Research Article - Journal of Parasitic Diseases: Diagnosis and Therapy (2018) Volume 3, Issue 1
Assessment of intestinal parasites among children taking antiparasitic drugs at Ngoma primary school, Rwanda.
Zéphanie Nzeyimana1, Thaddée Nshimiyimana2, Jean Marie Vianney Nyumbayire3, Filmin Uwihoreye4, Osuwat Lawrence Obado1 and Jean Baptiste Niyibizi1,5,6*
1Department of Medical Laboratory Sciences, Mount Kenya University Rwanda, Kigali campus
2Department of Biomedical Laboratory Sciences, University of Rwanda, Rwanda
3Laboratory Department, Masaka Hospital, Rwanda
4Laboratory Department, Polyclinc Kanimba, Rwanda
5Department of Biomedical Laboratory Sciences, Kibogora Polytechnic, Rwanda
6Department of Biomedical Laboratory Sciences, Mount Kenya University, Kenya
- *Corresponding Author:
- Jean Baptiste Niyibizi
Department of Medical Laboratory Sciences
Mount Kenya University Rwanda, Kigali campus
E-mail: niyibizi3@gmail.com
Accepted on February 20, 2018
Citation: Nzeyimana Z, Nshimiyimana T, Nyumbayire JMV, et al. Assessment of intestinal parasites among children taking antiparasitic drugs at Ngoma primary school, Rwanda. J Parasit Dis Diagn Ther. 2018;3(1):1-5. doi: 10.4066/2591-7846.1000020
DOI: 10.4066/2591-7846.1000020
Visit for more related articles at Journal of Parasitic Diseases: Diagnosis and TherapyAbstract
Background: Intestinal parasitic infections are amongst the most common infections worldwide. There is increasing recognition that these parasites can impair the growth and development of children of all ages. Since 2009, Rwanda MOH has targeted to reduce prevalence of soil transmitted helminths in school aged children from 65% to 50% by 2012. Objectives: Our study aimed to assess intestinal parasites among Ngoma primary school children taking antiparasitic drugs (Albendazole and Mebendazole). The specific objectives of this study were to establish the most commonly encountered intestinal parasites in Ngoma primary school children and to determine intestinal parasite load among the infected children.
Methods: 120 stool samples, conveniently sampled, of Ngoma primary school children were examined for intestinal parasites. Slides were prepared directly for Wet mount in saline and iodine then microscopically examined. Finally, formalin-ether sedimentation techniques and Modified Wisconsin Sugar flotation method were used to concentrate stool samples for parasite identification and egg count respectively.
Results: Of the 120 children, 39 (32.5%) were found infected with one or more intestinal parasites. The prevalence of Giardia lamblia, Entamoeba coli, Entamoeba histolytica, Ascaris lumbricoides, hookworm, and Taenia species infections as determined by Formol ether concentration technique were 13.3%, 7.5%, 5.8%, 3.3%, 1.7%, and .8% respectively. On the other hand, the mean of Egg per gram of stool estimates of Ascaris lumbricoides, hookworm, and Taenia species as determined by modified Wisconsin Sugar flotation method were 11, 9, and 6 egg per gram (epg), respectively. Conclusion: Intestinal parasitic infections were prevalent in varying magnitude among Ngoma primary school children. G. lamblia, E. coli, and E. histolyica together contribute to the majority of intestinal parasites encountered and they represent 86% of all the intestinal parasitic infections recovered.
Keywords
Parasites, Infestations, Cysts, Trophozoite, Diarrhea, Amoebiasis, Gastrointestinal infections.
Introduction
Intestinal parasites are organisms that live in the gastrointestinal tract of animals, including humans and can cause morbidity and mortality [1]. The two main types of intestinal parasites are helminths and protozoa. Helminths are worms with many cells. In their adult form, helminths cannot multiply in the human body. Protozoa have only one cell, and can multiply inside the human body, which can allow serious infections to develop [2]. The parasites in the intestines are classified into two classes such as protozoa and helminths. Protozoa are single celled and includes Amoebae, flagellates, ciliates, and coccidia and microsporodia whereas helminths multicellular organisms which include Nemathelminthes and Platyhelminthes [3]. Intestinal parasites are usually transmitted when someone comes in contact with infected feces for example, through contaminated soil, food, or water [4]. Certain types remain in the intestines; others travel outside the intestines to invade other organs. Most tapeworms and roundworms develop in the human body and lay their eggs there. The eggs then pass out of the body through feces and can infest others [5].
