Research Article - Biomedical Research (2017) Volume 28, Issue 9
An innovative method to analyse the range of border mandibular movements using 3D electromagnetic articulography (AG501) and MATLAB
Ramon Fuentes1, Alain Arias1,2, Diego Saravia1,2,3, María Florencia Lezcano4, Fernando Jose Dias11Research Centre in Dental Sciences (CICO), Dental School, Universidad de La Frontera, Temuco, Chile
2Master Program on Dentistry, Dental School, Universidad de La Frontera, Temuco, Chile
3Universidad Adventista de Chile, Chillan, Chile
4Facultad de Ingenieria, Universidad Nacional de Entre Ríos, Entre Ríos, Argentina
Accepted date: March 06, 2017
Abstract
Objective: Mandibular movements have been investigated for decades in dentistry to diagnose problems related to the masticatory system and temporomandibular joint. This study proposes a novel method for analysing the border movements of the mandible using 3D electromagnetic articulography and scripts developed in MATLAB software, which has the advantages of free and accurate assessment of movements in three dimensions from different angles.
Methods: Mandibular border movements of six patients were recorded using a magnetic articulograph AG501 with 5 sensors (4 static and 1 dynamic) in the protocols: 1. maximum mouth opening associated with noncontact laterality movements; 2. border movement in the frontal plane; and 3. border movement in the sagittal plane.
Results: The means of the parameters evaluated were 39.9 ± 4.7 mm for mouth opening (displacement on the vertical axis); 61.6 ± 6.5 mm for opening along the three-dimensional trajectory; 11.3 ± 2.1 mm and 11.6 ± 2.5 mm for displacement of non-contacting right and left laterality, respectively; (Posselt’s envelope of motion-frontal view) 481.5 ± 110 mm2 frontal border movement polygon area; and 65.3 ± 31.6 mm2 sagittal border movement polygon area (Posselt’s envelope of motion-sagittal view).
Conclusion: The method for analysing border mandibular movement proposed in this study using EMA AG501 and MATLAB scripts generate graphical data similar to classic studies and provided high precision data in a systematic, easy and intuitive way, allowing for further analysis with patients in different clinical conditions as well as the possibility of association with different analysis modalities.
Keywords
Mandibular border movements, Electromagnetic articulograph, MATLAB scripts
Introduction
The limitations and changes of mandibular movements normally generated by traumatism, occlusal and articular imbalances, anatomical, psychological, neuromuscular factors, orthognatic surgery and dental infections, combined with clinical signs and symptoms, such as muscle or joint pain, tenderness, movement restriction and joint noises may indicate diseases related to Temporomandibular Joint (TMJ) [1-7].
For decades the recording of mandibular movements analysed jaw movements in terms of their geometry [8]. These complex movements occurs in three dimensions, however the classic studies, due to available technology, described these movement in one plane (2D), the definition and description of more refined in three-dimensional analyses allows for a more accurate diagnosis, better and more personalized treatments [9].
In recent years, the technological improvement of the position tracking techniques has allowed for recording of the kinematics of the articulations with a high temporal resolution as well as calculating their positions and velocities [10].
The Electromagnetic Articulography (EMA) is capable of measuring movements with fine spatial and temporal resolution, providing useful articulatory data. The position of the receiver coil is detected in the EMA device on the basis of a field function representing the spatial pattern of the magnetic field in relation to the relative positions of the transmitter and receiver coils [11-13]. This method represents a safe, non-invasive and accurate method for tracking human movements [10].
AG500 (Carstens Medizinelectronik, Lenglern, Germany) is currently one of the most developed three-dimensional (3D)- EMA systems. This device represents an evolution of its two-dimensional (2D) predecessors (Carstens AG100 and AG200), does not require a heavy restraining head and provides motion tracking in five degrees of freedom. The 3D-EMA produces smaller measurement errors across a larger range of sensor positions and orientations compared to 2D-EMA, providing an unprecedented level of access to the most complex movements [10,14,15].
In recent years, with the evolution of EMA systems, the measurement of a large number of functions has been achieved in the three planes and in real time, which is related to tongue-mandible movements [9].
The interpretation of mandibular movements data obtained using EMA devices is not an easy task because no software can perform a simple, reproducible and understandable analysis of the data generated by EMA and deliver reliable clinical data.
The aim of this study is to present and describe an innovative method for analysing the trajectories, amplitudes and areas of mandibular movements using the latest 3D electromagnetic articulograph, Carstens, AG501 (Germany), and its software. The use of MATLAB to process the obtained data allowed for a broader, intuitive, understandable and rapid analysis of the results.
Methods
Electromagnetic articulograph AG501 description
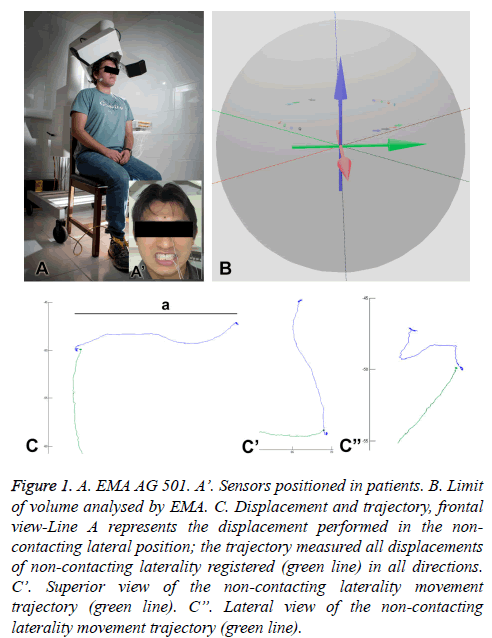
EMA AG501 (Carstens, Germany) (Figure 1A) has nine transmitter coils that emit magnetic fields to collect movement data in 3 dimensions (3D) and at multiple points, enabling realtime measurement of the structure movements connected to the sensors in a spherical volume of 0.014 m3 (r=15 cm, Figure 1B). The device software configures the data analysis, and the user can access the data obtained in different regions, such as the tongue, palate, mouth, incisors and skin [9]. The Electromagnetic Articulograph has been certified by the Federal Communications Commission (independent U.S. government agency) as a low power communication device transmitter that uses electromagnetic fields with a frequency range of 7.5 to 13.75 KHz. This range is lower than the frequency range of devices with radio transmission, such as cell phones (10 MHz a 300 GHz) [16].
