Research Article - Current Pediatric Research (2024) Volume 28, Issue 1
An audit of red cell transfusions in paediatric patients at tertiary care hospital.
Sandesh Pandurang Yemalwad*, Swarupa Nikhil Bhagwat
1Department of Transfusion Medicine, Seth GS Medical College and KEM Hospital Parel, Mumbai-400012 India
- Corresponding Author:
- Sandesh Pandurang Yemalwad
Department of Transfusion Medicine, Seth GS Medical College and KEM Hospital Parel, Mumbai-400012 India
E-mail: sandesh.yemalwad@gmail.com
Received: 25 December, 2023, Manuscript No. AAJCP-24-127651; Editor assigned: 27 December, 2023, Pre QC No. AAJCP-24-127651 (PQ); Reviewed: 10 January, 2024, QC No. AAJCP-24-127651; Revised: 18 January, 2024, Manuscript No. AAJCP-24-127651 (R); Published: 26 January, 2024, DOI:10.35841/0971-9032.28.01.1185-1189.
Abstract
Introduction: Blood transfusion is an integral part of modern health care system without which proper medical care may not be possible. Despite the availability of guidelines and protocols and sophisticated blood banking services worldwide, a high rate of inappropriate use of blood transfusion practices has been reported around the world, both in the developed and developing countries. Hence proper monitoring is necessary to control this indiscriminate use of blood and blood components. There are very few studies addressing the audit of transfusion practices exclusively in paediatric population. Hence this study was designed to evaluate the red blood cell transfusion practices of paediatric patients admitted in our tertiary care hospital with specialty and superspeciality departments in Western part of India and analyze the utilization pattern of red blood cell transfusion based on age group, gender and disease conditions requiring transfusion.
Materials and methods: A Retrospective study was conducted with 300 paediatric patients over a period of 18 months. In order to assess the appropriateness and inappropriateness and to assess the adequacy of documentation in case of Red blood cell transfusions. Statistical analysis: All data was analysed and calculated as descriptive statistics in the form of percentages out of total red cell transfusion episodes.
Results: Total 679 units of red cell were transfused in 300 consecutive episodes of red cell transfusion that were included in the study. The clinical specialty with the highest red cell transfusion episodes was paediatric medicine (82.33%) followed by neonatology (9.33%). Out of 300 red cell transfusion episodes, 132 (44%) episodes were appropriate in terms of indications and the dose transfused rest of the 168 (56%) were categorized to be inappropriate with only one adverse reaction was documented.
Conclusion: The study identified a high rate of irrational red blood cell transfusions and inadequacy of transfusion documentation. Regular transfusion audits and implementation of educational programs on rational use of blood components for the clinicians are recommended based on the findings of this study.
Keywords
Appropriateness, Red cell transfusion, Documentation
Introduction
Blood transfusion is an integral part of modern health care system. There are specific clinical conditions for which transfusion of blood and blood components form the mainstay of the treatment. However blood transfusion is associated with potential risks of acute and delayed complications including transfusion transmissible infections. In addition, human blood is a scarce and precious resource [1]. Therefore blood transfusion should be prescribed only to treat conditions associated with significant morbidity or mortality that cannot be prevented or managed sufficiently by other means [2]. Also, transfusion of blood and components in adequate and optimum doses is necessary to achieve the desired clinical outcome [3].
One of the important strategies of the World Health Organisation Blood Transfusion programme (WHO/BTS) is a reduction in unnecessary transfusion through the appropriate clinical use of blood and blood product, and the use of simple alternatives to transfusion, whenever possible [4].
Hence guidelines have been published by American association of blood banks, British committee for standards in haematology, Australian society of blood transfusion, world health organization to assist the clinicians in making the decisions regarding transfusion of blood and blood components. The AABB recommended guidelines on effective clinical use of red blood cell which assist clinician to make decision whether to transfuse or not. These guidelines elaborate on dose or amount of the red cell transfusion as well as on the indications and contraindications also. Furthermore, these guidelines recommend that clinical and laboratory response to transfusion of red blood cell should be monitored which will serve as a guide to further supportive care [5-7].
Additionally monitoring of patients during and after transfusion is necessary to detect any adverse reaction to transfusion [8]. Despite the availability of guidelines and protocols and sophisticated blood banking services worldwide, a high rate of inappropriate use has been reported around the world, both in the developed and developing countries [9,10]. Proper monitoring of blood transfusion practice is necessary to control this indiscriminate use of blood and blood components [11].