The World Health Organization (WHO) estimates that 3.5 billion people worldwide are infested with some type of intestinal parasite, and as many as 450 million of them are sick as a result. Children are most frequently infected with these parasites [1]. Intestinal parasitic infections are amongst the most common infections worldwide. It is estimated that 3.5 billion people are affected by intestinal parasites, and that 450 million are ill as a result of these infections, with the majority being children [1]. Neglected tropical diseases (NTDs) are the most common infections of poor people worldwide. In southern Rwanda in 2001, it was reported that 55% of 2004 school aged children were infected with hookworm, Ascaris lumbricoides, or Trichuris trichiura [6]. There is increasing recognition that these parasites can impair the growth and development of children of all ages [6]. These infections are regarded as a serious public health problem, as they cause iron deficiency anemia, growth retardation in children and other physical and mental health problems [5]. Intestinal parasites in primary schools are a major public health problem in Rwanda. It is believed that in Rwanda, more than 75% children were infected by intestinal worms in 2007 [7]. Highest prevalence of neglected diseases is found in tropical and subtropical regions [5]. In industrialized countries, risk groups include male homosexuals, travelers and recent immigrants, and institutionalized populations [5]. Tapeworms, pinworms, and roundworms are among the most common helminths in the United States [5].
From 2006, the Rwanda MOH has organised a biennial mother and child health week and in 2007, MOH began to administer Albendazole/Mebendazole, or Praziquantel (in bilharziosis risk zone) to school children aged between 5 and 16 years [4]. Since 2009, Rwanda MOH has targeted to reduce prevalence of soil transmitted helminths in school aged children from 65% to 50% by 2012. This study aimed to assess intestinal parasitic infections among Ngoma primary school a children taking antiparasitic drugs (here is Albendazole). Despite efforts by the Rwanda MOH to reduce parasitic infections among primary school children, intestinal parasitic infections are still reported to be a major health problem among those children as evidenced by the more than 75% Rwandan children who were estimated to be infected by intestinal worms in 2007 [7]. More so, according to the Health Sector Strategic Plan of July 2009-June 2012, Rwanda MOH targeted to reduce prevalence of soil transmitted helminths in school aged children from 65% in 2009 to 50% by 2012 [8]. With this period of the strategic plan, evidently, the results were not as earlier anticipated. This study aimed to assess intestinal parasitic infections among Ngoma primary school children taking antiparasitic drugs (Albendazole/ Mebendazole) in Ngoma primary school located in Southern province, Huye district in order to decipher the most common intestinal parasites among Ngoma Primary School children taking antiparasitic drugs and also to determine the parasite load (parasite per gram of stool) among infected children of Ngoma primary school.
Methods
The study was carried out at Ngoma primary school which is located at the Southern province, Huye district, in Ngoma sector, 1.5 km from Huye town. Cross-sectional investigation was used to collect information concerning intestinal parasitic infections in Ngoma primary school. Ngoma Primary school (from 3rd to 5th year primary school students) children, aged between 8 and 14, taking antiparasitic drugs biennially administered were considered in this study. Eligible children were conveniently selected and samples from 120 children were tested for intestinal parasites. During sample collection and processing, each child was given a wide mouthed container with a wooden applicator stick and hygienic paper to collect required amount of fecal sample after explaining to them how and how much sample to be collected. Samples were labelled with child’s code number corresponding to his/her data sheet then transported directly to Gatagara high school laboratory for analysis.
