Research Article - Biomedical Research (2017) Volume 28, Issue 16
Analysis on risk factors of recurrence and metastasis of breast cancer after breast-conserving surgery for patients with breast cancer
Hai-Ping Xia1#, Shao-Rong Gao2#, Xin-Feng Zhang1, Fu-Xin Zhou1, Chang-Jiang Liu1, Song Chen1,Wei Ren1, Tao Ma1 and Zi-Yong Liu1*
1The First Department of Surgery, 404 Hospital of the Chinese People’s Liberation Army, Weihai, Shandong, PR China
2The Third Department of Chemotherapy, Weihai Municipal Hospital, Weihai, Shandong, PR China
#These two authors contributed equally to this work
- *Corresponding Author:
- Zi-Yong Liu
The First Department of Surgery
404 Hospital of the Chinese People’s Liberation Army, PR China
Accepted on July 13, 2017
Abstract
Objective: This study aimed to analyse the risk factors of the recurrence and metastasis of breast cancer after breast-conserving surgery.
Methods: There were 102 breast cancer patients who underwent breast surgery reservations in 404 Hospital of the Chinese People’s Liberation Army from January 2011 to December 2014. We had recorded these cases’ 5-y recurrence rate and transfer rate after 1-5 y follow-up and retrospectively analysed the clinical data (including age, tumor size, margin status, receptor status and lymph node metastasis, etc.). The aim of this study was to analyse and summarize the risk factors for breast cancer patients who underwent tumor recurrence and metastasis after breast surgery.
Results: The patients were followed up for one to five years. Their 5-y recurrence rate was 10.78% and the transfer rate was 8.82%. According to Cox proportional hazards regression model, breast cancer breast tumor recurrence risk factors include: tumor volume>2 cm, margin invasion positive, HER-2 receptor-positive, estrogen receptor-positive, lymph node metastasis and tumor stage III (HR=3.7, 5.3, 3.8, 5.5, 5.3, 3.7). Tumor metastasis risk factors include: tumor volume>2 cm, HER-2 receptor-positive, estrogen receptor-positive, lymph node metastasis and tumor stage III (HR=5.3, 3.4, 2.3, 4.6, and 2.9).
Conclusion: Breast cancer patients retained the breast after the tumor volume>2 cm, with cutting edge invasion, HER-2 and estrogen receptor-positive, patients with lymph node metastasis, and stage III is associated with postoperative tumor recurrence. If tumor volume>2 cm, HER-2 and estrogen receptorpositive, patients with lymph node metastasis and stage III are related to tumor metastasis after operation.
Keywords
Breast cancer, Breast surgery, Tumor recurrence, Tumor metastasis, Risk factors.
Introduction
As a common malignant tumor, breast cancer is mainly treated with surgery, postoperative radiotherapy and chemotherapy. In recent years, more and more patients would like to retain the breast besides a radical cure. In this case, breast conserving surgery has become more and more widely used on clinic [1]. Relevant results in recent years have showed that the tumor metastasis rate and survival rate of the patients treated with breast conserving surgery in stages I and II were like those of the patients receiving total mastectomy.
Moreover, the quality of life of patients treated with breast conserving surgery was better and their rate of local recurrence was higher than that of the patients undergoing total mastectomy [2,3]. Therefore, the analysis and summary on risk factors of the recurrence and metastasis of breast cancer after breast-conserving surgery has important necessary to provide clinical guidance for the selection of operation and predict recurrence and metastasis and prognosis. This study retrospectively analysed the clinical data of 102 cases with breast cancer that underwent breast conserving surgery in our department of general surgery from January 2011 to December 2014. The results were reported as follows.
Materials and Methods
General materials
102 cases at the age of 21-64 (50.5 ± 1.5) and received breast conserving surgery in our hospital department of general surgery were selected randomly from January 2011 to December 2014. TNM stage: 57 cases of stage I, 30 cases of stage II, 5 cases of stage III, and 10 cases were unknown. Among them, 18 cases were treated with local extensive resection and 84 cases underwent quadrant resection+axillary lymph node dissection.