Figure 1: A. EMA AG 501. A’. Sensors positioned in patients. B. Limit of volume analysed by EMA. C. Displacement and trajectory, frontal view-Line A represents the displacement performed in the non-contacting lateral position; the trajectory measured all displacements of non-contacting laterality registered (green line) in all directions. C’. Superior view of the non-contacting laterality movement trajectory (green line). C”. Lateral view of the non-contacting laterality movement trajectory (green line).
Preparation for analysis
The procedures performed on patients in this study were previously evaluated and approved by the Universidad de La Frontera ethics committee (Approval number 069/15) according to international testing standards in humans.
The movement recording session was initiated by the application of a questionnaire to collect information about possible problems with mandibular movement, problems associated with the oral cavity, and health and oral care. Later, a clinical evaluation was performed to evaluate the presence/ absence of teeth, overbite and overjet values, right and left molar and canine classes, amplitude of mandibular moves and presence of sensitivity or changes for the TMJ or associated muscles.
The sensors are positioned on the patient and fixed to the patient with biologically compatible glue (Epiglu®, Meyer Haake, Germany). The sensors are positioned at the following anatomical points (Figure 1A): 1-Right mastoid process (reference sensor); 2-Left mastoid process (reference sensor); 3-Glabella (reference sensor); 4-Upper incisor (between the two upper central incisors) (reference sensor); and 5-Lower incisor (between the two lower central incisors) (movement sensor). The coil system is lowered to 2 cm from the top of the patient’s head. The patient is requested to look to the front and adopt a straight head position.
In the “HEAD CORRECTION” process, reference sensors are needed so the EMA could interpret the relative location for the movement sensors. In this case, the reference sensors are connected to channels 1, 2, 3 and 4 and the movement sensor is connected 5. This procedure is performed with the patient in the orthostatic position and aims to eliminate the interference related to the head and neck movements that are not of interest in the study.
Protocols of mandibular movements
Three different protocols of mandibular movements were record and later analysed in the frontal, sagittal and horizontal planes of 6 patients.
Protocol 1: The maximum mouth opening associated with right and left noncontact side movements. Initially, the patient was instructed to perform the maximum opening movement following the lateral right and left noncontact movements. All of these movements were performed starting from the Maximum Intercuspation Position (MIP), and they were repeated three times in different recordings.
Protocol 2: Border movement in the frontal plane “Posselt’s envelope of motion-frontal view” [17]. This protocol starts instructing the maximum right lateral contact movement; then, from this point, the patient performs the right maximum border aperture. Subsequently, the patient repeats the same moves to the left side. The movements of the right and left side are performed starting from the MIP, and they are repeated three times in different registers.
Protocol 3: Border movement in the sagittal plane “Posselt’s envelope of motion-sagittal view” [17]. Starting from MIP, the patient is instructed to move the mandible to the maximum protrusion position, passing through the edge-to-edge incisal position. From that point, the patient performs the maximum mouth opening in protrusion. The second movement of this protocol also begins from MIP to maximum mandibular retrusion, which is followed by maximum mouth opening in retrusion. These movements are repeated three times in different records.
The experiment was conducted in the “Oral Physiology Laboratory” of the Research Centre in Dental Sciences (CICO), Dental School at the Universidad de La Frontera (Temuco, Chile).
Data analysis
All recorded data were properly labelled and transferred from the AG501 device to another computer on which data processing was performed. To analyse the movements, custom MATLAB scripts were used. MATLAB is a multi-paradigm numerical computing environment that is widely used for scientific research. It is used for machine learning, signal processing, image processing, computer vision, communications, control design and other functions (The MathWorks Inc., USA). The scripts provide visualization of recorded trajectories in all spatial planes, and the numerical value of the distances, ranges and areas of interest in a simple, intelligible, objective way.
The movements data obtained from analysis of the patients are presented in tables. From these data, the means and Standard Deviations (SD) for analysing the data variation between patients and repetitions for the same person of the movements were obtained.
In the analysis of movements’ data on the displacement, trajectory and area were obtained. The difference between the displacement and trajectory (Figure 1C-frontal view, C’- superior view, and C”-lateral view) is that only the offset value in one normalized axis is considered in the first case, any other inclinations were not considered (line a). Additionally, in the second case, movement in any axis and direction is considered (green line).
