Research Article - Journal of Clinical Ophthalmology (2023) Volume 7, Issue 1
An eye-tracking-based binocular amblyopia treatment improving both visual acuity and binocularity: One year follow-up.
Tamara Wygnanski-Jafe1,2, Michael Belkin2,3, Oren Yehezkel4*
1 Department of Ophthalmology, Goldschleger Eye Institute, Tel-Hashomer, Israel
2 Department of Medicine, Tel-Aviv University, Tel-Aviv, Israel
3 Department of Ophthalmology, Goldschleger Eye Research Institute, Sheba Medical Center, Tel Hashomer, Israel
4 NovaSight Ltd, Airport City, Israel
- Corresponding Author:
- Dr. Oren Yehezkel Scientific Department, NovaSight Ltd, Airport City 7019801, Israel E-mail: oren.yehezkel@gmail.com
Received: 30-Dec-2022, Manuscript No. AACOVS-22-85085; Editor assigned: 02-Jan-2023, PreQC No. AACOVS-22-85085 (PQ); Reviewed: 16-Jan-2023, QC No. AACOVS-22-85085; Revised: 23-Jan-2023, Manuscript No. AACOVS-22-85085 (R); Published: 31-Jan-2023, DOI: 10.35841/aacovs.7.1.605-613
Citation: Wygnanski-Jafe T, Belkin M, Yehezkel O. An eye-tracking-based binocular amblyopia treatment improving both visual acuity and binocularity: One year follow-up. J Clin Ophthalmol. 2023; 7(1): 605-613
Abstract
Background: Amblyopia is a neurodevelopmental disorder resulting from abnormal visual experience early in life.
Purpose: To evaluate the efficacy and safety of a novel binocular eye-tracking-based passive home treatment system delivering personalized amblyopia therapy.
Methods: Real-time foveal area blur was induced on the dominant eye of 20 participants (aged 4-15 years) with anisometropic, strabismic (<5 PD), or mixed amblyopia in a prospective single- arm proof-of-concept human study. Subjects were trained over 12 weeks with 5 weekly sessions and then for an additional 12 weeks with 3 weekly sessions. Primary outcome was improvement in Best Corrected Visual Acuity (BCVA) and stereoacuity. Secondary outcomes were adherence, improvement persistence and patient-reported comfort.
Results: Mean BCVA significantly improved by 0.19 ± 0.11 logMAR for distance crowded VA, 0.27 ± 0.13 logMAR for near crowded VA, and by 0.22 ± 0.15 logMAR for distance single letter VA (p<0.001 for each). Stereoacuity improved by 198 ± 218 arcsec (p=0.001). Binocular VA improved 0.09 ± 0.13 logMAR for distance crowded VA (p=0.007), 0.12 ± 0.11 logMAR for near crowded VA (p<0.001) and 0.07 ± 0.12 logMAR for distance single letter VA (p=0.018). The adherence rate was 89% ± 27%. No patient reported discomfort. At 52 weeks, distance crowded VA, distance single letter VA, and stereoacuity were not significantly different from the end-of- treatment measurements.
Conclusion: The system improved VA and stereoacuity and produced a high adherence rate with no reported discomfort. Improvement persisted for 6+ months.
Translational relevance: A novel binocular treatment based on passive viewing of customized content, modified to reinforce the amblyopic eye, resulted in VA and stereoacuity improvement in a small, first-in-human study, suggesting that this treatment might reduce interocular suppression.
Keywords
Amblyopia, Binocular treatment, Dichoptic, Eye tracking, Stereopsis.
Introduction
Amblyopia is a cortical visual impairment occurring in 1%-5% of the population worldwide that cannot be attributed to the effect of structural abnormalities of the eye or ocular disease [1,2]. It is the most common cause of monocular vision loss in children. In addition to reduced Visual Acuity (VA), amblyopia can cause dysfunctions of accommodation, fixation, binocularity, vergence, reading speed and fluency, color vision, motion processing, fine-motor skills, stereoacuity (depth perception) and contrast sensitivity [3-11].
Several studies performed in children with amblyopia aged between 3 to 7 years have shown that in some cases optical correction, patching or and atropinization treatment can successfully treat the disorder, and this can be followed by penalization or occlusion therapy if the child fails to improve with optical therapy alone; numerous randomized controlled trials have shown that spectacles, patching, and atropine treatment can continue to be effective treatments for children up to age 17 and that even adults may benefit from treatment [12-24].
Poor adherence to treatment regimens is a leading cause of failure to improve, although some studies suggest that even with proper adherence to patching treatment the condition may not improve [25-28]. Patching, however, has its own drawbacks, including negative psychosocial effects and poor adherence [29,30]. Moreover, although 79% of children show at least a 2-line improvement after 4 months of patching [29], 25% regress once the patch is removed [31], and perhaps more importantly, the binocular outcome is often poor regardless of the improved VA of the amblyopic eye [32], which may be due to the monocular nature of the viewing conditions during patching.
Novel treatment techniques have shifted from monocular treatment (patching and atropinization) to targeting binocular visual function [33-37]. In this treatment strategy, the amblyopic eye remains the primary eye performing any given visual task, and may include presentation of modified visual stimuli to each eye or dichoptic contrast balance [38]. A benefit is that by minimizing interocular suppression to a level where the eyes are capable of transferring their images to the brain simultaneously, both VA and the binocular function would improve. Various studies have supported that concept, showing dichoptic contrast balancing methods have significantly improved both VA and/ or stereoacuity in all types of amblyopia (strabismic (caused by eye deviation leading to abnormal binocular interaction), anisometropic (caused by the absence of a clear image on the retina), or a combination of the two) [33,34]. Video games have been evaluated as another avenue for binocular treatment, but no consensus on the potential benefit of binocular treatment as a substitute for conventional therapies has been reached [14,22,38-42]. Dichoptic action-adventure games and/or movies seem to have better adherence in younger and teenaged children, and may be able to improve patching compliance and VA as well [43-48]. However, Guo et al. were unable to find significant differences in VA when the age range expands to include adults [49]. Other studies using virtual reality headsets found improvements in VA, stereoacuity, or both, when used in adults and children [45,50-59].