For macroscopic examination of specimens, specific features were taken into account in order to ascertain accuracy for each specimen’s result. These include: the consistency of stool such as formed, soft, loose or watery; presence of blood and or mucus, presence of round worms, thread worms or tapeworm proglottids. After macroscopic examinations, the microscopic examination was carried out using two methods, which are wet mount preparation that were performed according to the Centres for Disease Control and Prevention (CDC) protocols (CDC, 2016). The second method was concentration technique in which the researchers used Formol-ether sedimentation technique to concentrate negative samples with wet mount method as described by CDC, 2016. Modified Wisconsin Sugar flotation method as described by Dr. Nolan in 2004 was used for egg count [9]. These results were recorded on the developed laboratory sheet. Data were analysed and presented in terms of percentages, tables, charts and figures generated using Microsoft excels. Results of mean average analysis, standard deviation were analyzed using SPSS version 20.
Ethical Consideration
This study was conducted after obtaining an informed consent from the school director and teachers of 3rd to 5th year primary school students of Ngoma Primary School, following the ethical approval given by Kigali Health Institute to carry out this research. The researchers clarified the purpose of the study and the participation of the children was voluntary. The identity of the children remained confidential, hence it was not exposed to the public.
Results
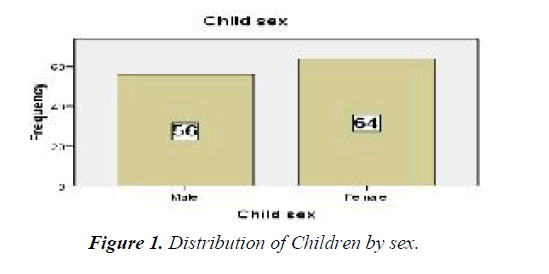
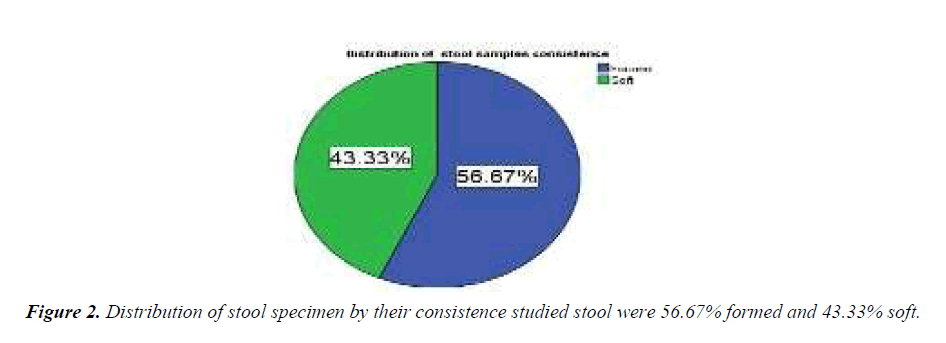
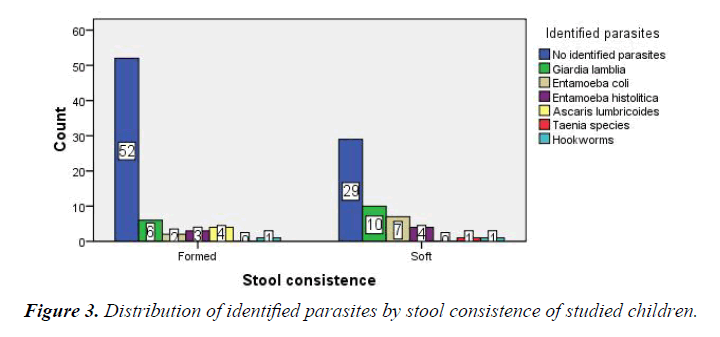
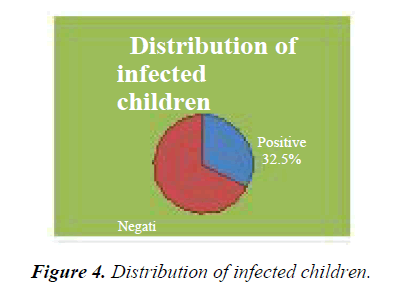
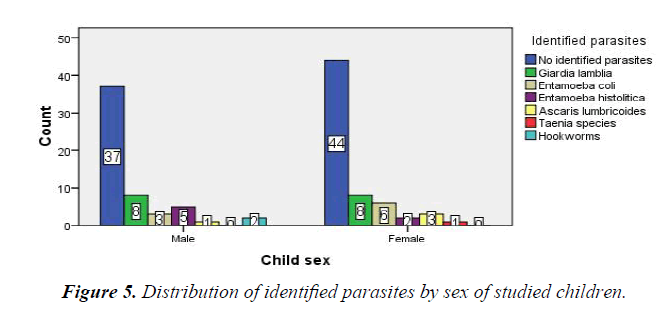