Results
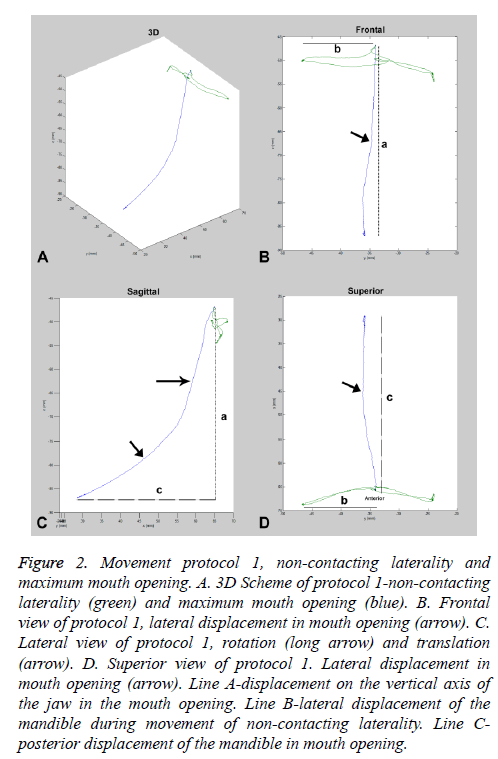
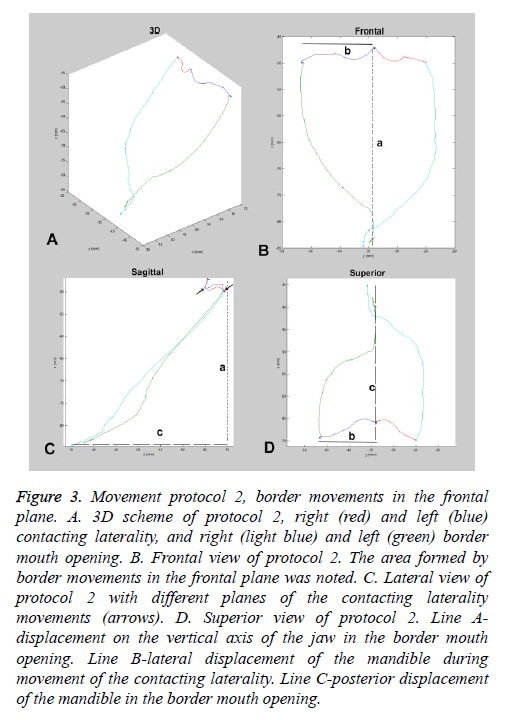
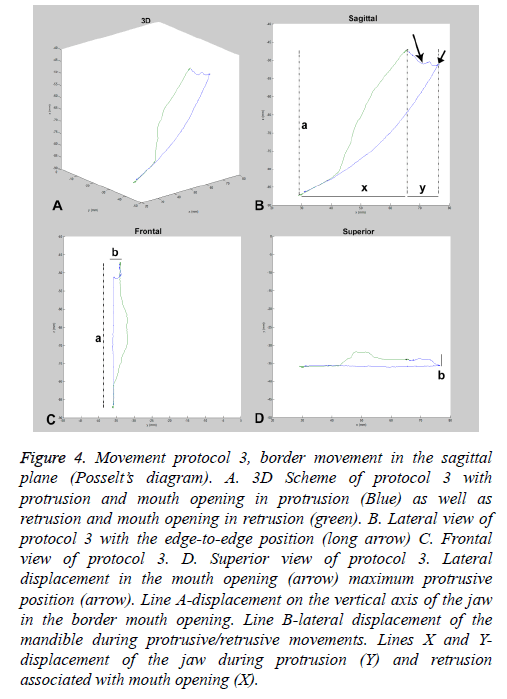
To analyse the proposed movements, the MATLAB software generates 3D graphics, which represent the trajectory obtained using EMA AG501 (Figures 2A, 3A and 4A). These graphics allow free viewing at different angles with the use of a movement tool. To standardize the analysis of trajectories, images in standard views in the frontal, lateral (or sagittal) and horizontal planes were obtained.
Figure 2: Movement protocol 1, non-contacting laterality and maximum mouth opening. A. 3D Scheme of protocol 1-non-contacting laterality (green) and maximum mouth opening (blue). B. Frontal view of protocol 1, lateral displacement in mouth opening (arrow). C. Lateral view of protocol 1, rotation (long arrow) and translation (arrow). D. Superior view of protocol 1. Lateral displacement in mouth opening (arrow). Line A-displacement on the vertical axis of the jaw in the mouth opening. Line B-lateral displacement of the mandible during movement of non-contacting laterality. Line C-posterior displacement of the mandible in mouth opening.
Figure 3: Movement protocol 2, border movements in the frontal plane. A. 3D scheme of protocol 2, right (red) and left (blue) contacting laterality, and right (light blue) and left (green) border mouth opening. B. Frontal view of protocol 2. The area formed by border movements in the frontal plane was noted. C. Lateral view of protocol 2 with different planes of the contacting laterality movements (arrows). D. Superior view of protocol 2. Line A-displacement on the vertical axis of the jaw in the border mouth opening. Line B-lateral displacement of the mandible during movement of the contacting laterality. Line C-posterior displacement of the mandible in the border mouth opening.
Figure 4: Movement protocol 3, border movement in the sagittal plane (Posselt’s diagram). A. 3D Scheme of protocol 3 with protrusion and mouth opening in protrusion (Blue) as well as retrusion and mouth opening in retrusion (green). B. Lateral view of protocol 3 with the edge-to-edge position (long arrow) C. Frontal view of protocol 3. D. Superior view of protocol 3. Lateral displacement in the mouth opening (arrow) maximum protrusive position (arrow). Line A-displacement on the vertical axis of the jaw in the border mouth opening. Line B-lateral displacement of the mandible during protrusive/retrusive movements. Lines X and Y-displacement of the jaw during protrusion (Y) and retrusion associated with mouth opening (X).
