Research Article - Biomedical Research (2017) Volume 28, Issue 3
An ethnobotanical survey of medicinal plants used for the ailment of diabetes mellitus in Changzhi city of Shanxi province, China
Juan-juan Guo1*#, Jie Han2#, Shao-li Wang1 and Jie-ying Liu11Department of Geriatric Ward, Peace Hospital Affiliated of Changzhi Medical College, Changzhi, Shanxi, China
2Department of Respiratory Ward, Peace Hospital Affiliated of Changzhi Medical College, Changzhi, Shanxi, China
#These authors contributed equally to this work
- *Corresponding Author:
- Juan-juan Guo
Department of Geriatric ward
Peace Hospital Affiliated of Changzhi Medical College, PR China
Accepted on September 9, 2016
Abstract
Ethnopharmacological relevance: Traditional practitioners in Changzhi city of Shanxi (Chinese: ) province have been using the folk medicinal plants for a long time concerning various principle ailments. In this study, a lot of vital ethno pharmacological information has been provided which would be functional for further pharmacological study.
Aim of the study: The aim of this study was to collect, analyse and evaluate the deep ethnopharmacological information on medicinal plants against diabetes mellitus in Changzhi City of Shanxi (Chinese: ) province and tried to sort out some indigenous species that are used by traditional practitioners.
Materials and Methods: Actual fieldwork was conducted with the help of an open ended and semistructured questionnaire. Total 169 people were interviewed, including some indigenous peoples and Traditional Health Practitioners (THPs) of different villages in Changzhi City. Documented plants are enlisted with their application, part used, mode of preparation, frequency of use and Use Value (UV). Results: The result of the present study has showed that total 71 plant species belonging to 44 families have been reported for diabetes mellitus ailment. Roots were found to be used the major commonly plant parts and the method of preparation was the powder. The most frequent mode of administration was orally intake.
Conclusion: The current study shown that some of the medicinal plants are largely used for representing an efficient ethnobotanical practice in this survey area. Plants, which achieved low UV’s also need to bioactive screening to validate their utilization for the reported disease. This could be considered as well sign of prospective plants for finding out new drugs.
Keywords
Diabetes, Medicinal plants, Changzhi city, Shanxi province, China.
Introduction
Diabetes mellitus (DM) is one of the most familiar chronic diseases in almost all countries. A survey finds recently that above 439 million people will suffer in future from DM by 2030 [1]. DM is occurred due to defective insulin secretion, insulin action, or both [2]. The continuing high glucose level in the blood is the main reason to cause some diabetic complications such as diabetic neuropathy [3], diabetic ketoacidosis [4], diabetic cardiopathy [5], diabetic nephropathy [6] and diabetic retinopathy [7]. The highest diabetes epidemics finds in China, and it grows continuously at a fearsome pace. According to latest data, among adults 11.6% of Chinese have diabetes. Perhaps more ominously, another study also found that half had pre-diabetes (Abnormal blood glucose levels but not far above for a diabetes diagnosis) by surveying 99,000 people. This study suggests that there are 493.3 million with pre-diabetes. This health crisis of Chinese people would be a heavy economic burden in near future [8,9].
Due to expensive medication as well as availability of traditional Chinese natural medicine, Ethnomedicinal plants is regarded an important option in the treatment of DM. China, has a long famous history of traditional medicine, and developed a distinctive medicinal treatment system. Practicing of medicinal plants is based on a traditional knowledge that has been conceded orally from generation to generation in humans and not many written documents are accessible [10]. Total 4,20,000 flowering plants accounted from the world further than 50,000 are used intended for medicinal principles [11,12]. In accordance with the World Health Organization (WHO), with reference to 4 billion people in developing countries trust in the healing properties of medicinal plant species and moreover utilize them routinely [13]. Ethnopharmacology and natural drug discovery remains a considerable optimism in the humanizing the underprivileged incomes of countryside populations [14].
From the ancient time, not a single medicinal plant based work has been recorded on Changzhi. Therefore, we strived in broadly compilation of medicinal plants of Changzhi against DM. In this survey study, we tried to bring together ethnobotanical knowledge’s from different Traditional Health Practitioners (THPs) and from local informants in Changzhi City. From this survey, report we tried to make out most frequently used medicinal plants for diabetes with their mode of preparation and different part used for different therapeutic uses. From the data analysis, we showed the most valuable species and extent usable species for a given ailment. Therefore, this work presents a complete summary of ethnobotanical practices in Changzhi City. Rural peoples surviving here mainly depend on conventional medicinal healers for healing of their diseases: one cause is trustworthiness to the treatment also another cause is need of access new medicinal capabilities [15].
