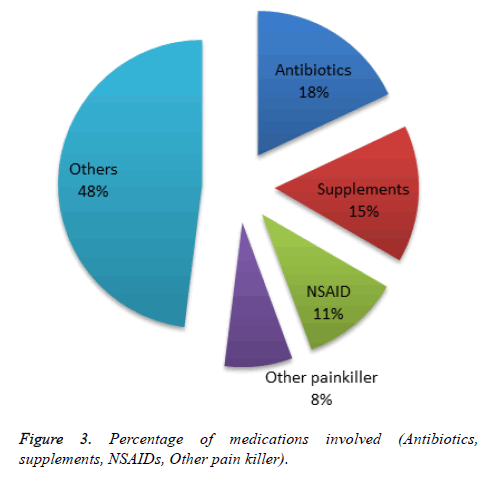
Next, from all these prescribed medications, it was found that the medications could be generalized into five main categories, namely supplements, antibiotics, supplements, NSAID’s, other painkillers, and a large category of medications denoted as “Others.” The percentage of medications prescribed belonging to the class of antibiotics was determined to be 18%, in other words, in one prescription there was a 51.8% chance that the prescription contained an antibiotic. Supplements accounted for about 15% (44.2% per encounter), whilst NSAID’s comprised about 11% (31.8% per encounter), other painkillers were found to be about 8% (21.8% per encounter) of the prescribed medications (Figure 3).
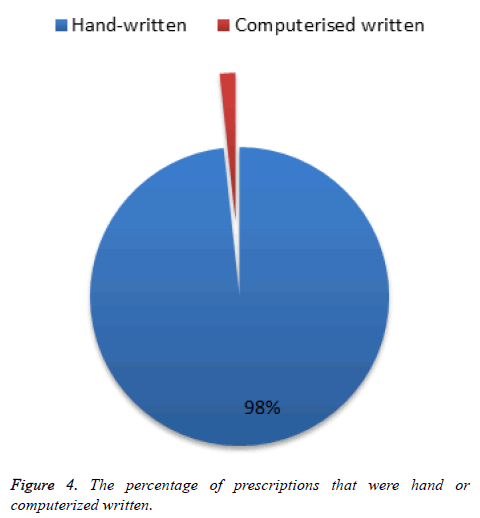
The majority of prescriptions 98.3% were written by hand whilst only a small fraction of 1.7% was written using a computerized system (Figure 4).
The duration of therapy to be implemented by the patient was mentioned in 56.5% of prescriptions, and the age of the patient was mentioned in 19.2% of the prescriptions. Patient names were absent in 7.2% of prescriptions. Date of the prescription was involved in 61.3% of prescriptions and the address of the prescriber was involved in 75% of prescriptions. However, the percentage of prescriptions which mentioned the dose and dosage form was 62% and 87.3% respectively. Also 88.1% of prescriptions were signed by the prescriber leaving 11.9% unsigned. The obtained data from the collected prescriptions are summarized in the Table 1.
| Variables | Number per 1000 Rx | Percentage (%) |
|---|---|---|
| Antibiotics | 518 | 51.8 |
| Supplements | 442 | 44.2 |
| NSAID | 318 | 31.8 |
| Other painkiller | 218 | 21.8 |
| Date of prescriptions | 613 | 61.3 |
| Duration of therapy | 565 | 56.5 |
| Name of patients | 928 | 92.8 |
| Address of prescriber | 750 | 75 |
| Signature of prescriber | 881 | 88.1 |
| Age | 192 | 19.2 |
| Dose | 620 | 62 |
| Dosage form | 873 | 87.3 |
Table 1. Data obtained from the collected prescriptions.
Discussion
In this study, 1000 prescriptions have been collected and analyzed; and a total of 2878 medications were prescribed. Studies on drug utilization patterns are essential for obtaining data and information about the quality of drug use and its aim towards educating the population for rational use of medication [14].