Protocol 1-Maximum mouth opening and non-contact laterality
This protocol assessed both the maximum mouth opening (blue) and right/left laterality non-contacting (green) starting from MIP. In this analysis, the frontal view (Figure 2B) and trajectory of each movement were observed with the possibility of evaluating lateral deviations (arrow) in the mouth opening and/or an abnormality in the laterality non-contacting movement. In the lateral view (Figure 2C), for the different planes in which they may occur, laterality and mouth opening for rearward movement of the jaw during the opening phases were observed (rotation-longer arrow and translation-arrow), and it is possible to measure this detachment. In the superior view (Figure 2D), it is also possible to note deviations from the trajectories of these movements as well as the different levels at which it occurs. In this case, the anteroposterior point of the mouth opening is offset to the side (arrow).
The values evaluated in this protocol were the mouth opening displacement; mouth opening trajectory and lateral right and left no-contact displacement were presented in Table 1.
| Patient | Rep. | Open. | Op. Track | Right lat. | Left lat. | Mean ± SD | |||
|---|---|---|---|---|---|---|---|---|---|
| Open. | Op. Track | Right lat. | Left lat. | ||||||
| 1 | 1 | 37.9 | 51.7 | 9.6 | 12.4 | 38.4 ± 0.9 | 54.1 ± 2.6 | 9.5 ± 0.3 | 12.5 ± 0.1 |
| 2 | 37.9 | 53.8 | 9.2 | 12.4 | |||||
| 3 | 39.3 | 56.8 | 9.8 | 12.6 | |||||
| 2 | 1 | 40.4 | 73.5 | 12.8 | 10.1 | 40.2 ± 0.6 | 72.7 ± 1.2 | 13 ± 0.2 | 10.3 ± 0.1 |
| 2 | 40.8 | 73.3 | 13.1 | 10.4 | |||||
| 3 | 39.6 | 71.3 | 13 | 10.4 | |||||
| 3 | 1 | 35.9 | 64 | 8.2 | 10.2 | 35.9 ± 0.1 | 62.6 ± 1.5 | 8.2 ± 0.1 | 9.7 ± 0.5 |
| 2 | 36 | 62.9 | 8.3 | 9.5 | |||||
| 3 | 35.8 | 61 | 8.1 | 9.4 | |||||
| 4 | 1 | 41 | 60.2 | 13.3 | 12 | 41.2 ± 0.6 | 58.4 ± 1.7 | 13.1 ± 0.21 | 12 ± 0.1 |
| 2 | 40.7 | 58.1 | 13 | 11.9 | |||||
| 3 | 41.8 | 57 | 12.9 | 12 | |||||
| 5 | 1 | 34.1 | 52.9 | 13.5 | 16.4 | 35 ± 0.9 | 57 ± 3.9 | 13.7 ± 0.3 | 16.3 ± 0.1 |
| 2 | 34.9 | 60.8 | 14 | 16.3 | |||||
| 3 | 36 | 57.3 | 13.7 | 16.2 | |||||
| 6 | 1 | 50.1 | 66.6 | 10.4 | 9.2 | 48.7 ± 1.3 | 64.6 ± 1.8 | 10.2 ± 0.2 | 9 ± 0.4 |
| 2 | 48.1 | 63.5 | 10.4 | 9.2 | |||||
| 3 | 47.8 | 63.6 | 10 | 8.5 | |||||
| Mean±SD | 39.9± 4.7 | 61.6± 6.5 | 11.3± 2.1 | 11.6± 2.5 | |||||
Table 1: Protocol 1 data, Mouth opening and non-contact laterality.
Mouth opening-To evaluate this parameter was considered only the displacement of the mandible in the vertical axis. The recordings from 6 patients in 3 repetitions showed values from 34.1 to 50.1 mm and a mean and SD of 39.9 ± 4.7 mm. However, in terms of the evaluation of only repetitions for the same patient, the SD value ranged from 0.1 to 1.3 mm.
Opening trajectory-For this parameter, the entire mouth opening 3D trajectory was considered. The recorded values ranged from 51.7 to 73.5 mm, with a mean and SD of 61.6 ± 6.5 mm. In assessing the repetition of the same patient, the values of the standard deviations were between 1.2 and 3.9 mm.
Right and left non-contacting laterality-This parameter evaluated the displacement on the horizontal axis for each side. The right lateral movement ranged from 8.1 to 14 mm and left handedness from 8.5 to 16.4 mm; the mean and SD in this case was 11.3 ± 2.4 mm to the right and 11.6 ± 2.5 mm to the left. In patients, repetitions of the analysis for the value deviations were from 0.1 to 0.3 mm for the right and 0.1 to 0.4 mm for the left side, respectively.
Protocol 2-Border movements, frontal plane
In this protocol, the trajectories of contacting laterality right (red) and left (blue) movements starting from MIP as well as border right (light blue) and left (green) openings were evaluated. In frontal view (Figure 3B), the particularities of the contacting lateral movement that differs from non-contacting laterality evaluated in protocol 1 could be observed. In addition, the borders for the opening movements that begin at the edge of the contacting literalities, forming the frontal border polygon revealing any deviation, anomaly or misuse of these movements can be evaluated in this view.
The lateral view (Figure 3C) reveals features of the anteroposterior movement that are usually not considered in this type of analysis, highlighting that there are different features in each of these different movements as well as the possibility of evaluating deviations. The superior plane (Figure 3D) allows for the evaluation of an unusual point of view of the movements in question and can identify deviations and changes in the trajectory at different points in the anteroposterior direction.