As a result, evaluation or exploration as well as documentation of information of indigenous group on the employ and management of medicinal plants would fill up the gap of indigenous information on medicinal plants [16]. It may help to provides further conservation of medicinal plant based knowledge and make it possible to discover ethnopharmacological based novel drug.
Materials and Methods
Study area
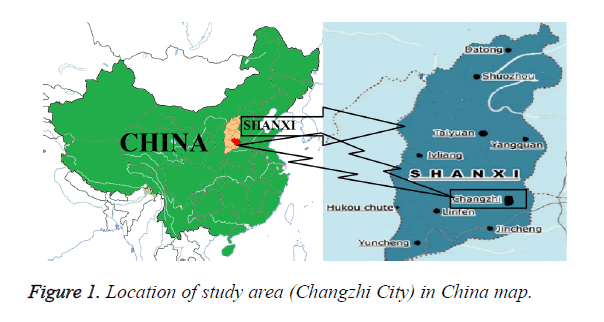
Shanxi (Chinese: ), one of the coastal province of the People's Republic of China, which is located in the northern part of China, with an area of 156000 km2 and a population of 35,712,111. Changzhi, one of the major cities of Shanxi (Chinese: ) province (36° 11′N 113° 06′E), is a part of the North China region as shown in Figure 1. The city is located in the north part of that province at between 36° 11′ northern latitude and 113° 06′ east of Greenwich. The city was one of the 36 administrative extant under the reign of the first emperor of a unified China. It has a continental monsoon climate. Its population and metropolitan area are 3,234,100 and 13,864 km2, respectively. The annual precipitation is near about 350-700 millimetres. Currently, Changzhi is a transportation centre in Shanxi. Convenient transportations are facilitated by 4 controlled-access highways (Taiyuan-Changzhi, Changzhi-Jincheng, Changzhi- Linfen, Changzhi-Handan), 2 railways (Taiyuan-Jiaozuo Railway and Handan-Changzhi Railway ), 3 national highways (China National Highway 207, 208 and 309) and 1 airport (Changzhi Wangcun Airport, ITAT Code: CIH, ICAO Code: ZBCZ). Internal transportation is also built with bus and taxi network.
Sampling of informants
This study was performed by the permission from the authority of Changzhi, Shanxi 046000. This ethnopharmacological survey was performed during January 2016 to May 2016. Three ground visits consisting of 6 days for each survey were performed. The focus of this study was traditional medicinal plant practitioners and local people with empirical knowledge on medicinal plants. Total 169 peoples were interrogated for this survey. During interview, the selection process is done by in the basis of informants, age, sexual category, as well as skill on practice of medicinal plants in various ailments.
Ethnomedicinal data collection
The data was collected with the help of a semi-structured questionnaire and the guided field-walk process. The record questionnaires dealt with individual information with age, sex, and educational conditions, skills on medicinal plants. It is also included subsequent information: (a) the name of the plants, (b) plants part/s used, (c) the mode of preparation, (d) plant types, (e) relative plenty at the region, (f) habitation of the plant species, (g) mode of application and (h) therapeutic uses of particular plant. In the guided field-walk method, interviews were conducted in Chinese, which was the language spoken and understood by traditional healers and the local peoples. Interviews are conducted during daytime and plant samples are collected, preserved, and later identified by the experts.
Data analysis
Current species information was organized in alphabetical order by scientific names along with the family, plant types, plant part used, mode of function, and mode of process, habit, habitat, and frequency of use.
Use value (UV)
Use Values (UV) are analysed for individual plants to provide a quantitative assess of its comparative importance to the informants purposely [17]. UV was calculated by this equation:
UVS = Σi UVis/ns
where ‘UVs’ indicates to the use value of a particular species, ‘UVis’ indicates to the number of use information mentioned by the informants for that particular medicinal plant species and ‘ns’ indicates to the entire number of informants that are interviewed. Usually UV is calculated to find out the level of therapeutic use for a particular plant species. Plant with wide healing uses or those that are broadly granted for the treat of a particular disease will gain a high UV.