A variety of interventions have been used to monitor and to bring about changes in transfusion practices as per the guidelines. One of the most widely used interventions for this is audit and feedback, which is defined by the Cochrane effective practice and organization of care group as “any summary of clinical performance of health care over a specified period of time [12]. The knowledge gained from audit will not only rationalize the use of blood components but will also ensure availability of these products to the patients in whom transfusion is indicated as per the clinical condition. There are many studies available in the literature where the researchers have audited the practices of transfusions of blood and blood components. However, majority of the studies have been carried out in adult population predominantly auditing the transfusion practices of fresh frozen plasma and platelet concentrates [13,14]. There are very few studies addressing the audit of transfusion practices exclusively in pediatric population [15,16]. The physiology, pathophysiology, developmental stage, size, blood volume, and remaining life span of neonates, infants, and pediatric patients differ from adult’s population [17].
Hence this study was designed to evaluate the red blood cell transfusion practices of pediatric patients admitted in our tertiary care hospital with speciality and super speciality departments in Western part of India and analyze the utilization pattern of red blood cell transfusion based on age group, gender and disease conditions requiring transfusion.
Materials and Methods
The retrospective study was performed in the department of transfusion medicine of a tertiary care teaching hospital with specialty and super specialty service over a period of 18 months. Approval from the Institutional Ethics Committee was obtained for conducting the study. (Reference: IEC (I)/OUT/ 2043/17).
Inclusion criteria
• The patients from pediatric wards, paediatric intensive care unit, pediatric haematology section, neonatal intensive care unit and pediatric surgery wards were included.
• All the patients below 12 years of age.
Exclusion criteria
Children registered in thalassemia centre receiving regular transfusions as well as those receiving growth factors because they are more prone to develop allo-immunization as well as their pathophysiology and congenital cause which limits the effectiveness of red cell transfusion.
Sample size
The sample size was 300 patients who received red cell transfusions in the period from June 2016 to June 2017. Although some patients had received red blood cell transfusions more than once during the study period, only the first transfusion episode was included in the study for each patient.
Data collection
Requisitions received in the blood bank for transfusion of red cell concentrates were scrutinized to identify the patient population as per the inclusion criteria mentioned above. The records of these patients were traced further and data was collected from medical record department of the hospital.
The age and gender of patients and clinical specialties prescribing the red blood cell transfusions which were categorized into percentage of the total as per the gender and the age groups as infants (28 days to 1 year of age), neonates (1st day to 28 days), pediatrics (1 year to 12 years) and the clinical specialty.
Data for assessment of transfusion appropriateness:
• Patient’s weight,
• Clinical diagnosis,
• Indication and dose of red blood cell transfusion,
• Pre-transfusion haemoglobin and haematocrit.
The AABB guidelines were used to assess the appropropriateness of indications and dose. According to AABB guidelines adequate transfusion is red blood cell transfusion at a dose of 10-15 ml/kg which will increase the haemoglobin about 1-2 g/dl in neonates and pediatric patients [18].
The transfusion episode was considered appropriate if both the indication and dose transfused was as per the above guidelines. It was considered inappropriate if indication and/or dose were not as per the guidelines. Both the appropriate and inappropriate transfusion episodes were further analysed for the commonest indication in each clinical specialty [19].
Data for assessment of adequacy of documentation:
The following data was assessed for adequacy of documentation;
• The data mentioned above in “B” required for assessment of appropriateness of transfusion.
• Pretransfusion monitoring of vital parameters (Pulse rate, respiratory rate, blood pressure and temperature) of patient.
• Post-transfusion monitoring of vital parameters of the patient during transfusion and additionally for up to 24 hours after transfusion.
• Documentation of any adverse transfusion reaction which is defined as IgM antibodies (and in some rare cases IgG) that cause red cell destruction typically induce intravascular haemolysis through complement activation to the membrane attack complex.19. This typically presents as an acute hemolytic transfusion reaction.
• Assessment of transfusion outcome based on laboratory parameters: Post-transfusion hemoglobin and hematocrit.
• If any of these above data is not documented, it was categorized as inadequate documentation.