In our present study, we present a first-in-human, preliminary evaluation of a novel binocular treatment based on passive viewing of customized content, modified to reinforce the amblyopic eye without the subject noticing (CureSightTM). Our hypothesis suggests the real-time eye tracking and custom software would result in consistent selective foveal blur in the non-amblyopic eye and create a very high adherence by 1) eliminating the discomfort inherent to patching and 2) exploiting the prevailing desire to consume digital content by the relevant age group.
Materials and Methods
Participants were prospectively recruited from the Goldschleger Eye Institute at the Sheba Medical Center, Israel (MOH_2018- 11-26_004806 (02/12/2018), available at: https://my.health.gov. il/CliniTrials/Pages/MOH_2018-11-26_004806.aspx) and was retrospectively listed on clinicaltrials.gov (NCT05078099). The study was approved by the Institutional Review Board of the Sheba Medical Center, Israel, and written informed consent was obtained from all guardians. The study adhered to the ethical standards established by the Declaration of Helsinki for research involving human participants. Participants were consecutively recruited from the hospital clinic, until the required sample size was obtained. All participants were screened by a pediatric ophthalmologist and a diagnosis of amblyopia was confirmed before study entry. The study enrolled its first participant on December 2, 2018, and the last participant/last visit was performed on March 19, 2020.
Eligibility criteria included a diagnosis of amblyopia due to strabismic, anisometropic, or combined mechanism amblyopia. Entry criteria included a BCVA in the amblyopic eye of ≥ 0.3 logMAR, with an interocular difference of ≥0.2 logMAR and difference in refraction of ≥ 1.00 D between eyes in spherical equivalent or ≥ 1.50 D difference in astigmatism between corresponding meridians in the two eyes. Eligible children wore optical correction for at least 16 weeks prior to the baseline visit. Exclusion criteria included developmental delay and coexisting ocular or systemic diseases, amblyopic eye VA lower than 1.0 logMAR (20/200), or any condition that might interfere with eye tracking, such as ptosis. All subjects underwent a complete ocular exam including at near and distance VA, stereoacuity, refraction, orthoptics and cycloplegic refraction. Strabismic children were eligible to participate only after correction of strabismus with glasses or surgery to <5 Prism Diopters (PD) residual strabismus or up to 10 PD of intermittent deviation. Distance and near crowded VA was measured using LEA symbols, ETDRS charts, and distance single letter was measured using Snellen chart.
Cure sight system
The Cure sight system comprises,
• All-in-1 PC with a passive 24” full HD display, Lenovo Ideacentre AIO 520, positioning the eye tracker, running the CureSight software and storing data in a cloud-based database.
• Eye tracker attached to the inferior border of the monitor, used for real-time eye tracking of the gaze position of each eye and providing real-time parameters to the software on the required blur coordinates.
• Anaglyph glasses used for creating separate channels for each eye.
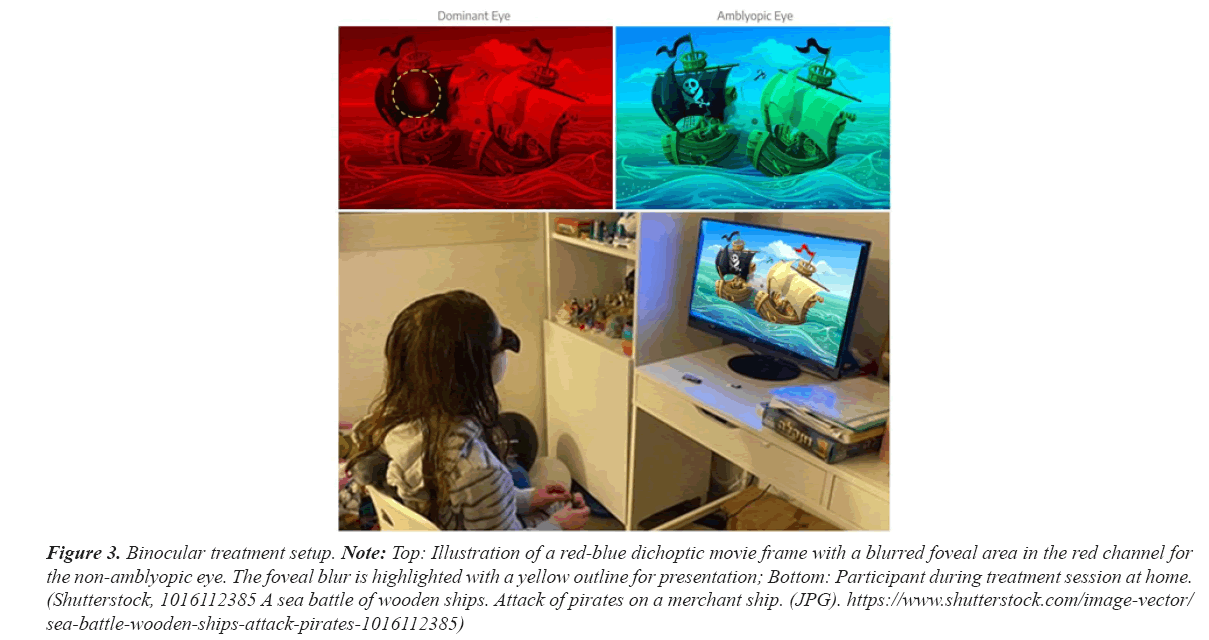
The customized software divides video content into two separate channels, resulting in dichoptic presentation. The input content included both ready-to-use side-by-side video files and regular 2D video formats converted into dichoptic format. Visual stimuli separate into two independent channels, red and blue, each presented to one of the eyes. The algorithm allows manipulating the content of each channel independently without affecting the content of the other eye. The blue channel was presented to the amblyopic eye and the red channel to the dominant one. A remote eye tracker (Tobii 4C 90 Hz) provided continuous information on the participant’s eye gaze position indicating the participant’s area of interest on the monitor. Proprietary software manipulates the dominant eye’s central vision area around the fovea to blur with a Gaussian envelope shape in respect to the participant’s real-time gaze position. The magnitude and diameter of the blurred area were fitted according to the VA of both the amblyopic and the dominant eye: the lower VA and larger the VA difference between the eyes, the greater the blur amplitude and diameter. The image presented to the amblyopic eye was not blurred. This manipulation is designed to encourage the visual system to use the amblyopic eye’s central image. The sharpness of the peripheral area of the dominant eye is not affected by the blur, to encourage the visual system to use the two images from both eyes simultaneously and thereby induce binocularity (Figure 1). The physician interacted with the system through a cloud-based interface to adjust treatment parameters according to participant’s current VA measured at each visit and to follow the participant performance to ensure compliance.