Results and Discussion
Informants
There are total 169 informants are interviewed among them 39 were THPs and 130 were Indigenous people. Major informants were found male 59.13% compare to the 40.83% female. Considering the age major part of the informants were 51-60 years (29.58%) old and the other informants were 41-50 years (28.40%) old, followed by 30-40 years (22.48%) old, respectively as shown in Table 1.
| Factor | Categories | No. of person | % Of informants |
|---|---|---|---|
| Gender | Male | 100 | 59.17 |
| Female | 69 | 40.83 | |
| Age | 31-40 yr | 38 | 22.48 |
| 41-50 yr | 48 | 28.4 | |
| 51-60 yr | 50 | 29.58 | |
| 61-70 yr | 22 | 13.02 | |
| More than 70 yr | 11 | 6.51 | |
| Class | Indigenous people | 130 | 76.92 |
| Traditional Health Practitioners (THPs) | 39 | 23.08 | |
| Experience of Traditional Health Practitioners | Less than 3 yr | 3 | 7.69 |
| 3-6 yr | 5 | 12.82 | |
| 6-10 yr | 6 | 15.38 | |
| 10-15 yr | 12 | 30.77 | |
| 15-20 yr | 5 | 12.82 | |
| More than 20 yr | 8 | 20.51 |
Table 1. Classification of informants according to various factors.
Many THPs cultivated medicinal plants in front of their house. They collect the plants in a particular time or season. Some knowledgeable THPs also preserve their personal formulations in written documents. Now days, some literate THPs have been following the formulation book containing official herbal formularies published by China as well as India. THPs does not want to disclose their experienced as well as ethnopharmacological knowledge to public as a way of not to place their profession under risk by more practitioners. The knowledge of the THPs is inter-generational and perhaps has been gathered over the centuries and passed on from one generation to another generation [18]. However, the knowledge is transfer from parent to children, in many other societies around the world most of the practitioners prefer their son to convey their ethnopharmacological knowledge [16,19-23]. Practicing of medicinal plants by THPs is found in many families where their knowledge is being passed to their family members or generation by only seeing the seniors doing it.
Medicinal plants recorded
Through this current study, 71 plant species belonging to 44 families were documented which are used for the healing of various diseases in the study area. The maximum number of species (4 species) be member of Leguminosae and Rubiaceae afterward Lamiaceae, Apiaceae, Asparagaceae, Rosaceae, Orchidaceae, Cucurbitaceae, Asteraceae belongs to (3 species) as shown in Table 2.
| Family | No. of species | Family | No. of species |
|---|---|---|---|
| Leguminosae | 4 | Cornaceae | 1 |
| Rubiaceae | 4 | Hypoxidaceae | 1 |
| Lamiaceae | 3 | Convolvulaceae | 1 |
| Apiaceae | 3 | Dioscoreaceae | 1 |
| Asparagaceae | 3 | Ebenaceae | 1 |
| Rosaceae | 3 | Berberidaceae | 1 |
| Orchidaceae | 3 | Eucommiaceae | 1 |
| Cucurbitaceae | 3 | Polygonaceae | 1 |
| Asteraceae | 3 | Caprifoliaceae | 1 |
| Fabaceae | 2 | Asclepiadaceae | 1 |
| Liliaceae | 2 | Oleaceae | 1 |
| Rutaceae | 2 | Sapindaceae | 1 |
| Ranunculaceae | 2 | Solanaceae | 1 |
| Lauraceae | 2 | Moraceae | 1 |
| Araliaceae | 2 | Paeoninacaeae | 1 |
| Gentianaceae | 2 | Gramineae | 1 |
| Amaranthaceae | 1 | Polyporaceae | 1 |
| Alismataceae | 1 | Orobanchaceae | 1 |
| Anthericaceae | 1 | Schisandraceae | 1 |
| Aristolochiaceae | 1 | Selaginellaceae | 1 |
| Buddleiaceae | 1 | Typhaceae | 1 |
| Campanulaceae | 1 | Poaceae | 1 |
Table 2. Distribution of medicinal plant species of according to their family.
In the present study, high UVs observed for Gymnema sylvestre (1.92), Astragalus membranaceus (1.89), Zea mays (1.71), Salviae miltiorrhiza (1.70), and Rehmannia glutinosa (1.66) indicates their broad usage in the ethnobotanical practices in the survey area. Low UVs observed for Curculigo orchioides (0.18), Flos lonicerae (0.27), Buddleja officinalis (0.29), Asparagus cochinchinensis and Cinnamomum cassia (0.30) shown in Table 3. Those plants are enlisted as high UVs may be growing extensively in the study area that is why indigenous people and THPs of this region always use these plants in many ailment categories. Most of the cases roots are poured in water and taken orally in morning. The diabetic patients suggested by the THPs take fruits orally. In some cases, Meshed soup, and decoction of bark in the following morning on an empty stomach are taken orally. Having high UVs are an expression of the resourceful use of these plant species for the mentioned ailments [24].
