Research Article - Biomedical Research (2017) Volume 28, Issue 8
Analysis of recurrent oral ulcer in patients with or without food allergy
Xueyan Wang*, Xiaorong Li and Haiyun ShiDepartment of Allergy, Beijing Shijitan Hospital, Capital Medical University, PR China
- *Corresponding Author:
- Xueyan Wang
Department of Allergy, Beijing Shijitan Hospital
Capital Medical University, PR China
E-mail: wxysjtbtfy@sina.com
Accepted date: December 28, 2016
Abstract
Objective: This study was to investigate the relationship between recurrent oral ulcer and cow's milk allergy.
Data and Methods: The research collected 128 patients with recurrent oral ulcer that saw a doctor in the outpatient of our allergic reaction department from 2010 to 2015. All the patients joined this study with informed consents. The occurrence rate of the recurrent oral ulcer was calculated according to the detailed medical history and comprehensive laboratory test results, including serum specific IgE of food allergy, IgG test and oral food challenge test. Finally, a typical patient with recurrent oral ulcer was shown to strengthen the conclusion we got.
Results: 17 patients were directly related to food allergy and accounted for 13.3% of the total patients with RAU, with the ratio of male to female of 4.67:1. Among them, 6 were allergic to milk, with the ratio of male to female of 2:1. 1 was allergic to fish, 1 was allergic to soybean, and 2 were allergic to wheat. Among 17 patients, 2 showed ulcer symptoms on the day of treatment, 3 were in the early ulcer stage, 10 were in the ulcer stage, 2 were in the healing period.
Conclusion: Multiple food allergies can induce and aggravate recurrent oral ulcer. In addition, the patients in the ulcer stage have more ulcer symptoms than at early ulcer stage. We should make a detailed diagnosis and treatment from the perspective of food allergen in the treatment of recurrent oral ulcer.
Keywords
Food allergy, Recurrent oral ulcer, Serum specificity IgE, Milk allergy, Egg allergy
Introduction
Recurrent oral ulcer induced by food allergy was a kind of oral mucosal disease with unknown etiological factors and accounted for about 20% in the global morbidity, especially the patients less than 20 years accounted for the majority [1,2]. It was worth noting that according to a lot of literatures, there was a certain correlation between the occurrence of recurrent oral ulcer and quite a few food allergens. However, there were still studies with negative attitude [3]. Many factors such as the then living environment, food habits and work pressure perhaps jointly determined the situation that at that time, there was not much correlation between the condition of patients with recurrent oral ulcer and food allergy. However, so far, the research on recurrent oral ulcer induced by food allergy had increasingly attracted medical experts and scholars [4,5] and one simple reason was perhaps: patients could voluntarily get rid of the diet therapy in the treatment [6].
At present, the conventional method to treat current oral ulcer was mainly the local drug therapy in China. More applications were oral ulcer film with quite a few traditional Chinese medicine or western medicine components and conventional drug therapeutic schedules such as vitamins, trace elements, and levomisole and so on [7-9]. The above-mentioned therapeutic schedules suited symptoms in most cases and failed to make a treatment targeted for clear etiological factors. In addition, the schedules only aimed to ease severe pain due to skin and mucosa ulceration rather than solved essential problems. Therefore, it was very crucial to find out and confirm the real pathological factors of recurrent oral ulcer. Detailed and in-depth research could be made from quite a few aspects such as psychological factors, food allergen, vitamin deficiency, infectious substances and trauma [10-12].
The paper analyses and evaluates food allergy of patients with recurrent oral ulcer collected by our hospital and data about inspection and medical history from the perspective of food allergy. Among them, the paper comprehensively analyses serum specificity IgE, oral food challenge test results, allergic history, and treatment history and other aspects in order to further find out the relationship between food allergy and recurrent oral ulcer, and make treatment based on elimination diet method in the field of food allergy accompanied by simple antihistamine drug treatment to successfully treat symptoms and root causes. Finally, the paper shows in detail data about a typical patient with recurrent oral ulcer induced by milk among the 17 patients in order to highlight the importance of food allergy in treating recurrent oral ulcer.
Data and Methods
Clinical manifestation of recurrent oral ulcer [13]
At present, recurrent oral ulcer is mainly divided into three categories: minor oral ulcer (MiAU), major oral ulcer (MjAU), and herpetiform ulcer (HU).