Methods
Treatment status: Among the 102 cases, 37 patients received chemotherapy before operation and they were treated one time per week and 2-3 times continuously. The remaining 65 patients underwent surgical treatment, including extensive local excision of the tumor (16 cases), resection margins and tumor distance of 2-3 cm and reconstruction of breast shape after resection. In addition, there were 77 patients (75.5%) who received radiotherapy and chemotherapy after operation.
Follow up
102 breast cancer patients were followed up by telephone and outpatient review after operation for 1 to 5 y, (24.5 ± 10.5) months on average. The content of the follow-up included the patients’ local recurrence and distant metastasis followed by an analysis of the clinical data of the patients with tumor recurrence and metastasis, which named their age, tumor size, margin status (positive margin: the margin from the 5 mm memory in the tumor tissue), lymph node metastasis, human epidermal growth factor receptor-2 (HER-2) expression and so on
Statistical method
IBM SPSS 17 statistical software was used for data statistics and analysis. Cox proportional hazards regression analysis was used to analyse the risk factors. The Cox model was represented by hazard ratios with 95% confidence intervals and related P value. If P<0.05, the difference was statistically significant.
Results
General clinical features of patients
Among the 102 patients, 10 patients had ductal carcinoma in situ (9.8%) and 92 (90.20%) had invasive carcinomas. The tumor volume was less than 2 cm in 72 (70.59%) cases but more than 2 cm in 92 cases (29.41%). There were 18 cases (17.65%) of N0 with Lymph node metastasis stage, 14 cases (13.73%) of N1, 30 cases (29.41) of N2, 30 cases (29.41) of N3 and 10 cases (9.80%) of NX (Table 1).
| Variate | n | % |
|---|---|---|
| Tumor types | ||
| Ductal carcinoma in situ | 10 | 9.80 |
| Invasive carcinomas | 92 | 90.20 |
| Neoplasm staging | ||
| I | 57 | 55.88 |
| II | 30 | 29.41 |
| III | 5 | 4.90 |
| Unknown | 10 | 9.81 |
| Tumor volume | ||
| ≤ 2.0 cm | 72 | 70.59 |
| >2.0 cm | 30 | 29.41 |
| Lymph node metastasis staging | ||
| N0 | 18 | 17.65 |
| N1 | 14 | 13.73 |
| N2 | 30 | 29.41 |
| N3 | 30 | 29.41 |
| NX | 10 | 9.80 |
| Estrogen receptor status | ||
| Positive (P) | 79 | 77.45 |
| Negative (N) | 23 | 22.55 |
| HER2 receptor status | ||
| P | 42 | 41.18 |
| N | 60 | 58.82 |
| Chemotherapy | ||
| Yes | 77 | 75.49 |
| No | 25 | 24.51 |
| Radiotherapy | ||
| Yes | 62 | 60.78 |
| No | 40 | 39.22 |
| Hormone therapy | ||
| Yes | 56 | 54.90 |
| No | 46 | 45.10 |
| Marginal erosion | ||
| Yes | 70 | 68.63 |
| No | 32 | 31.37 |
Table 1. General clinical feature of patients.
Follow-up
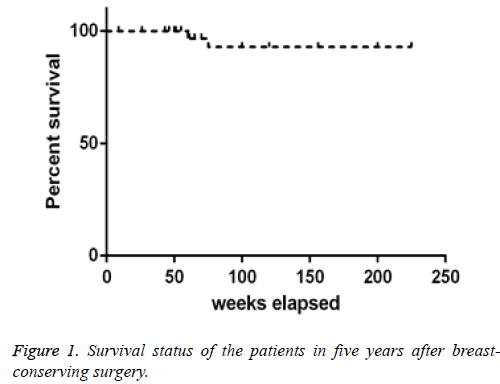
The 102 patients were followed up by one to five years and the results showed that 11 (10.78%) cases were recurred, 9 cases (8.82%) were transferred and the survival rate for 5 y was 96.08% (98/102). Among the 4 patients who died after the operation, 2 died because of breast cancer recurrence and metastasis and 2 died because of other diseases (Figure 1).