The average number of drugs per prescription was 2.8 that are higher than the suggested WHO criteria of less than two drugs per prescriptions. A study conducted in Delhi showed that the average number of drug per prescription ranged from 1.42 to 4.07 [3]. Another study from Lucknow's district reported that poly-pharmacy was common 3.1 ± 1.6 drug per prescription [1]. While another study in Islamic republic of Iran had reported a mean of 4.4 ± 1.7 drugs per prescription [15].
Poly-pharmacy increase the risk of drug-drug interaction, noncompliance, cost of therapy, errors in prescribing and the number of drug related problems per patient was in direct proportional to the number of drug used [14,16].
The numbers of drugs written in generic name were 777 drugs out of 2878 (27%), while the number of drugs written in brand name was 2101 drugs out of 2878 (73%). Low generic prescription of drug in Kurdistan region could reflect the influence of pharmaceutical companies. To change the situation the generic prescription of drugs by physician should be encouraged by regular educational program to improve prescribing practices among physicians. A study conducted that showed that only five prescriptions were written in generic name out of 600 prescriptions [17]. Another study from Jordan showed that the percentage of drugs prescribed by generic name was 5.1% [18]. While in northwest Ethiopia the percentage of drugs prescribed by generic name was high with average of 75% in health centers and 83% in health stations [19].
In this study, only 1.7% of prescriptions were computerized written, while 98.3% were handwritten. The computerized written prescription should be encouraged as they are more legible and huge number of errors could be avoided. As demonstrated [2], computer order entry systems reduced the frequency of medication errors, which could result in potential adverse event. Furthermore, computerized prescriptions could be integrated with other systems present in a hospital or polyclinic allowing the physician to access, record, and search for information more easily on a database.
Percentage of antibiotic (ABX) prescribed per encounter in this study was 51.8% and supplements were prescribed in 44.2% of encounters, while the pain killers were prescribed in 53.6% of encounters of which non-steroidal anti-inflammatory drugs formed 31.8%. In Pakistan antibiotics were prescribed in 52% of encounters [20]. While in Jordan the percentage of encounters with antibiotic range from 46.7% to 83.3% at different centers (21 center were involved in the study) [18]. It is very important to use antibiotic rationally, as overuse of antibiotic is associated with increasing rate of bacterial resistance and antibiotic become less effective against bacteria which has been sensitive to it before especially if the antibiotic is prescribed without a culture sensitivity test [19].
The percentage of prescriptions contained the name of the patient in this study were 92.8%, while the age of the patient were involved in 19.2% of prescriptions. It is important to involve the age of the patient in prescription as children differ from adults in their response to medication and special care is required in case of dispensing the medication to the elderly and neonates because the risk of toxicity is increased by decreasing the drug clearance (Cl) in these population age [12].
Duration of therapy was written in 56.5% of prescriptions. Absence of duration of therapy in drug prescription is regarded as irrational and can result in drug abuse as the patient may take the drug for shorter or longer duration and affect the efficacy of therapy. The dose and dosage form were written in 62% and 87.3% of prescription respectively.
In this study, we found that 61.3% of prescriptions involved the date of prescription, which is an important element of prescription especially for controlled drugs such as Benzodiazepines (BDZ), Barbiturates, Narcotics analgesics and others). Therefore the date of prescription should be involved in every prescription in order to prevent the use of same prescription for several times.
Among the other prescription requirements especially prescriptions containing controlled drugs is that prescriber should specify the prescribers address as well as its signature. In our study the address of prescribers were written in 75% of prescriptions and prescriber in 88.1% of prescriptions signed the prescriptions.