Among them, MiAU accounts for 80% of the total incidence, mainly showing local sensitivity, discomfort and some tenderness or burning sensation before aphtha. Most patients have such symptoms. Ulceration generally covers the area of 2~4 mm2, and is with neat edge, blush of about 1 mm in width, soft base, concave shape in the middle, is covered with grayish yellow or light yellow and white fibrinous pseudomembrane, and brings increasing pain. There are about 1~5 ulcers each time. And ulceration easily occurs in the mucous membrane of non-keratin areas such as lips and cheek. MjAU, also called recurrent necrotizing mucosal inflammation, is similar to MiAU in incidence. But its ulceration covers bigger and deeper area and has 10~30 mm in diameters, reaching lower mucous membrane and even muscular layer. The tissues around the ulceration are swollen and slightly raised. Most of ulcers are neat and are with scars or defects after healing. HU is characterized by small ulcers, with the diameter of only 1~2 mm. However, there are dozens or more ulcers. They can be distributed in any parts of mucous membrane and integrate with the adjacent ulcers into a large ulcer. In addition, the peripheral mucous membrane is congestive, which is relative rare. The incidence is less than 20%.
Data about patients
The research collects 128 patients with recurrent oral ulcer that saw a doctor in our hospital from 2010 to 2015. All the patients joined this study with informed consents. The occurrence rate were calculated according to the detailed data of medical history and comprehensive laboratory test results including serum specificity IgE of food allergy, food IgG test and oral food challenge test, and were described in detail, the patients’ basic information and pathogenetic characteristics from several aspects such as the pathogenetic stage, type, starting time, ulceration healing time and food allergen.
Inclusion criteria
Patients included in the research first should meet the diagnostic criteria of recurrent oral ulcer including definition and clinical manifestations and then meet the following conditions: medical history >2 years, incidence >more than 3 times within a year, no drug treatment within the latest 2 weeks, no systemic diseases.
Analysis of diagnosis and treatment
Firstly, the paper analyzes in detail data about patients’ medical history, including drug allergic history, recurrent ulcer history, occupation, whether they contact chemical and radioactive substances or not, whether they often travel on business, work overtime at night and move house or not, whether they are with chronic lesions including gastritis, duodenal ulcer, sore throat, and maxillary sinus or not, whether they had allergic diseases in childhood or not, and whether their parents have allergic history or not.
The detailed medical history is the cornerstone to accurately diagnose any diseases, so the paper screens the patients with recurrent oral ulcer related to food allergy, sorts out the then data including oral ulceration’s type, size, stage, medical history, physical examination, allergen examination results, and oral challenge test results, and collects and confirms data: patients with recurrent oral ulcer induced by food allergy’ age range, sex ratio, food allergen category, first morbidity time, oral ulcer morbidity stage on the day of treatment, oral ulcer category, and drug treatment history and others.
Finally, the paper shows in detail data about a typical patient with recurrent oral ulcer induced by milk among the 17 patients in order to highlight the importance of food allergy in treating recurrent oral ulcer.
Therapeutic schedules
The paper analyzes the data about inspection and medical history from the perspective of food allergy. Among them, the paper comprehensively analyzes serum specificity IgE, oral food challenge test results, allergic history, and treatment history and other aspects in order to further find out the relationship between food allergy and recurrent oral ulcer, and make treatment based on elimination diet method in the field of food allergy accompanied by simple antihistamine drug treatment to successfully treat symptoms and root causes. Therefore, the paper suggests that all patients with recurrent oral ulcer induced by food allergy should make a two-week elimination diet schedule in allusion to their respective tested food allergens.