Study design
Participants were instructed to watch video content for 90 minutes a day over the course of 5 days per week for the initial 12 weeks, followed by 90 minutes per day over the course of 3 days per week for additional 12 weeks. During the treatment sessions, the children wore customized anaglyph red-blue glasses over their optical correction for watching dichoptic movies presented on the Cure sight system monitor placed at the participant’s home. Participants watched movies of their choice at a viewing distance of 50 cm-70 cm.
Study visits were scheduled to 4,8,12,24, and 52 weeks (± 1 week) after the baseline examinations (± 1 week), with the primary outcome visit scheduled at 24 weeks. At each visit, a constant set of examinations (distance and near VA, stereo acuity, Worth 4 Dot, reading test, distance and near PACT) were performed. A standardized questionnaire was administered to participants and their guardians to assess the presence and frequency of diplopia.
At each visit, distance BCVA was assessed using an electronic visual acuity system according to standard ATS testing protocols, using LEA SYMBOLS with crowded optotype for children up to age 7 or LEA NUMBERS for older children. Near (40 cm) BCVA was assessed using manual versions of the LEA SYMBOLS or LEA NUMBERS charts, depending on age of patient according to the ATS 4 protocol, including fast screening phase and. Stereoacuity was tested using the Titmus stereo acuity chart (Stereo Optical Co., US) for acuity values of 40 arc sec or higher, and Random Dot Stereo Acuity Test with LEA SYMBOLS (Vision Assessment Co., US) was used for values <40 arc sec. Ocular alignment was measured using a Simultaneous Prism and Cover Test (SPCT) and a Alternate and Prism Cover Test (APCT). A Nova sight call center contacted all subjects’ guardians if the weekly compliance fell below the 70% threshold to encourage better compliance with treatment and provide technical support. A web-based clinical dashboard was used to monitor each patient’s treatment throughout the study. The dashboard provided data on each patient’s daily/ weekly/total usage in real-time, including email notifications to the treating physician and the call center.
Patient satisfaction with the treatment was assessed at the end- of-treatment 24-week visit using the Net Promoter Score (NPS) question. Parents/guardians were asked how likely they would be to recommend the treatment to someone else, responding on a scale of 0 to 5, with 0 being not likely at all and 5 being very likely.
Statistical analysis
Effectiveness of the binocular treatment for amblyopia was tested using a Linear Mixed Model, with Repeated Measures for six time points (baseline, 4 weeks, 8 weeks, 12 weeks, 24 weeks, 52 weeks), including planned pairwise comparisons (paired t-tests). P-value <0.05 were considered significant. SAS Vs 9.4 was used for analysis. One participant was excluded from the analysis of stereo acuity due to unreliable cooperation with the test. Effect size was calculated using the Cohen's D for a paired t-test, defined as the mean of the paired differences divided by the standard deviation of these differences.
Results
Proof-of-concept study
This prospective single-arm proof-of-concept human study included 23 amblyopic children (4-15 years of age, mean age 8.25 ± 3.6 years (SD), 9 female), 20 of whom completed 6 months of treatment. The remaining 3 participants exited the study before the first 4-week visit due to schedule limitations. Three participants were excluded at screening. Participants included; 5 with strabismus, 12 with anisometropia, and 3 with combined mechanism amblyopia. Baseline characteristics are summarized in Table 1. Thirteen participants (56.5%) had been previously treated with patching (Table 1).