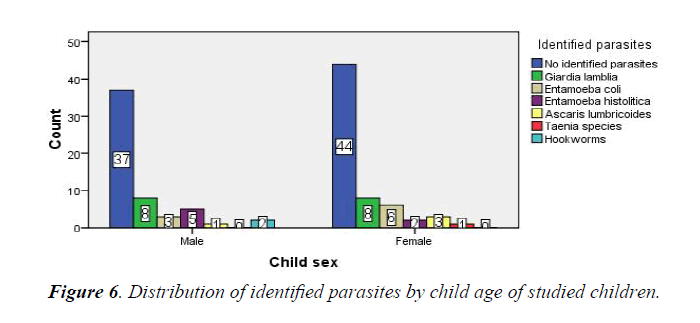
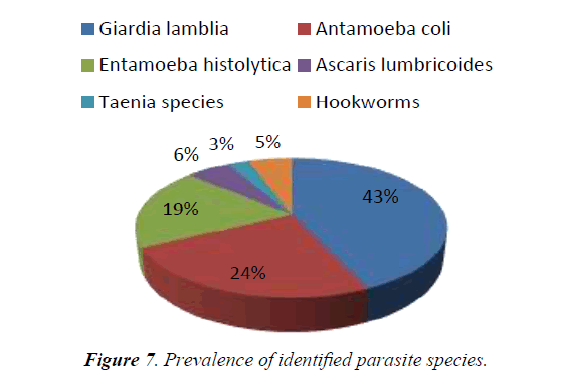
In Table 1 and Figure 1 respectively, represent age and sex distribution of the children enrolled and tested during the study. Less than half (Figure 2) of the tested children had soft stool from which a majority of parasites were recovered (Figure 3). Out of 120 examined children, 39 (32.5%) had intestinal parasitism (Figures 4-6). Of the 39 children who had parasite infections, 6 species (Table 2) of parasites were identified, with Giardia lamblia being the most common (13.3%) and Taenia spp the least (.8%) encountered species. Of the 6 identified species, intestinal protozoa represent 86% whereas the remaining represents the intestinal helminths (Figure 7). Table 3 shows the parasite load/ egg per gram (epg) of the 3 parasite species from which eggs were recoverable.
| Child age(years) | Frequency | Percent (%) | Cumulative Percent (%) |
|---|---|---|---|
| 8-11 | 73 | 60.8 | 60.8 |
| 12-14 | 47 | 39.2 | 100 |
| Total | 120 | 100 |
Table 1. Age distribution of the studied children
| Laboratory findings | Frequency | Percent (%) | Cumulative Percent |
|---|---|---|---|
| No identified parasites | 81 | 67.5 | 67.5 |
| Giardia lamblia | 16 | 13.3 | 80.8 |
| Entamoeba coli | 9 | 7.5 | 88.3 |
| Entamoeba histolitica | 7 | 5.8 | 94.2 |
| Ascaris lumbricoides | 4 | 3.3 | 97.5 |
| Taenia species | 1 | 0.8 | 98.3 |
| Hookworms | 2 | 1.7 | 100 |
| Total | 120 | 100 |
Table 2. Laboratory results of identified intestinal parasites in tested Ngoma primary school children.
Ascaris lumbricoides represented the highest epg (Mean of 11).
Our studied population aged between 8 and 14 years old. Studied ages were grouped into two groups, 8-11 and 12-14 representing respectively 60.8% (73) and 39.2% (39.2).