Results
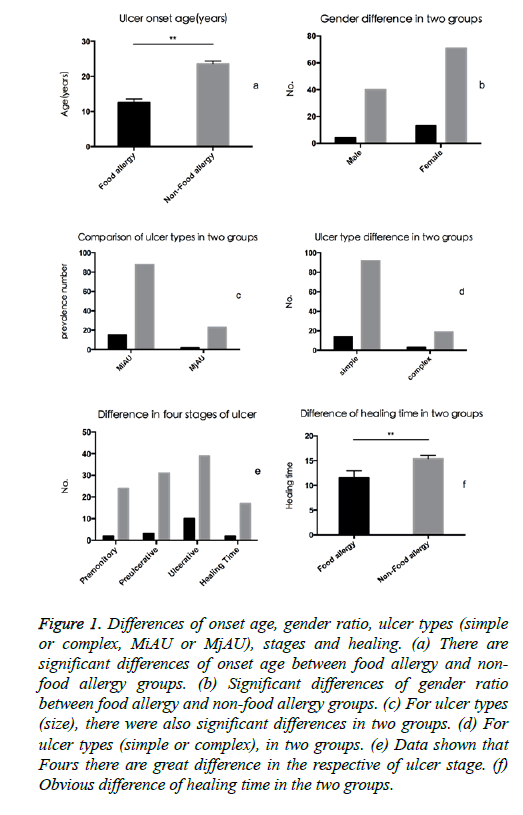
Among 68 patients with recurrent oral ulcer (RAU) that saw a doctor in our hospital from 2010 to 2015, 17 patients were directly related to food allergy and accounted for 25% of the total patients with RAU, with the ratio of male to female of 1:4.67 (4 male patients and 13 female patients) and the age of 4~22, that is, the average age of 12.5, history of oral ulcer of 1~7 years with the average years of 2.35 and course of disease of 3~21d. Among them, 6 patients were allergic to milk with the age of 4~18; 5 patients were allergic to eggs with the age of 11~20; 2 patients were allergic to seafood. 2 patients were allergic to wheat. 1 patient was allergic to fish. 1 patient was allergic to soybean. Among 17 patients, 2 patients showed ulcer symptoms on the day of treatment. 3 patients were in the early ulcer stage. 10 patients were in the ulcer stage. 2 patients were in the healing period (Table 1) [14-17]. According to the different information of the patients, the paper makes summary (Figure 1 and Table 2) [14-17].
| Group | Average age |
Gender | Stages of ROU | Types of ulcer | Classifi-cation | Average healing time(days) |
|---|---|---|---|---|---|---|
| Food allergy induced | 12.5 ± 4.5 | Male: 4 Female: 13 |
Prem.: 2 Preu.: 3 Ulcera.: 10 Heali.: 2 |
Simple: 14 Complex: 3 |
MiAU: 15 MjAU: 2 |
11.5 ± 6.1 |
| Not induced by food allergy | 23.6 ± 7.9 | Male: 40 Female: 71 |
Prem.: 24 Preu: 31 Ulcera.: 39 Heali.: 17 |
Simple: 92 Complex: 19 |
MiAU: 88 MjAU: 23 |
15.4 ± 7.2 |
| Prem.: Premonitory, Preu.: Preulcerative, Ulcera.: Ulcerative, Heali.: Healing. | ||||||
Table 1: Comparison between patients with food allergy and without food allergy.
| ID | Age (Years) Gender | First onset Age | RAU Stages | RAU Types | Classification | Previous Treatment | Food Allergen | Healing time |
|---|---|---|---|---|---|---|---|---|
| 1 | 26 male | 22 | Preulcerative | simple | MiAu | colchicine | Seafood | 10 |
| 2 | 42 female | 35 | Preulcerative | complex | MiAu | vitamin B12 | fish | 17 |
| 3 | 28 female | 25 | premonitory | complex | MiAu | Prednisone | cows milk | 21 |
| 4 | 27 male | 25 | ulcerative | simple | MiAu | Prednisone | eggs | 12 |
| 5 | 42 male | 38 | healing | complex | MiAu | vitamin B2 | eggs | 14 |
| 6 | 34 male | 30 | premonitory | complex | MiAu | vitamin B2 | soybean | 22 |
| 7 | 45 male | 38 | ulcerative | complex | MiAu | vitamin B2 | wheat flour | 28 |
| 8 | 41 female | 38 | premonitory | complex | MiAu | vitamin B12 | wheat flour | 30 |
| 9 | 48 male | 46 | premonitory | simple | MiAu | vitamin B12 | soybean, fish | 12 |
| 10 | 29 female | 26 | ulcerative | simple | MiAu | colchicine | eggs, cows milk | 10 |
| 11 | 30 female | 28 | ulcerative | simple | MiAu | cyclosporine A | cows milk | 14 |
| 12 | 32 female | 30 | healing | simple | MiAu | vitamin B2 | cows milk | 10 |
Table 2: Basic information of the CMA patients.
Figure 1: Differences of onset age, gender ratio, ulcer types (simple or complex, MiAU or MjAU), stages and healing. (a) There are significant differences of onset age between food allergy and nonfood allergy groups. (b) Significant differences of gender ratio between food allergy and non-food allergy groups. (c) For ulcer types (size), there were also significant differences in two groups. (d) For ulcer types (simple or complex), in two groups. (e) Data shown that Fours there are great difference in the respective of ulcer stage. (f) Obvious difference of healing time in the two groups.