Relative factors of tumor recurrence and metastasis after breast-conserving surgery
The patients’ age, size of tumor, margin status, HER-2 status, postoperative radiotherapy and chemotherapy, lymph node status were included into single factor variable. We concluded that the related factors affecting tumor recurrence were the size of tumor, margin status, HER-2 status, postoperative radiotherapy and chemotherapy, lymph node status and the related factors affecting tumor metastasis were about age, size of tumor, HER-2 status, postoperative radiotherapy and chemotherapy, lymph node status (Table 2).
| Risk factors | Tumor recurrence | Tumor recurrence | ||||
|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | P | Hazard ratio | 95% CI | P | |
| Age | 0.7 | 0.21-2.52 | 0.619 | 0.7 | 0.25-2.13 | 0.56 |
| Tumor volume | 3.7 | 1.42-9.83 | 0.008 | 5.3 | 1.74-16.04 | 0.003 |
| Margin infiltrate | 5.3 | 1.74-16.04 | 0.003 | 1.9 | 0.80-4.65 | 0.144 |
| HER-2 receptor | 3.8 | 1.36-10.72 | 0.011 | 3.4 | 2.00-5.69 | 0.001 |
| Estrogen receptor | 5.5 | 2.96-10.23 | 0.001 | 2.3 | 1.13-4.78 | 0.022 |
| Lymphatic metastasis | 5.3 | 1.74-16.04 | 0.003 | 4.6 | 1.84-11.71 | 0.001 |
| Stages | 3.7 | 1.42-9.82 | 0.008 | 2.9 | 1.29-6.64 | 0.01 |
| Tumor type | 0.9 | 0.20-3.77 | 0.849 | 1.2 | 0.28-5.07 | 0.811 |
Table 2. Analysis on relative risk factors of recurrence and metastasis after breast-conserving surgery for patients with breast cancer after 5 y.
Discussion
In recent years, breast-conserving surgery has become the first option for patients who have breast cancer, especially for those in early stage. According to recent studies, there was no significant difference in the rate of distant metastasis and survival of breast-conserving surgery when compared with mastectomy.
In addition, women in modern society have a higher requirement for breast appearance and quality of life. However, there are also studies showing that compared with radical mastectomy, the recurrence rate of breast conserving surgery is higher after surgery. Therefore, on the basis of how to ensure complete resection of the tumor and keep the satisfactory appearance of the breast at the same time, how to take effective measures to control or reduce the rate of recurrence and metastasis have become the main focus of the current study [4]. Recent studies indicated that the clinical factors related to recurrence rate and metastasis rate of breast surgery included surgical indications, age of patients, size of patient’s tumor, lymph node metastasis, whether patients had a margin of infiltration, HER-2 receptor, estrogen receptor and other factors [5]. It was proposed in the study by Ali et al. [6] that the survival rate of metastasis-free overall survival rate of breast cancer patients were 95.4% and 99.1% after 5 y of breast conserving surgery. It should be noted that region tumor always may relapse in two or three years after the operation. At the same time, the results of multiple regression analysis displayed that risk factors affecting patients of local recurrence of tumor after breast conserving surgery included advanced age, lymph node metastasis, and HER-2 receptor positive. This study analysed and summarized the clinical data of 102 cases that underwent breast conserving surgery in our hospital. The data showed that the recurrence rate was 10.78%, metastasis rate was 8.82% and survival rate after 5 y was 96.08%. Cox proportional hazards regression analysis displayed that the independent risk factors affecting the recurrence of breast were the over 2 cm volume of tumor, margin invasion positive, HER-2 receptor positive, estrogen receptor positive, lymph node metastasis and tumor stage III (HR were 3.7, 5.3, 3.8, 5.5, 5.3, 3.7). This was because if the tumor became larger in size size, staged lately or associated with cutting edge invasion, it was quite possible to develop into intraductal carcinoma which has recurrence rate similar to that of invasive carcinoma. And sometimes it’s difficult to prevent its recurrence by radiotherapy and chemotherapy before or after the operation. To