Statistical analysis
All data was analyzed and entered in Microsoft office excel 2007 format. The age group, gender, clinical specialty-wise distribution, appropriateness of transfusion and adequacy of documentation were calculated as descriptive statistics in the form of percentages out of total red cell transfusion episodes. Median was calculated for the dose of transfusion. The statistical analysis was used for interpretation of data.
Results
Total 679 units of red cell were transfused in 300 consecutive episodes of red cell transfusion that were included in the study. A transfusion across the three age group populations has been shown in Table 1.
| Age group | Total no of transfusion episodes (% of total) |
|---|---|
| Infant | 190 (63.33%) |
| Pediatric | 76 (25.33%) |
| Neonate | 34 (11.33%) |
| Total | 300 (100%) |
Table 1. Age wise distribution of red cell transfusion.
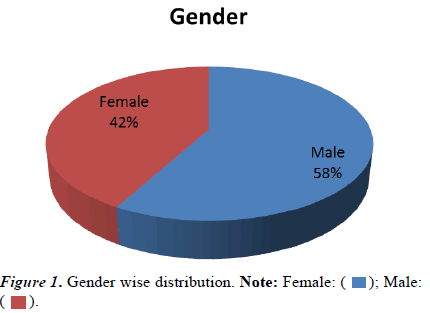
The percentage of gender wise distribution of red cell transfusion was shown in Figure 1.
The clinical specialty with the highest red cell transfusion episodes was mentioned in Table 2, whereas the specialty wise categorization of red cell transfusion appropriateness has been shown in Table 3. Table 4 shows the most common indications for appropriate and inappropriate transfusions for major user specialties.
| Clinical specialty | Total transfusion episodes in the specialty (% of total) |
|---|---|
| Pediatric medicine | 247 (82.33%) |
| Neonatology | 28 (9.33%) |
| Pediatric surgery | 14 (4.66%) |
| Cardiac surgery | 9 (3%) |
| Hematology | 2 (0.66%) |
| Total | 300 (100%) |
Table 2. Specialty wise usage of red cell transfusion.
| Clinical specialty | Total transfusion episodes in the speciality | Total appropriate transfusion episodes per speciality (% age) | Episodes with inappropriate dose or indications (i) | Episodes where appropriateness could not be decided (ii) |
|---|---|---|---|---|
| Total inappropriate transfusion episodes per speciality (% age) = (i) + (ii) | ||||
| Cardiac surgery | 9 | 4 (44.44%) | 1 (20%) | 4 (80%) |
| 5 (55.55%) | ||||
| Pediatric medicine | 247 | 115 (46.55%) | 93 (70.45%) | 39 (29.54%) |
| 132 (53.44%) | ||||
| Pediatric surgery | 14 | 8 (57.14%) | 0 (0%) | 6 (100%) |
| 6 (42.84%) | ||||
| Neonatology | 28 | 3 (10.71%) | 18 (72%) | 7 (28%) |
| 25 (89.28%) | ||||
| Hematology | 2 | 2 (100%) | 0 (0%) | 0 (0%) |
| 0 (0) | ||||
| 112/168 (66.66%) | 56/168 (33.33%) | |||
| Total | 300 | 132 (44%) | 168 (56%) | |
Table 3. Specialty-wise categorization of red cell transfusion appropriateness.
| Specialty | Common indication of appropriate transfusion | Common indication of inappropriate transfusion |
|---|---|---|
| Pediatric medicine | Anemia | Anemia not fulfilling the criteria of guidelines |
| Pediatric surgery | Anemia with Posted for surgery | Posted for surgery |
| Cardiac surgery | Anemia with posted for surgery | Posted for surgery |
| Neonatology | Anemia | Anemia not fulfilling the criteria of guidelines |
Table 4. The most common indications for appropriate and inappropriate transfusions for major user specialties.
Documentation and post-transfusion follow-up of red cell recipients
Overall documentation was assessed and found to be adequate in 213/300 (71%) of red cell transfusion episodes whereas in 87/300 (29%) of inadequately documented. The evaluation of post transfusion outcome was based on clinical and laboratory assessment such as pre transfusion hemoglobin, pre transfusion hematocrit and post transfusion hemoglobin, post transfusion hemoglobin.
Post-transfusion follow-up of patients was performed in 213/300 (71%) patients from different clinical specialties and shown clinical criteria was fulfilled according to the guidelines. Rest of 87/300 (29%) was found to be inadequate documentation so it could not be assessed. Out of 300 episodes, only one adverse reaction was documented in the post monitoring phase which included itching, fever and rash and due to inadequate documentation, the actual incidence of adverse reactions cannot be commented on.