Typical case analysis: recurrent oral ulcer induced by milk allergy
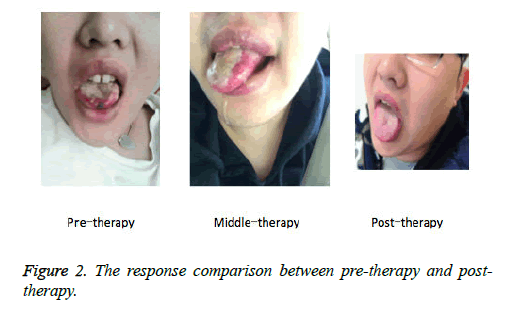
An 18 year old man saw a doctor in our allergic reaction department. The patient had found that his tongue and lips were often with oral ulcer about 2 years ago. At first, he felt discomfort due to the situation that his tongue seemed pricked by a needle and led to burning sensation; after 2 days, his condition deteriorated. He had quite a few small ulcers (with the diameter of 1~2 mm) in his mouth. The most serious situation was what seen in the picture before treatment: part of tissues had become necrotic and black in the tip of the tongue.
The patient received the Behcet syndrome treatment and took tripterygium glycosides for nearly 2 weeks, but his clinical symptoms failed to be improved. According to the collected data about medical history, the patient often ate a large number of dairy products including milk, cheese, and yogurt and others. This provided a clue for us. He perhaps became allergic to milk; after all, he ate a large number of milk and related dairy products for a long time. Therefore, we tried to screen common allergens including milk and related dairy products for the patient and found that his serum-milk specificity IgE and IgG slightly rose. At the same time, his specificity IgE of rice, wheat, egg, shrimp, and crab and others showed negative. In addition, he received 15 ml milk oral challenge test and felt that the tongue was painful. His lips became pale and congestive points gradually occurred in the tip of the tongue. Considering that the patient had obviously showed food allergic reaction and would suffer severe allergic shock if he ate more milk, we determined to give up the further test after he ate milk of 15 m. The results of blood routine examination including alanine aminotransferase level (49 mmol/L), total carbon dioxide content (28 mmol/L), triglyceride (1.75 mmol/L), serum apolipoprotein (1.85 g/L), lipoprotein (a) (0.30 g/L), and glycosylated serum protein (11.3%) were normal. We suggested that after seeing a doctor in our allergic reaction department, the patients should refuse to eat milk and related dairy products for 14 days, took ebastine for 7 days (10 mg/piece, 1 piece/day). Ebastine was mainly used to avoid the situation that the patient perhaps suffered other allergic reactions in the process of avoiding milk after eating milk for a long time. The follow-up period was 6 months. During the period, the patient did not suffer recurrent oral ulcer once again. The response comparison between pre-therapy and posttherapy, the patients suffered obviously different oral ulcer symptoms, as shown in Figure 2.
Discussion
Oral ulcer is the most common in oral mucosal diseases. Common cold, indigestion, mental tension, and depression and others occur occasionally. Oral ulcer easily occurs in lips, cheek, and lingual margin and others and any parts of mucous membrane, but it rarely occurs in attached gingiva and hard palate with completely keratinization. It mainly attacked the 10~20-year-old groups and generally could self-heal within 10 days. But if it often occurred or rises here and subsides there, it was called recurrent oral ulcer [18].
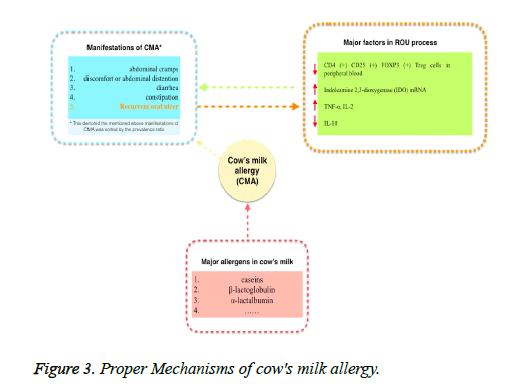
The reduction in the cell number of CD4 (+) CD25 (+) Foxp3 (+) Treg at the molecular level and peripheral blood would increase the prevalence rate of recurrent oral ulcer. In addition, indolamine 2, 3-dioxygenase mRNA played an important role in protecting patients with recurrent oral ulcer [19]. What’s more, as ulcer developed, TNF-αand IL-2 level rose and IL-10 level trended to be normal. There were many different allergies in milk. And casein, β-milk protein and α-milk protein were the most common allergens. In most cases, milk allergy was caused by the above 3 allergens [20,21], possible CMA mechanism has been shown in Figure 3. More mechanism or an unclear antibody or a factor needs to be investigated in detail.