| Serial No. | Scientific name | Family | Plant type | Parts used | Mode of administration | Frequency of usage | Use value |
|---|---|---|---|---|---|---|---|
| 1 | Achyranthes bidentata Bl. | Amaranthaceae | W, C, H | Root | (O) | 58 | 0.69 |
| 2 | Agrimonia pilosa Ledeb. | Rosaceae | W, H | Whole plant | (O) | 95 | 1.12 |
| 3 | Alisma orientalis (Sam.) Juzep. | Alismataceae | W, C, H | Tuber | (O) | 68 | 0.8 |
| 4 | Anemarrhena asphodeloides Bge. | Anthericaceae | W, H | Rhizome | (O) | 48 | 0.57 |
| 5 | Angelica sinensis (Oliv.)Diels | Apiaceae | W, H | Root | (O) | 150 | 1.6 |
| 6 | Asarum sieboldii Miq. | Aristolochiaceae | W, H | Rhizome | (O) | 20 | 0.36 |
| 7 | Asparagus cochinchinensis (Lour.) Merr. | Asparagaceae | W, H | Tuber | (O) | 17 | 0.3 |
| 8 | Astragalus membranaceus (Fisch) Bge.var.mongholicus (Bge.) Hsiao | Leguminosae | W, H | Root | (O) | 169 | 1.89 |
| 9 | Atractylodes lancea (Thunb.) DC. | Asteraceae | W, H | Rhizome | (O) | 23 | 0.41 |
| 10 | Atractylodes macrocephala Koidz. | Asteraceae | W, H | Rhizome | (O) | 58 | 0.69 |
| 11 | Buddleja officinalis Maxim | Buddleiaceae | W, S | Flower | (O) | 15 | 0.27 |
| 12 | Bupleurum chinese DC. | Apiaceae | W, H | Root | (O) | 112 | 1.33 |
| 13 | Caragana intermedia kuang et H. C. Fu | Leguminosae | W, S | Root | (O) | 34 | 0.4 |
| 14 | Cinnamomum cassia Nees ex Blume | Lauraceae | G, H | Dry Bark | (O) | 25 | 0.3 |
| 15 | Citrus medica L. | Rutaceae | G, H | Fruit | (O) | 38 | 0.44 |
| 16 | Clematis chinensis Osbeck | Ranunculaceae | W, H | Root, Rhizome | (O) | 40 | 0.47 |
| 17 | Codonopsis pilosula Nannf. | Campanulaceae | G, H | Root | (O) | 29 | 0.34 |
| 18 | Coptis chinensis Franch | Ranunculaceae | W, H | Rhizome | (O) | 54 | 0.64 |
| 19 | Cornus officinalis Sieb. et Zucc | Cornaceae | W, S | Fruit | (O) | 105 | 0.65 |
| 20 | Crataegus pubescens C. Presl | Rosaceae | W, C, T | Ripe fruit | (O) | 17 | 0.31 |
| 21 | Curculigo orchioides Gaertn | Hypoxidaceae | G, H | Rhizome | (O) | 10 | 0.18 |
| 22 | Cuscuta chinensis Lam. | Convolvulaceae | C, H | Seed | (O) | 27 | 0.32 |
| 23 | Dendrobium moniliforme (L.) Sw. | Orchidaceae | G, H | Whole plant | (O) | 132 | 1.56 |
| 24 | Dendrobium chrysanthum Wall. | Orchidaceae | W, H | Stem | (O) | 61 | 0.72 |
| 25 | Desmodium gangeticum | Fabaceae | W, S | Stem | (O) | 42 | 0.5 |
| 26 | Dioscorea opposita Thumb | Dioscoreaceae | W, H | Root | (O) | 118 | 1.4 |
| 27 | Diospyro skaki L. | Ebenaceae | W, T | Leaves, Fruit | (O) | 67 | 0.79 |
| 28 | Elephantopus scaber L. | Asteraceae | W, H | Whole plant, | (O) | 32 | 0.38 |
| 29 | Entada phaseoloides (L.) Merr | Leguminosae | W, V | Seed | (O) | 98 | 1.16 |
| 30 | Epimedium brevicornum Maxim | Berberidaceae | W, H | Leaves | (O) | 22 | 0.39 |
| 31 | Eucommia ulmoides Oliv. | Eucommiaceae | C, T | Bark | (O) | 19 | 0.34 |
| 32 | Fagopyrum cymosum (Trev.) Meisn. | Polygonaceae | W, H | Seed | (O) | 23 | 0.41 |
| 33 | Flos lonicerae | Caprifoliaceae | W, C, H | Flower | (O) | 12 | 0.23 |
| 34 | Gardenia jasminoides J. Ellis. | Rubiaceae | W, S | Fruit | (O) | 19 | 0.42 |
| 35 | Gymnema sylvestre (Retz.) Schult | Asclepiadaceae | W, H | Leaves | (O) | 169 | 1.92 |
| 36 | Gynostemma pentaphyllum (Thunb.) Mak. |