suppress tumor recurrence, a tip for this kind of breast cancer patients was to add the radiation and chemotherapy or hormone therapy after the breast conserving surgery [7]. In addition, the results of this study showed that the risk factors of tumor metastasis included over 2 cm tumor volume, HER-2 receptor positive, estrogen receptor positive, lymph node metastasis and tumor stage III (HR were 5.3, 3.4, 2.3, 4.6, 2.9). This study found no correlation between tumor recurrence and metastasis with patients’ age, which may be related to tumor staging, tumor size, and self-management in patients of different ages. There are many studies on the factors related to the local recurrence of breast cancer after mastectomy but few about postoperative metastasis for the moment [8]. Some reports demonstrated that relative factors of distant metastasis after breast conserving surgery included in age, diameter of the tumor [9-11]. By using the Cox proportional hazards regression model, this study illustrated that the factors related to tumor metastasis after breast conserving surgery were tumor volume, lymph node metastasis, HER-2 and estrogen receptor positive. Therefore, we should select suitable operation mode strictly according to the clinical indication. Usually, we would advise the patients with breast cancer in stages I and II to take breast conserving surgery according to the size of the tumor, the presence of lymph node metastasis, HER-2 and estrogen receptors. In summary, risk factors of breast tumor recurrence after breast conserving surgery contain tumor volume of over 2 cm, margin of invasion, HER-2 and estrogen receptor positive, lymph node metastasis and stage III. The related risk factors of tumor metastasis after surgery included tumor volume over 2 cm, HER-2, estrogen receptor positive, lymph node metastasis and stage III. It is recommended that postoperative chemoradiotherapy and hormone therapy should be used to inhibit and reduce recurrence and metastasis in patients of this kind
References
- Behm EC, Beckmann KR, Dahlstrom JE. Surgical margins and risk of locoregional recurrence in invasive breast cancer: an analysis of 10-year data from the Breast Cancer Treatment Quality Assurance Project. Breast 2013; 22: 839-844.
- Morrow M, Harris JR, Schnitt SJ. Surgical margins in lumpectomy for breast cancerdbigger is not better. N Engl J Med 2012; 367: 79-82.
- Miles RC, Gullerud RE, Lohse CM. Local recurrence after breast-conserving surgery: multivariable analysis of risk factors and the impact of young age. Ann Surg Oncol 2012; 19: 1153-1159.
- Kim K, Chie EK, Han W. Age, 40 years is an independent prognostic factor predicting inferior overall survival in patients treated with breast conservative therapy. Breast J 2011; 17: 75-78.
- Chung AP, Huynh K, Kidner T. Comparison of outcomes of breast conserving therapy in multifocal and unifocal invasive breast cancer. J Am Coll Surg 2012; 215: 137-146.
- Ali AN, Vapiwala N, Guo M. The impact of re-excision and residual disease on local recurrence after breast conservation treatment for patients with early stage breast cancer. Clin Breast Cancer 2011; 11: 400-405.
- van der Leij F, Elkhuizen PH, Bartelink H, van de Vijver MJ. Predictive factors for local recurrence in breast cancer. Semin Radiat Oncol 2012; 22: 100-107.
- Peltoniemi P, Huhtala H, Holli K, Pylkkänen L. Effect of surgeons caseload on the quality of surgery and breast cancer recurrence. Breast 2012; 21: 539-543.
- Vrijens F, Stordeur S, Beirens K. Effect of hospital volume on processes of care and 5-year survival after breast cancer: a population-based study on 25000 women. Breast 2012; 21: 261-266.
- In H, Bilimoria KY, Stewart AK, Wroblewski KE, Posner MC. Cancer recurrence: an important but missing variable in national cancer registries. Ann Surg Oncol 2014; 21: 1520-1529.
- Gooiker GA, van Gijn W, Post PN. A systematic review and meta-analysis of the volume-outcome relationship in the surgical treatment of breast cancer. Are breast cancer patients better off with a high volume provider? Eur J Surg Oncol 2010; 36: 27-35.