| Age | Sex | Amblyopic eye | Amblyopic eye VA | Fellow eye VA | Refractive error (OD) | Refractive error (OS) | Type | Tropia | Total Prior Duration in Refractive Correction (years) | Previous amblyopia treatment | Initial Stereo acuity |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 6 | F | OS | 0.52 | 0.24 | -14 | -789 | C | 7 X(T) | 4 | Yes | 200 |
| 8.1 | F | OD | 0.3 | -0.08 | -101.5 | -43.5 | A | 2 | No | 400 | |
| 7.3 | M | OS | 0.36 | 0.28 | -133.5 | -479.25 | C | 2 ET | 0.4 | Yes | 80 |
| 7.3 | F | OS | 0.5 | 0.24 | 0.75 | -5 | A | 1.5 | Yes | 100 | |
| 4 | M | OS | 1.02 | 0.4 | 1.5 | 4.75 | A | 1.5 | Yes | Fly | |
| 9.7 | M | OS | 0.46 | -0.08 | -88.5 | -84.75 | A | 1 | Yes | 200 | |
| 7.1 | M | OD | 0.62 | 0.28 | -85.75 | -47.5 | C | 5 ET | 1.8 | Yes | 400 |
| 8.5 | M | OD | 0.48 | 0.16 | 5 | -3.75 | S | 5 ET | 5 | Yes | 400 |
| 4.3 | F | OD | 0.7 | 0.56 | -175.75 | -131.5 | S | 10 E(T) | 0.4 | Yes | 200 |
| 4.2 | M | OD | 0.5 | 0.26 | -31 | -317 | A | 5.5 | Yes | 400 | |
| 10 | F | OS | 0.54 | 0.14 | 0.75 | -447 | A | 6 | Yes | 80 | |
| 16.1 | F | OS | 0.38 | 0.1 | -163.5 | -60.25 | A | 0.4 | No | 80 | |
| 10.8 | F | OD | 0.42 | 0.12 | -328 | -178 | A | 1 | No | 60 | |
| 6.11 | M | OD | 0.64 | 0.24 | -88 | -83.75 | A | 0.4 | No | Fly | |
| 6.02 | M | OS | 0.42 | 0.12 | -44 | -134 | S | 2 XT | 0.7 | No | 100 |
| 15.05 | F | OD | 0.36 | 0.12 | -39 | 1.25 | A | 0.4 | Yes | 80 | |
| 10.1 | M | OD | 0.64 | 0.02 | -174 | -174.75 | S | 4 ET | 0.4 | No | Nil |
| 6.61 | M | OD | 0.44 | 0.1 | -79.75 | -82.75 | A | 0.4 | No | 80 | |
| 6.87 | M | OD | 0.46 | 0.22 | 3 | 3 | S | 5 ET | 3 | Yes | 400 |
| 10.8 | F | OD | 0.3 | 0 | -41 | 0.25 | A |
8 | Yes | 80 |
Note: LogMAR: logarithm of the minimum angle of stereoacuity; SD: Standard Deviation; VA: Visual Acuity; A: Anisometropic; C: Combined mechanism; S: Strabismic; XT: exotropia; X(T): Intermittent exotropia; ET: Esotropia; E(T: intermittent esotropia. Angle of deviation at near was measured by simultaneous prism and cover test with habitual glasses.
Table 1. Baseline characteristics.
VA and stereoacuity
All examinations were performed by one pediatric ophthalmologist to avoid variation due to inter-examiner variability. Prior to treatment, the overall mean ± SD BCVA in the amblyopic eyes was 0.5 ± 0.17 logMAR for distance crowded VA, 0.5 ± 0.16 logMAR for near crowded VA, and 0.39 ± 0.15 logMAR for distance single letter VA (Table 2).
| Baseline | 4 weeks | 8 weeks | 12 weeks | 24 weeks | 52 weeks | |
|---|---|---|---|---|---|---|
| Distance VA Crowded | ||||||
| Mean | 0.5 | 0.4 | 0.33 | 0.31 | 0.31 | 0.31 |
| STDEV | 0.17 | 0.2 | 0.16 | 0.17 | 0.16 | 0.2 |
| Margin of Error | 0.07 | 0.09 | 0.07 | 0.07 | 0.07 | 0.09 |
| Near VA Crowded | ||||||
| Mean | 0.5 | 0.34 | 0.24 | 0.22 | 0.23 | 0.29 |
| STDEV | 0.16 | 0.15 | 0.11 | 0.13 | 0.15 | 0.18 |
| Margin of Error | 0.07 | 0.06 | 0.05 | 0.06 | 0.07 | 0.08 |
| Distance VA single | ||||||
| Mean | 0.39 | 0.3 | 0.24 | 0.24 | 0.17 | 0.24 |
| STDEV | 0.15 | 0.18 | 0.18 | 0.16 | 0.15 | 0.2 |
| Margin of Error | 0.07 | 0.08 | 0.08 | 0.07 | 0.07 | 0.09 |
| Stereo | ||||||
| Mean | 260 | 170.53 | 122.11 | 88.21 | 61.63 | 80.76 |
| STDEV | 233.05 | 187.16 | 175.07 | 89.32 | 41.3 | 63.13 |
| Margin of Error | 102.14 | 82.02 | 76.73 | 39.15 | 18.1 | 27.67 |
Table 2. Visual acuity and stereo acuity group measurements at six study visits.
Binocular BCVA was 0.14 ± 0.17 logMAR for the distance crowded VA, 0.17 ± 0.12 logMAR for the near crowded VA, and 0.04 ± 0.14 logMAR for the distance single letter VA. Stereoacuity was 260 ± 233 arcsec (a value of 800 arcsec was arbitrarily assigned if subjects failed the Titmus test).a
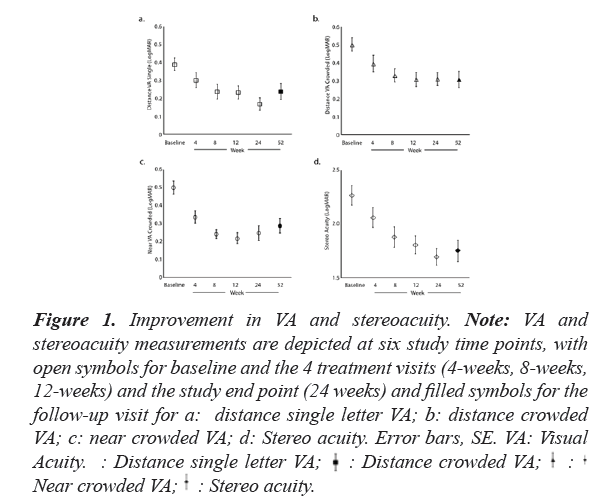
There was a significant positive effect of treatment in all examinations of the amblyopic eye (Table 3 and Figure 1).
| df, statistic | p value | |
|---|---|---|
| Amplyopic eye | ||
| Distance VA single | F(5,114)=4.001 | 0.002 |
| Distance VA ETDRS | F(5,114)=3.939 | 0.002 |
| Near VA ETDRS | F(5,114)=10.502 | 0 |
| Stereo | F(5,108)=4.682 | 0.001 |
| Binocular | ||
| Distance VA single | F(5,114)=4.001 | 0.002 |
| Distance VA ETDRS | F(5,114)=3.939 | 0.002 |
| Near VA ETDRS | F(5,114)=10.502 | 0 |
| Stereo | F(5,108)=4.682 | 0.001 |
Table 3. Tests of fixed effects.