Cucurbitaceae | W, H | Stem, Leaves, | (O) | 43 | 0.51 |
| 37 | Ligusticum chuanxiong Hort. | Apiaceae | W, H | Root | (O) | 124 | 1.47 |
| 38 | Ligustrum lucidum W. T. Ait. | Oleaceae | W, T | Fruit | (O) | 25 | 0.31 |
| 39 | Litchi chinensis Sonn. | Sapindaceae | C, G, T | Seed | (O) | 137 | 1.62 |
| 40 | Liriope spicata (Thunb.) Lour. | Asparagaceae | W, H | Tuber, Root | (O) | 37 | 0.44 |
| 41 | Lycium barbarum L. | Solanaceae | W, S | Fruit | (O) | 84 | 0.99 |
| 42 | Malus toringoides (Rehd.) Hughes | Rosaceae | W, C, T | Leaves | (O) | 29 | 0.51 |
| 43 | Momordica charantia L. | Cucurbitaceae | C, G, V | Fruit | (O) | 38 | 0.45 |
| 44 | Morus alba L. | Moraceae | W, S | Fruit, Leaves and Root | (O) | 47 | 0.56 |
| 45 | Ophiopogon japocicus (Thunb.) Ker-Gawl. | Liliaceae | W, H | Root | (O) | 68 | 0.8 |
| 46 | Paeonia lactiflora Pall. | Paeoninacaeae | W, H | Root | (O) | 92 | 1.09 |
| 47 | Panax ginseng C. A.Meyer | Araliaceae | W, H | Root | (O) | 151 | 1.61 |
| 48 | Panax quinquefolium L. | Araliaceae | W, S | Root, Rhizome | (O) | 80 | 0.95 |
| 49 | Phellodendron amurense Rupr. | Rutaceae | W, T | Bark | (O) | 20 | 0.36 |
| 50 | Phragmites communis Trin. | Gramineae | W, H | Rhizome | (O) | 37 | 0.43 |
| 51 | Polygonatum odoratum (Mill.) Druce. | Liliaceae | W, H | Rhizome | (O) | 49 | 0.58 |
| 52 | Polygonatum sibiricum Redoute | Asparagaceae | G, W, H | Rhizome | (O) | 35 | 0.41 |
| 53 | Poria cocos (Schw.) Wolf | Polyporaceae | C, H | Bark | (O) | 138 | 1.64 |
| 54 | Prunella vulgaris L. | Lamiaceae | W, H | Whole plant | (O) | 111 | 1.31 |
| 55 | Pueraria lobata (Willd.) Ohwi | Fabaceae | C, V | Root | (O) | 87 | 1.03 |
| 56 | Ramulus cinnamomi | Lauraceae | W, H | Twig | (O) | 74 | 0.88 |
| 57 | Rehmannia glutinosa (Gaertn.) Li-bosch. | Orobanchaceae | C, H | Root | (O) | 140 | 1.66 |
| 58 | Salviae miltiorrhiza Bge. | Lamiaceae | C, H | Root | (O) | 159 | 1.7 |
| 59 | Schisandra chinensis (Turcz.) Baill. | Schisandraceae | W, V | Fruit | (O) | 35 | 0.41 |
| 60 | Scutellaria baicalensis Georgi | Lamiaceae | C, H | Root | (O) | 25 | 0.29 |
| 61 | Selaginella tamariscina (Beauv.) Spring | Selaginellaceae | W, H | Whole plant | (O) | 42 | 0.49 |
| 62 | Sophora flavescens Ait. | Leguminosae | W, S | Root | (O) | 59 | 0.69 |
| 63 | Spiranthes sinensis (Pers.) Ames | Orchidaceae | C, H | Whole Plant, Root | (O) | 23 | 0.41 |
| 64 | Swertia kouitchensis Franch. | Gentianaceae | W, H | Whole plant | (O) | 77 | 0.91 |
| 65 | Swertia macrosperma C.B. Clark | Gentianaceae | W, H | Whole plant | (O) | 92 | 1.08 |
| 66 | Trichosanthes kirilowii Maxim. | Cucurbitaceae | C, V | Root | (O) | 68 | 0.45 |
| 67 | Typha angustifolia L. | Typhaceae | W, S | Pollen | (O) | 21 | 0.37 |
| 68 | Uncaria cordata (Lour.) Merr | Rubiaceae | W, H | Hook | (O) | 43 | 0.47 |
| 69 | Uncaria laevigata Wall.ex G. Don | Rubiaceae | W, H | Stem, Bark, Hook | (O) | 68 | 0.71 |
| 70 | Uncaria tomentosa DC. | Rubiaceae | W, V | Bark | (O) | 94 | 1.11 |
| 71 | Zea mays L. | Poaceae | C, G, H | Tuber | (O) | 169 | 1.71 |
Table 3. List of medicinal plants used as traditional Chinese health care medicine in the treatment of diabetes by local residents of Changzhi.