Discussion
Transfusion of blood products is an essential and potentially lifesaving measure. However, it is a double edged sword as it may not always be beneficial to patients. Associated hazards like transfusion transmitted infections and other transfusion reactions require careful consideration to be given regarding decision to transfuse this invaluable resource. In India, majority of blood banks are individual hospital-based which perform the roles of both blood collection and transfusion centre. Indiscriminate use of blood/blood components is more likely in this setting due to easier availability of transfusion products and limited control over their appropriate use. Auditing of transfusion practices therefore becomes necessary. Our study was to evaluate red blood cell transfusion in pediatric patients through a retrospective audit.
Our study included total 679 units of red cell were transfused in 300 consecutive episodes of red cell transfusion. Out of 300 red cell transfusion episodes total number of appropriate was 132 (44%) episodes and that of inappropriate 168 (56%) episodes. In a recent study from a Karnataka medical college, out of the total 920 transfusion requests, only 36 (3.9%) were from pediatrics, mainly for anemia and exchange transfusion. In another Indian report from Dehradun, only 5.6% of all transfusion requests were from pediatrics. Thus, limited studies are available to analyze use of transfusion products in pediatric patients and their appropriateness from India.
There was a retrospective audit of transfusion practices in children at a tertiary care hospital in New Delhi. Clinical indications were reviewed according to BCSH guidelines. Among specific components, Whole blood transfusion was found to be most appropriate (82.9%) followed by transfusion of platelets (66.7%), RBCs (61.4%) and FFP (30.9%). Inappropriate requests were more common from pediatric intensive care units (69.3%) than from general wards. RBCs were most appropriately transfused in anemia (73.14%) and most inappropriately for surgeries (53.6%). Whole blood was most appropriately used for exchange transfusion and most inappropriately for blood loss (75%). However appropriateness of red blood cell transfusion in our study (46%) which was lower side as there were no classification of appropriateness and inappropriateness of total red blood cell transfusions [15].
Wade et al., in a observational study from pediatric services of a tertiary care hospital of Mumbai, found that maximum number of inappropriate transfusions were for FFP (58%), followed by RBC transfusions (35.5%). Only two (6.45%) platelets transfusions were in appropriate while none of cryoprecipitate transfusion was in appropriate. All in appropriate transfusions were in intensive care or surgical units while general pediatric wards had no inappropriate transfusion [2]. However, many other Indian studies have also included paediatric patients while assessing the transfusion needs and appropriateness in various hospitals.
Makroo et al., conducted another retrospective study to evaluate transfusion practices in the medical intensive care units of a tertiary care hospital in New Delhi. Out of 1817 ICU admissions over one year study period, 911 (50.1%) patients received blood components transfusion, including packed red blood cells (43.8%), FFP (18.3%) and platelets (8.4%). Some patients received multiple products. In this analysis, 21.4% of packed cell, 14.46% of FFP and 19% of platelet transfusions were found to be inappropriate [20].
Thus, there continues to be general but unfounded enthusiasm for red blood cell usage across a range of clinical specialties leading to shortage of the component as well as posing the patients to the risks of adverse effects of transfusion. The list of transfusion reactions in pediatric patients includes acute and delayed haemolytic transfusion reactions, Febrile Nonhemolytic Transfusion Reaction (FNHTR), allergic reaction, Transfusion-Related Acute Lung Injury (TRALI), Transfusion-Associated Circulatory Overload (TACO), and isolated hypotension.
Vossoughi et al., observed that pediatric transfusion reaction rate of 538 per 100,000 transfusions was significantly higher than the adult reaction rate of 252 per 100,000 transfusions. More than half 54.6% of pediatric transfusion reactions were associated with red blood cell transfusions, as were 64.1% of adult transfusion reactions and within the pediatric population allergic reactions to red blood cells were the most frequently reported reaction types [21]. In our study, out of 300 episodes only one adverse reaction documented in the post monitoring phase which includes itching, fever and rash [22]. The studies were done showed that inappropriate use of blood component transfusion may lead to numerous different adverse events including volume overload, Transfusion Related Acute Lung Injury (TRALI), transfusion transmitting infections and allergic reactions [23,24].