The assessed values in protocol 2 were of the frontal polygon area, maximum displacement and trajectory of the right and left contacting laterality as well as the right and left border opening trajectory were in Table 2.
| Patient | Rep. | Polig. Area FP | Right cont. lat. traj. | Right bord. op.track | Left lat. cont. traj. | Left bord. op.traj. | Right cont. lat. max. | Left cont. lat. max. | Mean ± SD | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Polig. Area FP | Right cont. lat. traj. | Right bord. op.track | Left lat. cont. traj. | Left bord. op.traj. | Right cont. lat. max. | Left cont. lat. max. | |||||||||
| 1 | 1 | 418.1 | 46.4 | 60.2 | 41.9 | 71.1 | 8.8 | 10.9 | 440.1 ± 19.1 | 45.9± 12.8 | 63.8± 3.2 | 45± 9.2 | 65.9± 4.7 | 9.4± 0.7 | 11.3± 0.4 |
| 2 | 449.3 | 58.5 | 66 | 37.8 | 61.9 | 9.3 | 11.3 | ||||||||
| 3 | 452.9 | 32.8 | 65.3 | 55.3 | 64.8 | 10.2 | 11.6 | ||||||||
| 2 | 1 | 599.5 | 38.2 | 73.6 | 36.6 | 74.5 | 12.8 | 9.1 | 605. ± 6.7 | 38.7± 2.1 | 74.9± 1.3 | 37.3± 1.7 | 75.3± 1.5 | 12.8± 0.03 | 9.2± 0.1 |
| 2 | 612.7 | 41 | 74.9 | 39.2 | 74.4 | 12.8 | 9.3 | ||||||||
| 3 | 603.8 | 36.8 | 76.2 | 36 | 77.1 | 12.9 | 9.1 | ||||||||
| 3 | 1 | 270.3 | 46.9 | 76.6 | 37 | 63.4 | 8.2 | 7.1 | 270.1 ± 0.3 | 48.5± 2.3 | 72.3± 6.11 | 37.3± 0.4 | 68.2± 6.8 | 8± 0.2 | 7.1± 0.04 |
| 2 | 267 | 50.1 | 67.9 | 37.6 | 73 | 7.9 | 7.1 | ||||||||
| 3 | |||||||||||||||
| 4 | 1 | 487.4 | 45.6 | 85.5 | 43.7 | 97.7 | 13.1 | 12.1 | 490.6± 14 | 43.3± 2.3 | 82.7± 6.9 | 43.8± 2.6 | 85.5± 10.6 | 13.1± 0.01 | 12.2± 0.1 |
| 2 | 478.5 | 43.1 | 87.7 | 46.5 | 78.2 | 13.1 | 12.1 | ||||||||
| 3 | 505.9 | 41 | 74.8 | 41.3 | 80.6 | 13.1 | 12.3 | ||||||||
| 5 | 1 | 602.7 | 64.5 | 88.7 | 59.3 | 76.5 | 12.6 | 14.6 | 602.3± 22.9 | 51.5± 11.2 | 75.1± 11.8 | 55.5± 5.7 | 75.7± 3 | 12.9± 0.3 | 14.7± 0.1 |
| 2 | 624.9 | 45.1 | 69.3 | 58.3 | 78.3 | 13 | 14.6 | ||||||||
| 3 | 579.2 | 45 | 67.3 | 49 | 72.4 | 13.1 | 14.8 | ||||||||
| 6 | 1 | 458.8 | 40.1 | 85.5 | 28.6 | 74.5 | 9.3 | 9.6 | 410.1± 43.3 | 40.1± 6.6 | 75.1± 13.4 | 30.7± 3.1 | 72.8± 1.5 | 9.3± 0.1 | 9.7± 0.1 |
| 2 | 376.3 | 33.5 | 80 | 29.1 | 71.5 | 9.2 | 9.8 | ||||||||
| 3 | 395.1 | 46.6 | 59.9 | 34.3 | 72.6 | 9.4 | 9.8 | ||||||||
| Mean | 481.5 | 44.4 | 74.1 | 41.9 | 74.3 | 11.1 | 10.9 | ||||||||
| SD | 110 | 7.8 | 8.9 | 8.9 | 7.8 | 2 | 2.3 | ||||||||
Table 2: Protocol 2 data, mandibular border movements in frontal plane.
Frontal border movement polygon area-This parameter considered the Polygon area formed by border movements in the frontal plane. The area of this polygon ranged from 297 to 624.9 mm2 in assessments of six patients, with a mean area and SD of 481.5 ± 110 mm2. Between movement repetitions, the SDs ranged from 0.3 to 43.3 mm2.
Right and left contacting laterality trajectory-This parameter evaluated the track of the contacting laterality to the right and left sides. The path of laterality right-contacting ranged from 32.8 to 64.5 mm, with a mean and SD of 44.4 ± 7.8 mm; to the left side of the path, there was variation from 28.6 to 59.3 mm, with a mean and SD of 41.9 ± 8.9 mm. In the evaluation between repetitions of the patients, the values of the SDs were between 2.1 to 12.8 mm to the right side and from 0.4 to 9.2 mm to the left side.
Maximum displacement of the right and left-contacting laterality-This parameter evaluated the point of maximum linear displacement of laterality that began in MIP. On the right side, displacement ranged from 7.9 to 13.1 mm, with mean and SD of 11.1 ± 2.0 mm; to the left side, the values were 7.1 to 12.1 mm, with a mean and SD of 10.9 ± 2.3 mm. The evaluation of the repetitions for recording the deviations were between 0.01 to 0.7 mm to the right side and 0.04 to 0.4 mm to the left side.
Right and left border opening trajectory - This parameter evaluated the trajectory in every direction (3D) of the right and left border opening as well as starting from the maximum displacement point of the contacting laterality. Analysing the records of six patients, the path of border opening right ranged from 59.9 to 88.7 mm (mean ± SD, 74.1 ± 8.9 mm), and to the left side, it ranged from 61.9 to 97.7 mm (mean ± SD, 74.3 ± 7.8 mm). The analysis revealed the repetition path to the right side, with the SD ranging from 1.3 to 13.4 mm and for the left, ranging from 1.5 to 10.6 mm.