Information regarding the preparation
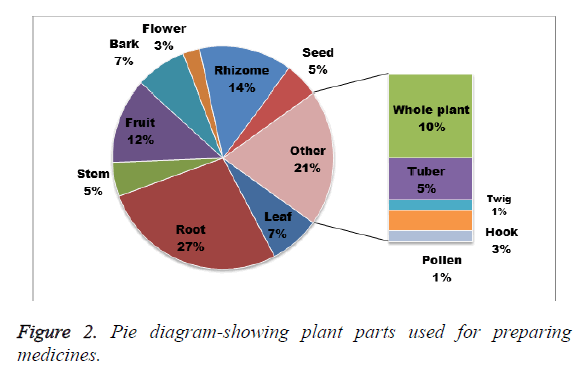
A variety of plant parts including root, leaf, seed, fruit, stem, flower, bark, tuber, whole plant twig, hook, pollen, and rhizome were found to be extensively used for the healing of different types of ailments. The most commonly used plant parts were roots (27%), followed by rhizome (14%), fruit (12%) and others are given in Figure 2. Ethnomedicinal practice has also been widely used and enlisted into several other ethnobotanical survey reports [25-28].
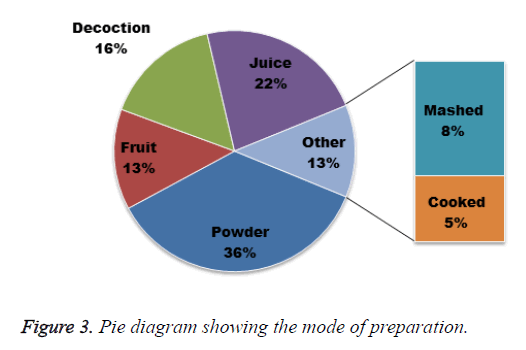
In view of the mode of preparation of herbal medicines, information contains powder, juice, fruit, and decoction. Among these, the main mode of preparation is powder (36%), followed by juice (22%); decoction (16%) and rest are given in Figure 3. Powder, juice, fruit, and decoction can regularly be found as one of the chief forms of medicine preparation in ethnobotanical practice as it is simple to prepare by amalgamation through water and other ingredients [29,30]. In many cases, the preparation mode also involves drying of the plant substances afterward crushing into fine powder. Water is usually used if a solvent is needed for the preparation. A little bit milk or honey is also used as a matrix or included as an adjuvant to mask smell or to augment viscosity of the solvent. Many people of this district often habitually add sugar, salt, banana, or lemon to enhance the palatability of a drug preparation. Paste is made by grinding plant pieces via mortar and grinder.
In many cases, THPs prepare drugs with the assist of several plant species for managing of a single disease. Adjuvants are often included to get better therapeutic property or to enhance the artistic value of the preparation. Poly herbal preparations are able to give better therapeutic power as a wide variety of bioactive mixes from diverse plants is used in the preparation [31].
Habit, habitat, and nature of the plants
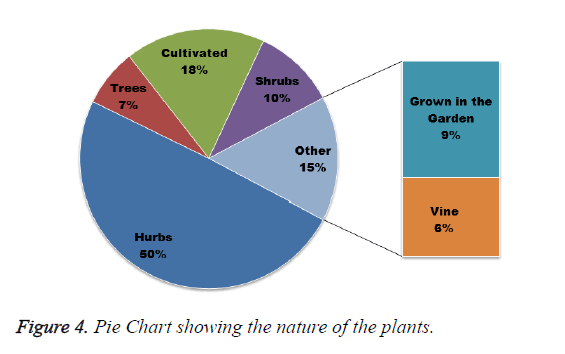
In the present study there are 71 identified therapeutically important plants are recorded, among them 76% are wilds.