In 120 cases, 81 were not presenting any parasite and 39 presented any species of parasite identified being Giardia lamblia, Entamoeba coli, Entamoeba histolytica, Ascaris lumbricoides, Taenia species, or hookworms.3.5 Distribution of identified parasites by stool consistence of studied children.
Most identified parasitic stages were cystic and egg for protozoa and helminths respectively, as formed and soft feces are highly likely to contain these parasitic forms (CDC DPDx 2010). Soft stool presented more parasites than formed one.
In 64 counted females, 20 had any one of the intestinal parasites and 44 with no identified parasite whereas in 56 males, 19 had any one of the parasites and 37 with no identified parasite. Females presented more Entamoeba coli than males.
Giardia lamblia is the most prevalent intestinal parasite found in all studied ages. 12 years aged children present most children with no identified parasite.
• E. coli prevalent in 8 and 9 aged children.
• E. histolitica is mostly distributed in 10 and 11 aged children.
Comparison of Parasite Species Proportions
Giardia lamblia represents the highest proportion (43%) followed by Entamoeba coli (24%) and Entamoeba histolytica (19%). Giardia lamblia, Entamoeba coli and Entamoeba histolytica are intestinal protozoa which are mostly encountered in Ngoma Primary school they all represent 86% of identified intestinal parasites whereas Ascaris lumbricoides, Hookworms, and Taenia species which are intestinal helminths represent only 14%.
Results for egg count
The means of egg per gram of stool is as shown in Table 3 below.
| Identified helminths | Mean | N | Std. Deviation |
|---|---|---|---|
| Ascaris lumbricoides | 11.25 | 4 | 2.217 |
| Hookworms | 9.5 | 2 | 2.121 |
| Taenia species | 6 | 1 | . |
| Total | 10 | 7 | 2.646 |
Table 3. Results for egg count.
The above table shows that 7 children were found to have helminthe eggs in their stool, among them, 4 had Ascaris lumbricoides eggs with mean of 11 egg per gram of stool (EPG), 2 with 9 hookworm EPG and 1 with 6 Taenia species EPG.
Discussion
In this study was conducted to establish the most commonly encountered intestinal parasites in Ngoma primary school children, and to determine the parasite load among helminths infected children. The results from this study revealed that G. lamblia is the most prevalent (13.3%) intestinal parasitic infection among the children of Ngoma primary school. Along with E. coli (7.5%) and E. histolyica (5.8%), G. lamblia predominantly infects children aged 8-11 years, with much less infection seen among the older (12-14 years) children. These findings are comparable to those reported from an Indian study by Wani et al. The Indian study was conducted among school children of Srinager city. Wani et al., reported Ascaris lumbricoides as the most prevalent (28.4%) intestinal parasite with Giardia lamblia a distant third at 4.9%. Comparably a study in Kassala town (Sudan) reported a Giardia lamblia prevalence of 12.3% and Entamoeba histolytica .4%. In a Rwanda study that included 2400 children aged 2-20 years old with 93% being 5-10 years old, the overall intestinal prevalence was 55.9%. These findings were remarkably different from ours in that, hookworms constituted 44.5% of the parasites. As was variously explained hygiene is at the heart of all these glaring and unacceptably high prevalence rate. Whereas this study report mainly high parasite load (epg) of Ascaris lumbricoides (11 epg), Hookworms (9 epg), and Taenia species (6 epg) several other studies have reported high parasitic loads. The authors suggest that the major difference arises from sample size (120) which was estimated to be low compared to the one conducted by Kassala with 900 children as sample size and the Rwanda study by Kabatereine with a sample size of 2400 children. Whereas females appeared to have higher infection rates than male students, the present authors could not attribute this occurrence to any particular or specific reason. Increase Ascaris lumbricoides and Hookworm species parasite loads have also been equally reported among those age groups. Cyst and eggs were mainly recovered from children who had formed stool as expected (CDC DPDx 2010).