Conclusion
Our study reveals that the prescription pattern in Kurdistan region is poor in comparison with other systems used throughout the developed world, and the majority of medical practitioners are not adhering to the international standards of prescribing medications. The government authorities both ministry of health and the Kurdistan Syndicate of Pharmacists should encourage the rational use of medication in both the public and private sectors. This can be achieved through new applicable regulations and by formal interventions which can be done by pharmacists to make physicians aware of the situations in which they are likely to commit errors or through the application of proper training or the use of computerized prescriptions. As can be seen from Figure 4, only 1.7% of the collected prescriptions were computerized, which reflects on the nation’s poor usage of technology. Although handwritten prescriptions are generally quicker and simpler to complete, computerized prescriptions allowed the advantage of reducing the occurrence of human errors. It is also more favorable for a physician to prescribe using the medications generic name unless there are significant differences in bio equivalency or content between the same medicaments manufactured by different companies.
References
- Kumari R, Idris MZ, Bhushan V et al. Assessment of Prescription Pattern at the public health facilities of Lucknow district. Indian J Pharmacol. 2008;40:243-7.
- Bates DW, Boyle DL, Vander Vliet MB et al. Relationship between medication errors and adverse drug events. J Gen Intern Med. 1995;10:199-205.
- Biswas NR, Biswas RS, Pal PS et al. Pattern of prescription and drug use in two tertiary hospital in Delhi. Indian J Physiol Pharmacol. 2000;44:109-12.
- Shewade PS, Shashindran D, Bapha C. Drug utilization studies. National Med J of India. 1998;1:185-9.
- Whittlesea C, Hodson K. Clinical Pharmacy and Therapeutics (6th edn.), Elsevier, London, UK. 2018.
- Promoting rational use of medicine: core components. WHO Policy Perspectives on Medicines. 2018;1-6.
- Vries TPGM De, Henning RH, Hogerzeil HV. Guide to good prescribing (3rd edn.) WHO Geneva, Switzerland. 1994.
- Hameed A, Naveed S, Qamar F. Irrational use of antibiotic, in different age groups of Karachi: A wakeup call for antibiotic resistance and future infections. J Bioequi and Bioavailab. 2016;8:242-5.
- Darwish D, Abdelmalek S, Dayyih W, et al. Awareness of antibiotic use and antimicribial resistance in iraqi community in Jordan. J Infect Dev Ctries. 2014;8:616-23
- Mortazavi SS, Shati M, Keshtkar A, et al. Defining polypharmacy in the elderly: A systematic review protocol. BMJ Open. 2016;6:1-4.
- Zeind CS, Carvalho MG. Drug interaction (11th edn.) Wolters Kluwer Health Press, London, United Kingdom. 2018.
- Ah-See K, Badminton M, Bahl A, et al. British national formulary. ( 70th edn.) BMJ, London, United Kingdom. 2018.
- Samaranayake NR, Dabare PR, Wanigatunge CA et al. The pattern of abbreviation use in prescriptions: A way forward in eliminating error-prone abbreviations and standardisation of prescriptions. Curr Drug Saf. 2014;9:34-42.
- Moghadamnia AA, Mirbolooki MR, Aghili MB. General practitioner prescribing patterns in Babol city, Islamic Republic of Iran. East Mediterr Health J. 2002;8:550-5.
- Shankar PR, Dubey AK, Rana MS, et al. Drug Utilization with special Reference to Antimicrobials in a subhealth post in western Nepal. J Nepal Health Res Council. 2005;3:65-9.
- Viktil KK, Blix HS, Moger TA, et al. Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug-related problems. Br J Clin Pharmacol. 2007;63:187-95.
- Otoom S, Batieha A, Hadidi H et al. Evaluation of drug use in Jordan using WHO prescribing indicators. East Mediterr Health J. 2002;8:537-43.
- Rahman Z, Nazneen R, Begum M. Evaluation of prescribing pattern of the private practitioners by the undergraduate medical students. Bangladesh J Pharmacol. 2009;4:73-75.
- Desta Z, Abula T, Beyene L. Assessment of rational drug use and prescribing in primary health care facilities in north west Ethiopia. East Afr Med J. 1997;74:758-63.
- Hafeez A, Kiani AG, Ud Din S et al. Prescription and dispensing practices in public sector health facilities in Pakistan: Survey report. J Pak Med Assoc. 2004;54:187-91.