Other species used is a member of herbs (50%), followed by cultivated plants (15%) and others are given in Figure 4. These medicinal plants can be found growing mainly in the jungle, riversides, and ponds side, roadside and homemade gardens. Therefore, the majority of the plant species documented in the present study grow up wild in that region. THPs used trees and herbs mainly as therapeutic due to their rapid accessibility in nature [22,29]. In accordance with local residents, some people supply plant materials to the herbal companies and pharmaceutical companies. They collect these plants from wild without paying any consideration to their conservation [32]. Though some of the enlisted plants are largely distributed in the present survey area, several of them are rare and reached in an extinction period due to the rapid deforestation or collecting them without any apprehension towards biodiversity protection. Therefore, rapid action from the authorities is essential for the proper cultivation and conservation of this therapeutically and commercially important and susceptible species.
Conclusion
The recent study gives a general expression of the medicinal plant use in Changzhi. There are 71 plant species are identified used for treating DM. There have a number of studies on medicinal plants of China, which give, emphasize such type of ethnomedicinal study in future in China [33-36]. Therefore, as this survey report will protect the medicinal plant practice of this area, some allegation can also be concluded from the study that comprises right steps for the propagation and protection of the medicinal plants containing the susceptible species, legalization of their use and proper patronization of the ethnobotanical practice to balance the less available modern medical facilities. This study finds a number of unique plant species for ethnomedicinal purposes against diabetes, which may contribute in future research, and development of new novel drugs.
Acknowledgments
We are very grateful to the Traditional Health Practitioners and indigenous people for sharing generously their knowledge of medicinal plants with us.
References
- Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010; 87: 4-14.
- Panunti B, Jawa AA, Fonseca VA. Mechanisms and therapeutic targets in type 2 diabetes mellitus. Drug Discover Today Dis Mech 2004; 1: 151-157.
- Kamenov ZA, Parapunova RA, Georgieva RT. Earlier development of diabetic neuropathy in men than in women with type 2 diabetes mellitus. Gend Med 2010; 7: 600-615.
- Hoffman WH, Helman SW, Passmore G. Acute activation of peripheral lymphocytes during treatment of diabetic ketoacidosis. J Diab Compl 2001; 15: 144-149.
- Chait A, Bornfeldt KE. Diabetes and atherosclerosis: is there a role for hyperglycemia? J Lipid Res 2009; 50 Suppl: S335-339.
- Inukai T, Fujiwara Y, Tayama K, Aso Y, Takemura Y. Serum levels of carboxy-terminal propeptide of human type I pro-collagen are an indicator for the progression of diabetic nephropathy in patients with Type 2 diabetes mellitus. Diab Res Clin Pract 2000; 48: 23-28.
- Romero AP, Fernandez BJ, Baget BM, Martinez SI, Mendez MI, Salvat SM, Buil CJA. Changes in the diabetic retinopathy epidemiology after 14 years in a population of Type 1 and 2 diabetic patients after the new diabetes mellitus diagnosis criteria and a more strict control of the patients. J Diab Compl 2009; 23: 229-238.
- Xu Y, Wang L, He J, Bi Y, Li M, Wang T, Wang L, Jiang Y, Dai M, Lu J, Xu M, Li Y, Hu N, Li J, Mi S, Chen CS, Li G, Mu Y, Zhao J, Kong L, Chen J, Lai S, Wang W, Zhao W, Ning G. 2010 China Non-communicable Disease Surveillance Group. JAMA 2013; 310: 948-959.
- Yang W, Zhao W, Xiao J, Li R, Zhang P. Medical care and payment for diabetes in China: enormous threat and great opportunity. PLoS One 2012; 7: e39513.
- Neves JM, Matos C, Moutinho C, Queiroz G, Gomes LR. Ethnopharmacological notes about ancient uses of medicinal plants in tras-os-Montes (northern of Portugal). J Ethnopharmacol 2009; 124: 270-283.
- Govaerts R. How many species of seed plants are there? Taxon 2001; 50: 1085-1090.
- Schippmann U, Leaman DJ, Cunninghan AB. Impact of cultivation and gathering of medicinal plants on Biodiversity: global trends and issues. Satel Commi Gen Res Food Agr Rome 2002.
- Rai LK, Prasad P, Sharma E. Conservation threats to some important medicinal plants of the Sikkim Himalaya. Biol Conserv 2000; 93: 27-33.
- Nanyingi MO, Mbaria JM, Lanyasunya AL, Wagate CG, Koros KB. Ethnopharmacological survey of Samburu district, Kenya. J Ethnobiol Ethnomed 2008; 4: 14.
- Calixto JB. Twenty-five years of research on medicinal plants in Latin America: a personal view. J Ethnopharmacol 2005; 100: 131-134.
- Teklehaymanot T. Ethnobotanical study of knowledge and medicinal plants use by the people in Dek Island in Ethiopia. J Ethnopharmacol 2009; 124: 69-78.