Figure 1: Improvement in VA and stereoacuity. Note: VA and
stereoacuity measurements are depicted at six study time points, with
open symbols for baseline and the 4 treatment visits (4-weeks, 8-weeks,
12-weeks) and the study end point (24 weeks) and filled symbols for the
follow-up visit for a: distance single letter VA; b: distance crowded
VA; c: near crowded VA; d: Stereo acuity. Error bars, SE. VA: Visual
Acuity. : Distance single letter VA; 
At the primary endpoint of 24 weeks of treatment (total of 132.5 ± 38.1 hours), amblyopic eye VA significantly improved from baseline by 0.19 ± 0.11 logMAR for distance crowded VA, by 0.27 ± 0.13 logMAR for near crowded VA and by 0.22 ± 0.15 logMAR for distance single letter VA (Table 4).
| Distance_VA_single | ||||||
|---|---|---|---|---|---|---|
| MeanDiff | STDDiff | Cohens_D | DF | t Value | P Value | |
| Baseline Vs 4 weeks | 0.09 | 0.1 | 0.94 | 114 | 1.68 | 0 |
| 4 Vs 8 weeks | 0.06 | 0.1 | 0.62 | 114 | 1.16 | 0.013 |
| 8 Vs 12 weeks | 0.01 | 0.09 | 0.06 | 114 | 0.09 | 0.804 |
| 12 Vs 24 weeks | 0.07 | 0.1 | 0.63 | 114 | 1.21 | 0.012 |
| 24 Vs 52 weeks | -0.07 | 0.15 | -0.47 | 114 | -1.31 | 0.049 |
| Baseline Vs 24 weeks | 0.22 | 0.15 | 1.46 | 114 | 4.15 | 0 |
| Baseline Vs 52 weeks | 0.15 | 0.17 | 0.89 | 114 | 2.84 | 0.001 |
| Distance_VA_crowded | ||||||
| MeanDiff | STDDiff | Cohens_D | DF | t Value | P Value | |
| Baseline Vs 4 weeks | 0.11 | 0.1 | 1.03 | 114 | 1.9 | 0 |
| 4 Vs 8 weeks | 0.07 | 0.12 | 0.56 | 114 | 1.18 | 0.022 |
| 8 Vs 12 weeks | 0.02 | 0.07 | 0.32 | 114 | 0.41 | 0.175 |
| 12 Vs 24 weeks | 0 | 0.12 | -0.02 | 114 | -0.04 | 0.944 |
| 24 Vs 52 weeks | 0 | 0.12 | 0.03 | 114 | 0.05 | 0.912 |
| Baseline Vs 24 weeks | 0.19 | 0.11 | 1.73 | 114 | 3.46 | 0 |
| Baseline Vs 52 weeks | 0.2 | 0.12 | 1.63 | 114 | 3.51 | 0 |
| Near_VA_crowded | ||||||
| MeanDiff | STDDiff | Cohens_D | DF | t Value | P Value | |
| Baseline Vs 4 weeks | 0.16 | 0.11 | 1.52 | 114 | 3.51 | 0 |
| 4 Vs 8 weeks | 0.1 | 0.12 | 0.82 | 114 | 2.04 | 0.002 |
| 8 Vs 12 weeks | 0.02 | 0.07 | 0.34 | 114 | 0.51 | 0.145 |
| 12 Vs 24 weeks | -0.01 | 0.07 | -0.14 | 114 | -0.21 | 0.539 |
| 24 Vs 52 weeks | -0.06 | 0.12 | -0.5 | 114 | -1.29 | 0.038 |
| Baseline Vs 24 weeks | 0.27 | 0.13 | 2.16 | 114 | 5.85 | 0 |
| Baseline Vs 52 weeks | 0.21 | 0.11 | 1.96 | 114 | 4.57 | 0 |
| Stereo | ||||||
| MeanDiff | STDDiff | Cohens_D | DF | t Value | P Value | |
| Baseline Vs 4 weeks | 89.47 | 112.96 | 0.79 | 108 | 7.59 | 0.003 |
| 4 Vs 8 weeks | 48.42 | 90.02 | 0.54 | 108 | 4.98 | 0.031 |
| 8 Vs 12 weeks | 33.89 | 98.49 | 0.34 | 108 | 3.57 | 0.151 |
| 12 Vs 24 weeks | 26.58 | 82.72 | 0.32 | 108 | 2.58 | 0.178 |
| 24 Vs 52 weeks | -19.13 | 47.45 | -0.4 | 108 | 1.8 | 0.096 |
| Baseline Vs 24 weeks | 198.37 | 217.95 | 0.91 | 108 | 2.36 | 0.001 |
| Baseline Vs 52 weeks | 179.24 | 193.53 | 0.93 | 108 | 7.59 | 0.001 |
Table 4. Pairwise comparisons and Cohen’s D.