Protocol 3-Border movements in the sagittal plane
This protocol evaluated the trajectory of movements of maximum protrusion and mouth opening in mandibular protrusion (blue) as well as mouth opening in mandibular retrusion (green). In the lateral view (Figure 4B), it was noted the formation of the sagittal border polygon. For points of the protrusive trajectory, such as edge to edge, the maximum protrusion and maximum opening point are observed. The frontal view (Figure 4C), usually not assessed in these movements, and may reveal lateral deviations, especially in the superior-inferior direction. In this case, the value was less than 5 mm, which can indicate a significant change. The superior view (Figure 4D) can also help reveal these deviations, and in this case, it is possible to assess at the points in the anteroposterior direction.
In this protocol, the polygon area formed by border movements in the sagittal plane was evaluated as were the linear displacements of protrusion and retrusion and the protrusive and retrusive trajectories, these data were presented in Table 3.
| Patient | Rep. | Polig. Area SP | Max. Prot. | Max. Retr. | Prot. traj. | Retr. traj. | Mean ± SD | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Polig. Area SP | Max. Prot. | Max. Retr. | Prot. traj. | Retr. traj. | |||||||
| 1 | 1 | 83.7 | 8.3 | 26.4 | 91.3 | 71.3 | 62.6 ± 20.4 | 8.3 ± 0.06 | 25.4 ± 1.6 | 90 ± 2.4 | 65.7 ± 7 |
| 2 | 61.2 | 8.4 | 26.3 | 91.5 | 68 | ||||||
| 3 | 43 | 8.3 | 23.5 | 87.3 | 57.8 | ||||||
| 2 | 1 | 84 | 10.2 | 37 | 113.4 | 86.3 | 80.1 ± 19 | 10.3 ± 0.08 | 36.8 ± 2.10 | 113.6 ± 0.2 | 84.7 ± 1.8 |
| 2 | 59.4 | 10.4 | 38.8 | 113.5 | 85.2 | ||||||
| 3 | 96.8 | 10.3 | 34.6 | 113.8 | 82.8 | ||||||
| 3 | 1 | 13.9 | 3.5 | 37.4 | 97 | 79.9 | 12.6 ± 2.7 | 4.2 ± 0.7 | 36.7 ± 0.6 | 99.8 ± 3.8 | 79.5 ± 1.4 |
| 2 | 9.5 | 4.8 | 36.6 | 104.1 | 80.7 | ||||||
| 3 | 14.4 | 4.4 | 36.2 | 98.2 | 78 | ||||||
| 4 | 1 | 83.5 | 11.1 | 25.7 | 127.2 | 85.2 | 73.3 ± 13.7 | 11.1 ± 0.4 | 27 ± 1.3 | 119.3 ± 6.8 | 90.3 ± 5.2 |
| 2 | 57.7 | 11.5 | 28.3 | 115.5 | 90.2 | ||||||
| 3 | 78.6 | 10.8 | 27 | 115.3 | 95.6 | ||||||
| 5 | 1 | 130.8 | 10.8 | 15.6 | 154.1 | 81.2 | 97.5 ± 30.9 | 10.4 ± 0.4 | 16.8 ± 2.8 | 136.9 ± 15.2 | 91.4 ± 11.7 |
| 2 | 91.9 | 10.4 | 14.8 | 125.2 | 104.1 | ||||||
| 3 | 69.7 | 10.1 | 19.9 | 131.4 | 89 | ||||||
| 6 | 1 | 44.2 | 8.4 | 21.4 | 102.4 | 72.6 | 65.7 ± 19.8 | 8.1 ± 0.4 | 23.4 ± 2 | 101.5 ± 8.1 | 76.2 ± 3.5 |
| 2 | 83.1 | 8.2 | 25.3 | 109.1 | 79.6 | ||||||
| 3 | 69.8 | 7.7 | 23.5 | 93.1 | 76.5 | ||||||
| Mean | 65.3 | 8.7 | 27.7 | 110.2 | 81.3 | ||||||
| SD | 31.6 | 2.4 | 7.5 | 17 | 10.5 | ||||||
Table 3: Protocol 3 data, Mandibular border movements in sagittal plane.
Sagittal border movement polygon area-The values of the sagittal polygon area showed wide variation from 9.5 to 130.8 mm2, with mean and SD of 65.3 ± 31.6 mm2. In the evaluation of the repetitions, the SDs also had a wide variation of between 2.7 and 30.9 mm2.
Mandibular displacement in protrusive movement-This parameter evaluated the linear displacements of the sagittal plane in the anteroposterior direction during mandibular protrusion movement (Figure 4B, Line y). The values varied from 3.5 to 11.5 mm, with a mean and SD of 8.7 ± 2.4 mm. Considering only the repetitions for the same patient, the SD values ranged from 0.06 to 0.7.
Mandibular displacement in retrusion associated with maximum mouth opening-This parameter assesses the anteroposterior displacement in the sagittal plane of the jaw during the retraction movement, which is followed by maximal mouth opening (Figure 4B, Line x). The values varied from 14.8 to 38.8 mm; the mean and SD were 27.7 ± 7.5 mm, respectively. When considering the repetitions, the SD values were 0.6 to 2.8 mm.