The paper comprehensively analyses the relationship between food allergy and recurrent oral ulcer from the perspective of food allergy and makes treatment based on elimination diet method in the field of food allergy accompanied by simple antihistamine drug treatment to successfully treat symptoms and root causes. At the same time, the paper shows in detail data about a typical patient with recurrent oral ulcer induced by milk in order to further highlight the importance of food allergy in treating recurrent oral ulcer.
References
- Hamedi S, Sadeghpour O, Shamsardekani MR. The Most Common Herbs to Cure the Most Common Oral Disease: Stomatitis Recurrent Oral Ulcer (RAU). Iran Red Crescent Med J 2016; 18.
- Zhong L, Huang D, Wang H. Investigation and analysis of the incidence of recurrent oral ulcer in Xinjiang medical students. J Xinjiang Med Univ 2014.
- Zwiri AM. Anxiety, Depression and Quality of Life among Patients with Recurrent Aphthous Ulcers. J Contemp Dent Pract 2015; 16: 112-117.
- Wang T, Cheng F, Ren H, Qiu C, Zhau C, Chen Y. Clinical observation of recurrent oral ulcer of heat accumulation in the heart and spleen treated with acupoint injection and fire needling therapy. Zhongguo Zhen Jiu 2016: 5-6.
- Ju-WL. Study on the relationship between the trace elements,immune indexes and recurrent oral ulcer. J Hain Med Univ 2016.
- Hay KD, Reade PC. The use of an elimination diet in the treatment of recurrent aphthous ulceration of the oral cavity. Oral Surg Oral Med Oral Pathol 1984; 57: 504-507.
- Li Y. Clinical observation of combined Chinese and western medicine on treatment of recurrent oral ulcer. Chin J Traum Disab Med 2016; 9-10.
- Wang L. Treatment of levamisole combined with vitamin B12 on the clinical effect of the treatment of recurrent oral ulcer. Chin J Prim Med and Pharm 2016; 23.
- Liu A. Stomatitis sprays and rehabilitation new oral liquid for the treatment of oral ulcer. Chin J Mod Drug Appl 2016; 10: 175-176.
- Karthikeyan P, Aswath N. Stress as an etiologic co-factor in recurrent aphthous ulcers and oral lichen planus. J Oral Sci 2016; 58: 237-240.
- Baburizza MM, Maldonado EA, Núñez HO. OI0302 Helicobacter pylori: a risk factor for recurrent oral stomatitis? Oral Surg Oral Med Oral Pathol & Oral Radiol 2014; 117: e364.
- Vaillant L, Samimi M. Aphthous ulcers and oral ulcerations. Presse Med 2016; 45: 215-226.
- Yu H, Zheng W. Human leukocyte antigen (HLA) in the role of recurrent oral ulcer. Int J Oral Sci 1986.
- Rogers RS. Recurrent aphthous stomatitis: clinical characteristics and evidence for an immunopathogenesis. J Invest Dermatol 1977; 69: 499-509.
- Cui RZ, Bruce AJ, Rogers RS. Recurrent aphthous stomatitis. Clin Dermatol 2016; 34: 475-481.
- Jorizzo JL, Taylor RS, Schmalstieg FC, Solomon AR, Daniels JC. Complex aphthosis: a forme fruste of Behçet's syndrome? J Am Acad Dermatol 1985; 13: 80-84.
- Stanley HR. Aphthous lesions. Oral Surg Oral Med Oral Pathol 1972; 33: 407-416.
- Liang L, Lu M, Du M. Clinical effect of combining traditional Chinese and western medicine on the treatment of recurrent oral ulcer in children. J Clin Stomatol 2016; 11: 670-672.
- Lewkowicz N, Lewkowicz P, Dzitko K, Kur B, Tarkowski M. Dysfunction of CD4+CD25high T regulatory cells in patients with recurrent aphthous stomatitis. J Oral Pathol Med 2008; 37: 454-461.
- Bazrafshani MR, Hajeer AH, Ollier WE, Thornhill MH. Recurrent aphthous stomatitis and gene polymorphisms for the inflammatory markers TNF-alpha, TNF-beta and the vitamin D receptor: no association detected. Oral Dis 2002; 8: 303-307.
- Wei XF, Gao WX, Xiao-Li LU. Detection of IL-2 and T suppressor cell in patients with recurrent oral ulcer. J Jilin University 2005.