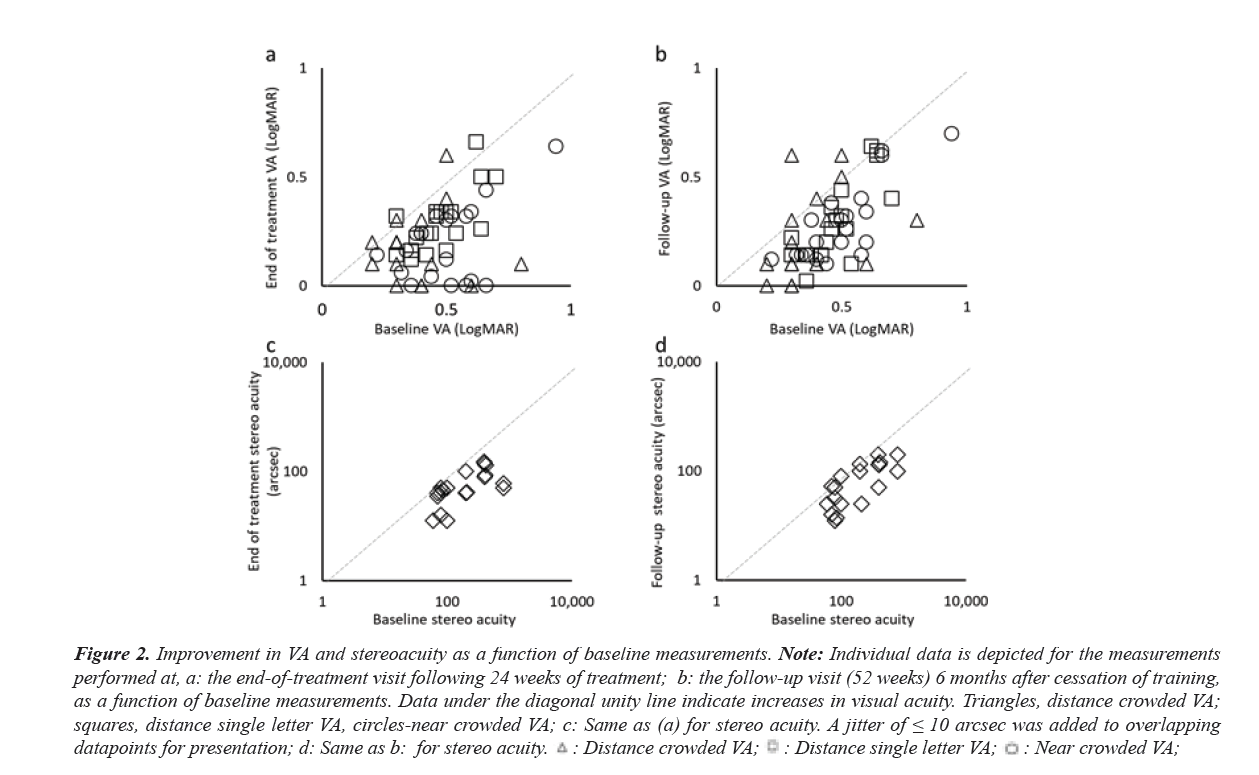
Importantly, stereoacuity improved by 198 ± 218 arcsec (equivalent to 76% or 2-octave improvement), with a posttreatment stereoacuity of 62 ± 41 arcsec. Both the VA and stereoacuity improvements were achieved by the 2-month study visit and all improvements were maintained through the 52-week follow-up visit. Only distance crowded VA and stereoacuity were not significantly different from the end-of- treatment measurements. At the 52 weeks’ visit, neither distance crowded VA nor distance single letter VA were significantly different from the end-of-treatment measurements. Figure 2 illustrates the improvement persistence and shows the outcomes per participant at 24 weeks and at 52 weeks.
Figure 2: Improvement in VA and stereoacuity as a function of baseline measurements. Note: Individual data is depicted for the measurements
performed at, a: the end-of-treatment visit following 24 weeks of treatment; b: the follow-up visit (52 weeks) 6 months after cessation of training,
as a function of baseline measurements. Data under the diagonal unity line indicate increases in visual acuity. Triangles, distance crowded VA;
squares, distance single letter VA, circles-near crowded VA; c: Same as (a) for stereo acuity. A jitter of ≤ 10 arcsec was added to overlapping
datapoints for presentation; d: Same as b: for stereo acuity. 
Binocular VA was significantly improved after 24 weeks of treatment by 0.09 ± 0.13 logMAR for distance crowded VA (p=0.007, Cohen’s D=0.68), by 0.12 ± 0.11 logMAR for near crowded VA (p<0.001, Cohen’s D=1.05) and by 0.07 ± 0.12 logMAR VA for distance single letter VA (p=0.018, Cohen’s D=0.57).
Adherence
Adherence was calculated as a percentage of the total time prescribed. At week 24, mean ± SD adherence to therapy was 89% ± 27%.
Worth 4 dot test
Prior to treatment, 10 participants showed suppression measured using the Worth 4 dot test performed at a distance of 6 matters, whereas only one participant showed suppression at the primary endpoint of 24 weeks of treatment.
Adverse events
Participants were continuously monitored for diplopia using diplopia questionnaire, new or worsening eye heterotropia, worsening VA, or any other unanticipated adverse event. No adverse events were reported.
Satisfaction survey
The mean ± SD response of the NPS was 4.79 out of maximal 5, including 15 of 20 parents/guardians who responded with 5,4 parents/guardians who responded with 4, and 1 parent/ guardian not answering. Parents/guardians were asked to grade their satisfaction with the treatment on a scale of 0 to 5, with 0 being not satisfied at all and 5 being very satisfied. Mean ± SD response was 4.70 out of maximal 5, including 14 of 20 parents/ guardians who responded with 5 and 6 parents/guardians who responded with 4.