Protrusive and retrusive trajectories-These parameters evaluated the trajectories of contacting retrusive and protrusive movements followed by maximum mouth opening in both cases considering all planes and directions of movement. The protrusive path values ranged from 87.3 to 154.1 mm, with a mean and SD of 110.2 ± 17 mm, while retrusive paths ranged from 57.8 to 104.1 mm, with a mean and SD of 81.3 ± 10.5 mm. Among the repetitions of movements, the SD values were 0.2 to 15.2 mm in the protrusive path and 1.4 to 11.7 mm in the retrusive trajectory.
Discussion
There are many studies that seek to systematically and reproducibly assess mandibular motion [5,8,18] because the analysis of these movements is an important method for diagnosing problems in the masticatory system, especially in terms of the TMJ dynamics [1-5]. Therefore, understanding has increasingly been refined, and an accurate understanding of these movements is of great clinical importance for dental practice [9].
The 3D graphics of the jaw movements obtained in this study allowed for free visualization at different angles and magnifications; therefore, it was possible to observe the main features in the movement path for planes that are normally evaluated. However, it is important to highlight the benefit of evaluating the same movements in views that are not normally assessed, such as during mouth opening at the frontal border polygon in a lateral view or sagittal border polygon by a frontal and superior view. These types of analyses can reveal changes and deviations in movement that are often not perceived by views that are considered normal, and they may directly influence their efficiency and quality. In another stage, they may be related to articular and/or muscular problems.
The schemes presented in recent studies of jaw movements [5,19] show analysis in only one plane at a time without freedom of movement analyses in 3D. The previous study by our research group [9] presented schemes in VisArtico software that allowed for their free movement on any axis or vision plane; however, the use of interactive MATLAB scripts revealed a friendlier and intelligible interface compared to VisArtico.
Among the parameters analysed, we can classify them into three distinct categories, such as: 1. Displacement analysis that evaluated only one axis point, as represented by mouth opening, displacement in the laterality contacting and noncontacting movements, and protrusive and retrusive displacement in the sagittal plane; 2. movement trajectories that consider the free movement in any direction/axis, which was represented by the trajectories of mouth opening, contacting and non-contacting laterality and protrusion and retrusion; and 3. areas of polygons formed by the frontal and sagittal border movements.
It is intuitive to relate the variability of these three classes of parameters to their complexity; however, the study data showed, for example, that some patients have offset values on a simple axis that vary more than the area values and trajectories in others. Furthermore, certain motion types also revealed a high variation between patients and repetitions of the same patient. These are considered to be more complex than those relying on increased knowledge and concentration, such as for lateral border opening, which starts from the maximum-contacting laterality. Special attention is also needed to the area of border sagittal movements, such as its great variability and the difficulty of movement performance by patients who formed very irregular polygons with these movements.
Even today, there are some simple methods for evaluating mandibular movements, including the use of rules, callipers and visual analogue scales [1,3,4,20]. These methods have the advantage of low cost, but very important factors, such as accuracy, standardization and systematization, can become uncertain in their application.
The “ARCUSdigma II facebow” is a computerized axiograph that operates based on the analysis and imaging of the hinge axis as well as its movement, which is used to calculate the condylar path inclination, Bennett’s angle, immediate side shift, and Bennett’s shift, allowing for qualitative on-screen computer analysis of mandibular movements [21]. This device is considered to be the gold standard for analysing mandibular movements [21-23]. However, it has the disadvantage of interfering with the free/natural mandibular movement by constituting a “facebow”.
Another commonly used device for evaluating mandibular movements is the “mandibular kinesiograph”, which also contains a facebow and has been criticized for controversial results mainly related to “maximum mouth opening”, even been considered clinical useless resource [24]. Due to the characteristics of the EMA that have a high spatial and temporal fidelity whose data are collected by 9 transmitter coils, at a frequency of 250 hz (250 data/axis/sensor/second), no aberrant or controversial data of the measures obtained should be obtained.
Therefore, the analysis proposed in this study, using EMA AG 501 associated with MATLAB, has advantages in all of these aspects. The systematization of new varieties of all measures is processed by focused mathematical software that allows for survey analysis as well as simple and rapid data generation. This approach allows for customization of developed routines for obtaining various data related to mandibular movements with high accuracy and quality of the obtained schemes, easy comparison of data from different groups of patients, and noninvasive protection of the physical integrity of the evaluated patients.
A study that was previously reported by our research group [9] pioneered the use of EMA in evaluating mandibular movements. It is commonly used for speech therapy, especially to assess the stomatognathic system changes that are related to speech. The literature also demonstrated the use of the MATLAB software to analyse the head and neck with respect to speech changes [25,26]; however, in these cases, tongue movement data were obtained from the magnetic resonance method.
The limitations of the study are revealed in the small sample of patients, which was intentional because it is an attempt at innovation in the evaluation protocols of these movements. Therefore, studies with a small, homogeneous sample of patients were performed; these patients were not divided into different groups. Furthermore, it is possible to refine and improve the protocols and data evaluation routines to improve the application for achieving objectives of further studies.
The new method presented in this study to analyse mandibular border movements using EMA AG501 associated with MATLAB scripts Uses equipment with high spatial and temporal fidelity with a differentiated data processing due to the use of MATLAB, since it generates complete schemes for visualization of the trajectories of the 3D movements, which are similar to the classic studies with high precision of measurements in a systematic, easy and intuitive way. These factors allow for further analysis of different patient groups in which it will be possible to evaluate changes in the mandibular movements in the various spatial planes and/or views, resulting in the higher quality and greater reliability of these clinical analysis. The next studies performed by our research group will be based on this analysis method and will seek to evaluate other functional movements, such as the masticatory cycles and swallowing as well as analyse muscle function and functional efficiency. It will increasingly be necessary to adapt/ customize the MATLAB scripts and motion protocols that generate the most significant results for each type of evaluation in the future.