The clinical specialty with the highest red cell transfusion episodes was in pediatric medicine (82.33%) followed by neonatology (9.33%). The most common indication of inappropriateness of both speciality was anaemia not fulfilling the criteria of guidelines. Hence clinical reassessment to determine the need for further transfusion is appropriate. This reassessment also guides the decision on whether to retest the haemoglobin level [4]. RBC transfusion should not be dictated by Hb concentration alone, but also be based upon assessment of the patient clinical status [25]. In concern of anemia WHO stated that blood transfusion is used to relieve the clinical signs or respiratory distress, it is not a cure for anemia, but the underlying cause of the anemia still needs to be investigated and treated [4].
Another common inappropriate indication of transfusion in our study was that patient was posted for surgery this was compared to another study which indicates that preoperative blood order protocols for paediatric open heart surgery can be procedure specific. Patient age is less predictive of transfusion numbers. Because a large proportion of transfusions at our institution were given in the immediate postoperative period, orders should be designed to cover blood needs transfusion, particularly in the postoperative period, may eliminate any differences between surgeons and patients [26].
In addition to these, we also came across transfusion episodes where indications and/or amount transfused were not documented. This was observed in 34/300 (11.33%) and found to be inadequate documentation so it could not be assessed. Suboptimal transfusion documentation remains problematic and is highly correlated with non-justifiable transfusions [27]. Appropriate documentation is beneficial in assessing transfusion justification within established guidelines [28]. Hence inadequately documented transfusion episodes were considered inappropriate in terms of dose and or indications. Monitoring of transfusions ensures safety of transfusion episodes. Moreover, follow up of clinical and laboratory parameters following transfusions indicates degree of effectiveness, serves as a guide to further supportive care and may help in refining the existing guidelines of transfusion [23,29].
Earlier studies have shown positive correlation between the lack of clear documentation regarding rationale of transfusion with the lack of follow up after transfusion and ability to justify such transfusions during retrospective audits of transfusion [27,28]. We could not assess this correlation due to insufficient number. The findings of red blood cell transfusion audit indicate need for further analysis and implementation of changes in transfusion practices. Lack of awareness of transfusion guidelines for red cell usage has been reported to be the most common reason for inappropriate transfusions in previous studies [29]. Educational interventions in the form of regular seminars, discussions in the hospital transfusion committee; and training programs for clinicians and postgraduate students can have positive impact on transfusion practices and optimal use of blood components.
Transfusion audits are important tools to assess the transfusion needs of the local population, detect inappropriate transfusion practices and identify bottlenecks in blood components supply chain, to ensure timely remedial measures. The strength of our research is that we audited the adequacy of monitoring and follow of up of red cell recipients as well as indications, adverse event, documentation and amount of dose transfused. Majority of the other studies have emphasized upon the appropriateness of red cell transfusions [30]. Moreover, the data indicates that most of the published audits of red cell usage in India are from the northern part of the country. However, the major hindrance to the transfusion audit was poor documentation, which is a known limitation of retrospective audits [28]. We could not assess the actual effectiveness of red cell transfusions due to inadequacy of data because of insufficient documentation. Hence, we plan to perform prospective and concurrent audits of usage of all the blood components in future to overcome this limitation.
Conclusion
The study identified a high rate of irrational red blood cell transfusions and inadequacy of transfusion documentation. Regular transfusion audits and implementation of educational programs on rational use of blood components for the clinicians are recommended based on the findings of this study. It is necessary to remember that to reap maximum benefits from audits documentation needs to be judiciously maintained. All pertinent patient details must be entered for both prospective and retrospective audits. Clinicians should adhere to guidelines and not be swayed by clinical backdrop of patients.
References
- Zimmermann R, Büscher M, Linhardt C, et al. A survey of blood component use in a German university hospital. Transfusion 1997; 37: 1075-1083.
- Wade M, Sharma R, Manglani M. Rational use of blood components-An audit. Indian J Hematol Blood Transfus 2009; 25(2): 66-69.
- Theresa Nester MD, Shweta Jain MD. Hemotherapy decisions and their outcomes. In: AABB. 2012: 500.
- Sharma Richa JC. An audit of appropriate use of blood components in tertiary care hospital. Int J Med Sci Educ 2015; 2(3): 94.
- Nathan DG, Oski FA. Hematology of infancy and childhood. (3rd edn) 1998; 1560-1566.