The present study reports that intestinal protozoa represent the highest prevalence (26.6%) in identified intestinal parasites. This can be attributed to the type of deworming drug (albendazole) administered which targets only intestinal helminths which have significantly decreased to 5.8% in the studied children as MOH targeted to reduce intestinal helminths from 65%to 50% [8-16]. This can be probably attributed to increased awareness to prevent intestinal parasites, studied low sample size and the town location of Ngoma Primary school. In the present study, authors also report that mean epg, burden of the cases is positively related with the infection rate, of 11 (below 200) is of light infections as WHO report of 2002. WHO reported that less than 200 epg represent light infections for hookworms whereas greater than 200 epg should be regarded as a potential danger. This can be attributed to the Rwanda MOH deworming program, and asymptomatic tested children.
Conclusion
Intestinal parasitic infections are still a major health problem among the children we studied.
G. lamblia, E. coli and E. histolyica together contribute to the majority of intestinal parasites encountered and they represent 86% of all the intestinal parasitic infections recovered. However, our findings seem to suggest that the MOH interventional strategies are playing a positive role as there seems to be a decline in prevalence of intestinal helminths. Because of what appears to be a decline in intestinal parasite prevalence, MOH should continue with the deworming exercise. However antiprotozoal drugs should be integrated for protozoa are prevailing. Laboratories need to be equipped with better stool concentration; both flotation and sedimentation techniques and personnel trained on how to use them. Hygiene practices need to be emphasized, particularly to the younger children. We would also recommend further studies using larger sample sizes and better diagnostic approaches.
Limitations of the Study
In the present research, due to lack of Zinc sulphate reagents, Zinc sulphate floatation technique was not carried out.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper as far as this work is concerned.
Acknowledgement
Authors kindly appreciate the contribution of University of Rwanda, former KHI administration, Osuwat Lawrence Obado, Rwanda Education Board and Ministry of education at large.
References
- Lynne SG. Classification of Human Parasites, Vectors, and Similar Organisms. Clinical Infectious Diseases. 1993;16:614-15.
- Curtis V, Cairncross S, Yonli R, et al. Review: Domestic hygiene and diarrhoea-pinpointing the problem. Tropical Medicine and International Health 2000;5:22-32.
- Madigan MT, Martinko JM, Parker J. Brock Biology of Microorganisms. Pearson Education Inc. 2006;947-948.
- Elmer WK. Colour Atlas and Textbook of Diagnostic Microbiolog. Lippencort 1997;1071-1162.
- Dawit A. Medical parasitology: Lecture notes Degree and Diploma Programs For Health Science Students 2004.
- Eleonor TB, Vicente YB, Winifreda U. Infection status of intestinal parasites in children living in residential institutions in Metro Manila, the Philippines. Korean J Parasitol. 2004;41:113-5.
- Beaver PC, Jung RC, Cupp EW. Clinical Parasitology. Lea and Febiger. 1984.
- Ministry of Health: Rwanda ministry of Health: Health Sector Strategic Plan July 2009-June 2012.
- Formalin-Ethyl Acetate Sedimentation and Zinc Sulfate Flotation Techniques for Detection of Intestinal Parasites. J Clinical Microbio. 1981;13:882-4
- https://www.cdc.gov/dpdx/diagnosticprocedures/stool/microexam.html
- Haddad CM. Imaging of parasitic disease. J Media Reviews. 299:2691-2.
- Kim BJ, Ock MS, Chung DI, et al. The intestinal parasite infection status of inhabitants in the Roxas city, the Philippines. Korean J Parasitol. 2003;41:113-5.
- Amal KM, Anthony RM. Neglected Tropical Diseases: Epidemiology and Global Burden. Tropical Medicine and Infectious Disease. 2017; 2:36; doi:10.3390/tropicalmed2030036
- http://www.theaccessproject.com/index.php/about/ntd/
- Ichhpujani RL, Bhatia R. Medical Parasitology. 2nd Ed Jaypee Bros, New Delhi, 1998.
- Abdelsafi AG, Mohammed AE. Prevalence of Intestinal Parasite Infection in Primary School Children in Elengaz Area, Khartoum, Sudan. Academic Research International. 2014; 5: 2223-53.