Conflict of Interest Statement
The authors report no conflict of interest.
References
- Hirsch C, John MT, Lautenschlager C, List T. Mandibular jaw movement capacity in 10-17-yr-old children and adolescents: normative values and the influence of gender, age, and temporomandibular disorders. Eur J Oral Sci 2006; 114: 465-470.
- Sousa LM, Nagamine HM, Chaves TC, Grossi DB, Regalo SC, Oliveira AS. Evaluation of mandibular range of motion in Brazilian children and its correlation to age, height, weight, and gender. Braz Oral Res 2008; 22: 61-66.
- Machado BC, Medeiros AP, Felício CM. Mandibular movement range in children. Pro Fono 2009; 21: 189-194.
- Mazzetto MO, Hotta TH, Pizzo RC. Measurements of jaw movements and TMJ pain intensity in patients treated with GaAlAs laser. Braz Dent J 2010; 21: 356-360.
- Sojka A, Huber J, Kaczmarek E, Hedzelek W. Evaluation of Mandibular Movement Functions Using Instrumental Ultrasound System. J Prosthodontics 2015.
- Schmidt KC, Briesemeister M, Ries LGK. Changes in mandibular and cervical motor control of children with cerebral palsy. Revista CEFAC 2014; 16: 228-236.
- Yazdani J, Ebrahimi H, Talesh KT, Khashabi E, Pourshahidi S. Comparing the effect of 3 orthognathic surgical methods on the mandibular range of movement. J CraniofacSurg 2010; 21: 703-705.
- Ahlers MO, Bernhardt O, Jakstat HA, Kordab B, Turp JC, Schindler HJ, Hugger A. Motion analysis of the mandible: concept for standardized evaluation of computer-assisted recording of condylar movements. ZeitschriftfürKraniomandibuläreFunktion 2014; 6: 333-3352.
- Fuentes R, Navarro P, Curiqueo A, Ottone NE. Determination of mandibular border and functional movement protocols using an Electromagnetic Articulograph (EMA). Int J ClinExp Med 2015; 8: 19905-19916.
- Kuruvilla M, Murdoch B, Goozèe J. Electromagnetic articulography assessment of articulatory function in adults with dysarthria following traumatic brain injury. Brain Inj 2007; 21: 601-613.
- Toutios A, Ouni S, Laprie Y. Estimating the control parameters of an articulatory model from electromagnetic articulograph data. J AcoustSoc Am 2011; 129: 3245-3257.
- Kaburagi T, Honda M. Electromagnetic articulograph based on a nonparametric representation of the magnetic field. J AcoustSoc Am 2002; 111: 1414-1421.
- Kaburagi T, Wakamiya K, Honda H. Three-Dimensional Electromagnetic Articulograph Based On A Nonparametric Representation Of The Magnetic Field. Seventh IntConfSpok Lang Proc 2002.
- Yunusova Y, Green JR, Mefferd A. Accuracy assessment for AG500, electromagnetic articulograph. J Speech Lang Hear Res 2009; 52: 547-555.
- Stella M, Bernardini P, Sigona F, Stella A, Grimaldi M, Fivela BG. Numerical instabilities and three-dimensional electromagnetic articulography. J AcoustSoc Am 2012. 132: 3941-3949.
- WHO. World Health Organisation-Electromagnetic fields and public health: Intermediate Frequencies (IF). WHO Int 2016.
- Posselt U. Studies in the mobility of the human mandible, Copenhagen. ActaOdontScand 1952; 10: 10.
- Eberhard L, Braun S, Wirth A, Schindler HJ, Hellmann D, Giannakopoulos NN. The effect of experimental balancing interferences on masticatory performance. J Oral Rehabil 2014. 41: 346-352.
- Pinheiro Junior PF, Albuquerque LCA, Silva CLDL, Silva NFD, Cunha DAD, Silva HJD. Amplitude and speed of masticatory movements in total laryngectomy patients. Braz J Otorhinolaryngol 2014; 80: 138-145.
- Flores-Orozco EI, Rovira-Lastra B, Peraire M, Salsench J, Martinez-Gomis J. Reliability of a visual analog scale for determining the preferred mastication side. J Prosthet Dent 2016; 115: 203-208.
- Wieckiewicz M, Zietek M, Nowakowska D, Wieckiewicz W. Comparison of selected kinematic facebows applied to mandibular tracing. Biomed Res Int 2014; 2014: 818694.
- Flores-Orozco EI, Rovira-Lastra B, Willaert E, Peraire M, Martinez-Gomis J. Relationship between jaw movement and masticatory performance in adults with natural dentition. ActaOdontolScand 2016; 74: 103-107.
- Frisoli M, Edelhoff JM, Gersdorff N, Nicolet J, Braidot A, Engelke W. Comparative study using video analysis and an ultrasonic measurement system to quantify mandibular movement. Cranio 2006; 13: 1-11.
- Cooper BC, Adib F. An assessment of the usefulness of Kinesiograph as an aid in the diagnosis of TMD: a review of Manfredini studies. Cranio 2015; 33: 46-66.
- Iltis PW, Frahm J, Voit D, Joseph AA, Schoonderwaldt E, Altenmuller E. High-speed real-time magnetic resonance imaging of fast tongue movements in elite horn players. Quant Imaging Med Surg 2015; 5: 374-381.
- Iltis PW, Frahm J, Voit D, Joseph A, Schoonderwaldt E, Altenmuller E. Divergent oral cavity motor strategies between healthy elite and dystonic horn players. J ClinMovDisord 2015; 21: 15.