- Robert Kliegman M, Joseph W. Risk of blood component transfusions. Nelson textbook of pediatrics. (17th edn) 2003:1646-1650.
- Michael M, Maynard K. Administration of blood components. 2012: 553.
[Crossref]
- Pinkerton PH. Blood bank audit. J Clin Pathol 1995; 48(4): 283-286.
- Martí-Carvajal AJ, Muñoz-Navarro SR, Peña-Martí GE, et al. An audit of appropriate use of blood products in adult patients in a Venezuelan general university hospital. Int J Qual Heal Care 1999; 11(5): 391-395.
- Mollison PL, Engelfriet CPO. Blood transfusion in clinical medicine. (9th edn) Oxford, Blackwell Scientific Publication 1993: 150-161.
- Alan T, Simon S. Approaches to blood utilization auditing. 2012:699.
- Mozes B, Epstein M, Ben-Bassat I, et al. Evaluation of the appropriateness of blood and blood product transfusion using preset criteria. Transfusion 1989; (29): 473-476.
- Tuckfield A, Haeusler MN, Grigg AP. Reduction of inappropriate use of blood products by prospective monitoring of transfusion request forms. Med J Aust 1997; (167): 473-476.
- Bahadur S, Sethi N, Pahuja S, et al. Audit of pediatric transfusion practices in a tertiary care hospital. Indian J Pediatr 2015; 82(4): 333-339.
- Ali AM, Décary F, Blajchman MA. Evaluation of pediatric transfusion practice using criteria maps. Transfusion 1991; 31(1): 52-58.
- Hillyer CD, Mondoro TH, Josephson CD, et al. Pediatric transfusion medicine: Development of a critical mass. Transfusion 2009; 49(3): 596-601.
- Carson JL, Grossman BJ, Kleinman S, et al. Cell transfusion : A clinical practice guideline from the AABB. 2012.
- James Zimring C, Steven L, Spitalnik M. Molecular biology and immunology in transfusion medicine. 2012: 253.
- TS V. A prospective audit of blood transfusion requests in RL Jalappa hospital and research centre for blood and blood components. J Blood Lymph 2012; 02(03): 2-4.
- Makroo RN, Mani RK, Vimarsh R, et al. Use of blood components in critically ill patients in the medical intensive care unit of a tertiary care hospital. Asian J Transfus Sci 2009; 3(2): 82-85.
- Vossoughi S, Perez G, Whitaker BI, et al. Analysis of pediatric adverse reactions to transfusions. Transfusion 2018; 58(1): 60-69.
- Shinagare SA, Angarkar NN, Desai SR, et al. An audit of fresh frozen plasma usage and effect of fresh frozen plasma on the pre–transfusion international normalized ratio. Asian J Transfus Sci. 2010;2(4):128-132.
- Nagarekha K. Evaluation of fresh frozen plasma usage at a medical college hospitalA two year study. Int J Blood Transfus Immunohematol 2012; 2: 16-20.
- Varghese R, Gomathi G. Audit of use of blood and its components in a tertiary care center in South India. Asian J Transfus Sci 2012; 6(2): 189.
- Chambers LA, Cohen DM, Davis JT. Transfusion patterns in pediatric open heart surgery. Transfusion. 1996; 36(2): 150-154.
- Madrigal E, Prajapati S, Avadhani V, et al. Adequacy of physician documentation and correlation with assessment of transfusion appropriateness: A follow-up study in the setting of prospective audits and patient blood management. Transfusion 2017; 57(2): 367-375.
- Gilmore S, Friedman A. Patient inclusion in transfusion medicine : Current perspectives. Published online 2015:7-16.
- Bhagwat SN, Sharma JH. A retrospective audit of appropriateness and monitoring of fresh frozen plasma transfusions in a tertiary care hospital. 2017; 4(7): 1562-1567.
- Spradbrow J, Cohen R, Lin Y, et al. Evaluating appropriate red blood cell transfusions: A quality audit at 10 Ontario hospitals to determine the optimal measure for assessing appropriateness. Transfusion 2016; 10(56): 2466-2476.
- Manuel Quintana D, Alberto Borobia M, José García Erce A, et al. Appropriate use of red blood cell transfusion in emergency departments: A study in five emergency departments. Blood Transfus 2017; 3(15): 199-206.
 ); Male:
(
); Male:
( ).
).