- Phillips O, Gentry AH, Reynel C, Wilkin P, Galvez-Durand BC. Quantitative ethnobotany and Amazonian conservation. Conserv Biol 1994; 8: 225-248.
- Jahan N, khan A, Hasan MN, Hossain MU, Das U, Sultana S, Rahmatullah M. Ethnomedicinal plants of fifteen clans of the garo tribal community of Madhupur in Tangail district, Bangladesh. Am Eur J Sust Agr 2013; 7: 188-195.
- Deribe K, Amberbir A, Getachew B, Mussema Y. A historical overview of traditional medicine practices and policy in Ethiopia. Ethiopian J Health Develop 2006; 20: 127-134.
- Giday M, Asfaw Z, Woldu Z. Medicinal plants of the Meinit ethnic group of Ethiopia: an ethnobotanical study. J Ethnopharmacol 2009; 124: 513-521.
- Panghal M, Vedpriya A, Sanjay Y, Sunil K, Jaya PY. Indigenous knowledge of medicinal plants used by Saperas community of Khetawas, Jhajjar District, Haryana, India. J Ethnobiol Ethnomed 2010; 6: 4.
- Uniyal SK, Singh KN, Jamwal P, Lal B. Traditional use of medicinal plants among the tribal communities of Chhota Bhangal, Western Himalaya. J Ethnobiol Ethnomed 2006; 2: 14.
- Parveen, Upadhyay B, Roy S, Kumar A. Traditional uses of medicinal plants among the rural communities of Churu district in the Thar Desert, India. J Ethnopharmacol 2007; 113: 387-399.
- Ayyanar M, Ignacimuthu S. Ethnobotanical survey of medicinal plants commonly used by Kani tribals in Tirunelveli hills of Western Ghats, India. J Ethnopharmacol 2011; 134: 851-864.
- Mahishi P, Srinivasa BH, Shivanna MB. Medicinal plant wealth of local communities in some villages in Shimoga District of Karnataka, India. J Ethnopharmacol 2005; 98: 307-312.
- Abo KA, Fred-Jaiyesimi AA, Jaiyesimi AE. Ethnobotanical studies of medicinal plants used in the management of diabetes mellitus in South Western Nigeria. J Ethnopharmacol 2008; 115: 67-71.
- Gonzalez JA, García-Barriuso M, Amich F. Ethnobotanical study of medicinal plants traditionally used in the Arribes del Duero, western Spain. J Ethnopharmacol 2010; 131: 343-355.
- Telefo PB, Lienou LL, Yemele MD, Lemfack MC, Mouokeu C, Goka CS, Tagne SR, Moundipa FP. Ethnopharmacological survey of plants used for the treatment of female infertility in Baham, Cameroon. J Ethnopharmacol 2011; 136: 178-187.
- Sanz-Biset J, Campos-de-la-Cruz J, Epiquien-Rivera MA, Canigueral S. A first survey on the medicinal plants of the Chazuta valley (Peruvian Amazon). J Ethnopharmacol 2009; 122: 333-362.
- Nadembega P, Boussim JI, Nikiema JB, Poli F, Antognoni F. Medicinal plants in Baskoure, Kourittenga Province, Burkina Faso: an ethnobotanical study. J Ethnopharmacol 2011; 133: 378-395.
- Teklehaymanot T, Giday M. Ethnobotanical study of medicinal plants used by people in Zegie Peninsula, northwestern Ethiopia. J Ethnobiol Ethnomed 2007; 3: 12.
- Khan MA, Islam MK, Siraj MA, Saha S, Barman AK, Awang K, Rahman MM, Shilpi JA, Jahan R, Islam E, Rahmatullah M. Ethnomedicinal survey of various communities residing in Garo Hills of Durgapur, Bangladesh. J Ethnobiol Ethnomed 2015; 11:44.
- Wang Z, Wang J, Chan P. Treating type 2 diabetes mellitus with traditional Chinese and Indian medicinal herbs. Evid Based Complement Alternat Med 2013; 2013: 343594.
- Tao X, Wang X, Jia W. Using Chinese natural products for diabetes mellitus drug discovery and development. Expert Opin Drug Discov 2007; 2: 977-986.
- Li W, Sun H, Zhou J, Zhang Y, Liu L, Gao Y. Antibacterial activities, antioxidant contents and antioxidant properties of three traditional Chinese medicinal extracts. Bangladesh J Pharmacol 2015; 10: 131-137.
- Zhang X, Liu Y, Xiong D, Xie C. Insulin combined with Chinese medicine improves glycemic outcome through multiple pathways in patients with type 2 diabetes mellitus. J Diabetes Invest 2015; 6:6: 708-715.