Discussion
Conventional treatment of amblyopia includes patching or penalizing the dominant eye. However, patching does not always result in 20/20 vision with good stereoacuity and amblyopia recurrence is common. Furthermore, patching does not promote binocular cooperation and prevent suppression, the absence of which may be the actual cause for residual and recurrent amblyopia. In this first-in human prospective single- arm proof-of-concept human study evaluating the efficacy of a novel binocular eye-tracking based treatment system delivering personalized amblyopia therapy, we report an improvement in mean amblyopic eye VA at 24 weeks of 1.9, 2.7 and 2.2 lines (distance LEA, Near LEA, and distance single-letter Snellen, respectively). Moreover, treatment results were maintained for an additional 24 weeks without additional treatment. Our results are comparable to findings in participants of similar ages in a large-scale Pediatric Eye Disease Investigator Group (PEDIG) study [45]. In that study, after 16 weeks of therapy, mean amblyopic-eye VA of the participants in the patching group improved by 1.35 lines (95% CI 1.17–1.54 lines) and those in the iPad dichoptic game improved by 1.05 lines (95% CI 0.85–1.24 lines) [45]. Our study differs, however, in that 13 participants (65%) had prior amblyopia therapy, which often blunts response to subsequent therapy using traditional modalities [45].
Our study included participants who were either stereo-blind or stereo-deficient before treatment. Improvement of 2 octaves (equivalent of 76%) in stereoacuity was found at 24 weeks that was maintained for at least 6 months after treatment cessation. This magnitude of stereoacuity improvement is greater than most of the reported improvement in studies on patching and dichoptic treatments, which typically range from 0 to 1.5 octaves.
Our results may have important implications for the recovery of binocular function, even with treatment not explicitly targeted on improving stereoacuity. Few studies in the literature have directly addressed stereopsis directly [60]. However, some studies that directly measure interocular suppression after treatment found improvement in binocular VA and stereoacuity [61].This study also trained participants for a much longer period of time (24 weeks) than is typically reported in the literature (4- 16 weeks) [40], and evaluated persistence of treatment at 52 weeks. We found the effects of treatment with the CureSight remained stable for 6 months after treatment cessation. The vast majority of dta points that fell under the diagonal unity line in Figure 3 indicate improved VA; it is noteworthy that a similar plot for the 52-week follow-up data supports this supposition and illustrates improved persistence (Figure 3).
Figure 3: Binocular treatment setup. Note: Top: Illustration of a red-blue dichoptic movie frame with a blurred foveal area in the red channel for the non-amblyopic eye. The foveal blur is highlighted with a yellow outline for presentation; Bottom: Participant during treatment session at home. (Shutterstock, 1016112385 A sea battle of wooden ships. Attack of pirates on a merchant ship. (JPG). https://www.shutterstock.com/image-vector/ sea-battle-wooden-ships-attack-pirates-1016112385)
In this study, improvement in near crowded VA was higher by 26% compared to distance crowded VA. This finding warrants further investigation, as it suggests potential insights into the mechanism of the observed improvement. These may include improvement in accommodation and/or fixation due to the near viewing distance used for treatment. It is possible that longer treatment would result in a similar magnitude of improvement in distance VA as was observed for near VA, which should be explored in future studies.
Amblyopia treatment is highly dose-dependent, and it is widely accepted that adherence to prescribed treatment is critical.59 Engaging, personalized home-based therapy may improve adherence and treatment outcomes. To date, home- based treatments for amblyopia are many times associated with poor treatment adherence [40,51], or require compromises such as shorter treatment sessions. Gao, et al reported on 115 participants (children, teenagers and adults) and found that adherence of 65% ± 37% to home-based videogame treatment was characterized by short sessions (21.5 ± 11.2 minutes) and frequent pauses, suggesting regular disengagement [62]. These observations complicate dose-response calculations and may also interfere with the effectiveness of binocular treatments for amblyopia, which require within-session accumulation of visual stimulation. Xiao et al found a higher mean adherence of 78%, attributed to personalization of the treatment content. In this study, treatment adherence was 89%, substantially higher than that observed with patching or other binocular treatments [59]. Further, this study defined adherence as 75% of minimal prescribed time, which is generally considered a strict definition. Our adherence rates were sustained throughout the study, even with higher treatment duration (144 hours) than reported elsewhere.
This study is not without limitations, among them that this first- in human study included a relatively small number of patients with no randomization and no control group, and test-retest and learning effects were not considered. VA was measured at 20 feet, which can be difficult for young children, and VA measures were not masked, nor measured psychometrically. Stereoacuity was measured using the Titmus test which offers monocular cues, although if participants experience an improvement in VA, then they are more likely to recognize monocular cues and do so better than at baseline. However, these limitations need to be viewed within the context of the fact that this was a small first-in-human evaluation of a novel approach for the treatment of amblyopia, something that will require more comprehensive and structured clinical evaluation in future studies.
The study also had several strengths, including the fact that more than half of all participants had undergone prior patching, a known factor that limits the effect of binocular treatments [14,32], yet all 13 of those participants showed improvement on both VA and stereoacuity. The authors recognize the sample size does not equally represent all ages and all varieties of amblyopia. The Titmus test was used throughout the trial, and the participants improved on this test, negating the potential limitation of using this test.
Conclusion
A novel binocular treatment based on passive viewing of customized content, modified to reinforce the amblyopic eye, resulted in VA and stereoacuity improvement, suggesting treatment-induced reduction in inter ocular suppression. A large-scale randomized controlled trial to test the validity of the results reported herein is under way. The authors recognize the sample size does not equally represent all ages and all varieties of amblyopia. The system improved VA and stereoacuity and produced a high adherence rate with no reported discomfort. Improvement persisted for 6+ months.
Referencesa
- Woodruff ME. Amblyopia: Basic and clinical aspects. Opto Vis Sci. 1991;68(5):365-96.
- Wallace DK, Repka MX, Lee KA, et al. Amblyopia Preferred Practice Pattern. Ophthalmology. 2018;125:105-42.
[Cross Ref] [Google Scholar] [Pub Med]
- Sloper J. Amblyopia beyond acuity. JAAPOS. 2008;12(1):3-4.
[Cross Ref] [Google Scholar] [PubMed]
- Agrawal R, Conner IP, Odom JV, et al. Relating binocular and monocular vision in strabismic and anisometropic amblyopia. Arch Ophthalmol. 2006;124(6):844-50.
[Cross Ref] [Google Scholar] [PubMed]
- Rutstein RP, Corliss D. Relationship between anisometropia, amblyopia, and binocularity. Optom Vis Sci. 1999;76(4):229-33.
[Cross Ref] [Google Scholar] [PubMed]
- Ciuffreda KJ, Hokoda SC, Hung GK, et al. Static aspects of accommodation in human amblyopia. Am J Optom Physiol Opt. 1983;60(6):436-49.
[Cross Ref] [Google Scholar] [PubMed]
- Abraham SV. Accommodation in the amblyopic eye. Am J Ophthalmol. 1961;52(2):197-200.
[Cross Ref] [Google Scholar] [PubMed]
- Weakley Jr DR. The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity. Ophthalmology. 2001;108(1):163-71.
[Cross Ref] [Google Scholar] [PubMed]
- McKee SP, Levi DM, Movshon JA. The pattern of visual deficits in amblyopia. J vis. 2003;3(5):5-.
[Cross Ref] [Google Scholar] [PubMed]
- O'Connor AR, Birch EE, Anderson S, et al. Relationship between binocular vision, visual acuity, and fine motor skills. Optom Vis Sci. 2010;87(12):942-7.
[Cross Ref] [Google Scholar] [PubMed]
- Stifter E, Burggasser G, Hirmann E, et al. Monocular and binocular reading performance in children with microstrabismic amblyopia. British J Ophthalmology. 2005;89(10):1324-9.
[Cross Ref] [Google Scholar] [PubMed]
- Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120(3):268-78.
[Cross Ref] [Google Scholar ] [PubMed]
- Pediatric Eye Disease Investigator Group. Two-year follow-up of a 6-month randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2005;123(2):149-57.
[Cross Ref] [Google Scholar] [PubMed]
- Levi DM. Rethinking amblyopia 2020. Vision Res. 2020;176:118-29.
- Polat U, Ma-Naim T, Belkin M, et al. Improving vision in adult amblyopia by perceptual learning. Proc Natl Acad Sci. 2004;101(17):6692-7.
[Cross Ref] [Google Scholar] [PubMed]
- Levi DM. Perceptual learning in adults with amblyopia: a reevaluation of critical periods in human vision. Dev Psychobiol. 2005;46(3):222-32.
[Cross Ref] [Google Scholar] [PubMed]
- Repka MX, Beck RW, Holmes JM, et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121(5):603-11.
[Cross Ref] [Google Scholar] [PubMed]
- Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075-87.
[Cross Ref] [Google Scholar] [PubMed]
- Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111(11):2076-85.
- Repka MX, Beck RW, Holmes JM, et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2008;126 (8):1039-44.
[Cross Ref] [Google Scholar] [PubMed]
- Repka MX, Kraker RT, Holmes JM, et al. Atropine vs patching for treatment of moderate amblyopia: follow-up at 15 years of age of a randomized clinical trial. JAMA Ophthalmol. 2014;132(7):799-805.
[Cross Ref] [Google Scholar] [PubMed]
- Pediatric Eye Disease Investigator Group. Patching vs atropine to treat amblyopia in children aged 7 to 12 years: a randomized trial. Arch Ophthalmol. 2008;126(12):1634-42.
[Cross Ref] [Google Scholar] [PubMed]
- Repka MX, Kraker RT, Beck RW, et al. Treatment of severe amblyopia with weekend atropine: results from 2 randomized clinical trials. JAAPOS. 2009;13(3):258-63.
[Cross Ref] [Google Scholar] [PubMed]
- Scheiman MM, Hertle RW, Beck RW, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Arch Ophthalmol. 2005;123(4):437-47.
[Cross Ref] [Google Scholar] [PubMed]
- Oliver M, Neumann R, Chaimovitch Y, Gotesman N, et al. Compliance and results of treatment for amblyopia in children more than 8 years old. Am J Ophthalmol. 1986;102(3):340-5.
[Cross Ref] [Google Scholar] [PubMed]
- Pritchard C. Why Won't You Treat My 10 Year Old's Lazy Eye? Am Orthopt J. 1990;40(1):15-8.
- Loudon SE, Polling JR, Simonsz HJ. Electronically measured compliance with occlusion therapy for amblyopia is related to visual acuity increase. Graefe's Arch Clin Exp Ophthalmol. 2003;241(3):176-80.
[Cross Ref] [Google Scholar] [PubMed]
- Stewart CE, Moseley MJ, Stephens DA, et al. Treatment dose-response in amblyopia therapy: the Monitored Occlusion Treatment of Amblyopia Study (MOTAS). Invest ophthalmol Vis Sci. 2004;45(9):3048-54.
[Cross Ref] [Google Scholar] [PubMed]
- Holmes JM, Beck RW, Kraker RT, et al. Impact of patching and atropine treatment on the child and family in the amblyopia treatment study. Arch Ophthalmol. 2003;121(11):1625-32.
[Cross Ref] [Google Scholar] [PubMed]
- Felius J, Chandler DL, Holmes JM, et al. Evaluating the burden of amblyopia treatment from the parent and child’s perspective. JAAPOS. 2010;14(5):389-95.
[ -->