Research Article - The International Tinnitus Journal (2023) Volume 27, Issue 1
Adenoidectomy and Endoscopic Myringotomy with and without ventilation tube insertion for Treatment of Otitis Media with Effusion in 6-12 years old Children
1Department of Surgery-otolaryngology, College of Medicine, University of Baghdad, Baghdad, Iraq
2Department of Radiology, Al-immamain Al-kadimain Medical City, Baghdad, Iraq
Send correspondence to:
Dr. Ahmed Muhei Rasheed
Department of Surgery-Otolaryngology, College of Medicine, University of Baghdad, Baghdad, Iraq, Tel: 7713293222. E-mail: ahmed.muhei@comed.uobaghdad.edu.iq
Paper submitted on February 25, 2023; and Accepted on March 30, 2023
Citation: Rasheed AM, Abbas AM, Hilal SA, Homadi NJ. Adenoidectomy and Endoscopic Myringotomy with and without ventilation tube insertion for Treatment of Otitis Media with Effusion in 6-12 years old Children. Int Tinnitus J. 2023;27(1):27-33.
Abstract
Background: Otitis Media with Effusion (OME) is frequently caused by adenoiditis in children. OME is arguably one of the most common disorders that impairs hearing, speech development, and causes learning issues as a result. However, treatment options are debatable.
Aim: This study aims to evaluate if inserting a ventilation tube in conjunction with adenoidectomy is significantly superior to adenoidectomy in conjunction with myringotomy alone in terms of hearing outcome in 6-12 years old children with OME.
Patients and Methods: In this prospective controlled clinical study, 33 children; 66 ears, with ages ranging from 6-12 years (19 males and 14 females) diagnosed as cases of bilateral OME and varying degrees of adenoid hypertrophy were included. The patients were randomized into two groups; group I (17 patients; 34 ears) underwent adenoidectomy and endoscopic myringotomy alone, whereas the 16 patients;32 ears, in group II underwent adenoidectomy and endoscopic myringotomy together with ventilation tube insertion. Measurement of pure tone hearing threshold was achieved pre-operatively and at the end of 1st and 3rd postoperative months. The means of the pure tone hearing threshold averages of the patients in both groups were compared. Independent samples t-test was used to define the association between the two means.
Results: Pre-operatively, the means of pure tone hearing threshold averages were 27.3 ± 2.670 dB in group I patients and 29.5 ± 2.865 dB in group II patients. At the end of 1st and 3rd post-operative months, the pure tone hearing threshold average means in group I patients were 18.2 ± 2.689dB and 14.8 ± 2.735 dB respectively, while the means in group II patients were 10.6 ± 1.742 dB and 3.5 ± 1.158 dB respectively. Independent samples t-test revealed a statistically significant difference between group I and group II patients regarding the means of pure tone hearing threshold averages at the end of the 1st and the 3rd post-operative months (P value=0.015 and 0.003 respectively).
Conclusion: In terms of hearing level, ventilation tube insertion in conjunction with adenoidectomy is statistically superior to adenoidectomy with myringotomy alone in the treatment of OME.
Introduction
Otitis media with effusion (OME) is a condition in which there is accumulation of fluid in the middle ear without any acute infection-related signs and symptoms. As the fluid builds up in the middle ear, it causes pressure on the tympanic membrane. The pressure affects the normal tympanic membrane vibration, decreases sound conduction, and therefore causes decreased hearing [1]. OME is one of the most common childhood infectious diseases and is the most frequent cause of acquired hearing loss in childhood [2]. Between the ages of 3 and 10 years, about 20%-50% of children will experience an OME episode [3]. OME in children, especially recurrent and chronic OME, can have an impact on their hearing and language leading to verbal disabilities and also behavioral disorders [4]. Risk factors for OME include passive smoking, bottle feeding, daycare nursery, and atopy [5]. The most important etiologic factor in the development of OME is eustachian tube dysfunction; the second etiologic theory postulates that otitis media is caused by inflammation [3].
Watchful waiting for three months is a first-line measure in the treatment of OME. Surgical treatment options are considered in persistent cases [6]. A variety of drugs have been attempted for the treatment of OME including antibiotics and steroids. Oral antibiotics are useful in treating OME in the short-term but there is no evidence of long-term usefulness. The use of oral steroids has shown some benefits, but it is unknown whether these benefits are significant clinically [7,8]. Inserting a ventilation tube can be a successful procedure to improve hearing [9]. Some Complications may occur as a result of ventilation tube insertion.
The current study aims to evaluate if inserting a ventilation tube in conjunction with adenoidectomy is significantly superior to adenoidectomy in conjunction with myringotomy alone in terms of hearing outcome in 6-12 years old children with OME.
Methodology
Ethical considerations were obtained according to Helsinki Declaration. Informed written consent was obtained from the parents after explaining the nature of the study. The approval of the ethics committee was obtained from the Health Ethics Committee in the college of medicine, university of Baghdad.
This is a prospective controlled clinical study was enrolled on 33 children (66 ears); 19 males and 14 females, diagnosed as cases of bilateral OME and varying degrees of adenoid hypertrophy attending the department of otolaryngology at Al-jerahat Teaching Hospital in Medical City, Baghdad, Iraq, during the period from November 2019 to October 2022.
A full history and otorhinological examination including otoscopy and fiberoptic nasal endoscopy were performed. All patients were sent to audiometry, tympanometry, and post-nasal space x-ray (Figures 1 and Figure 2). The tympanometry results were classified into types A, B, and C according to Modified Jerger Classification.
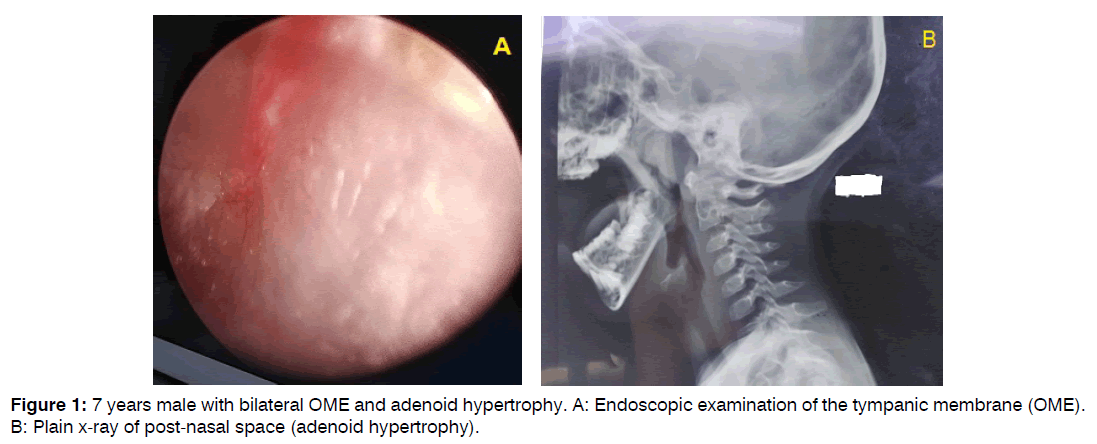
Figure 1: 7 years male with bilateral OME and adenoid hypertrophy. A: Endoscopic examination of the tympanic membrane (OME). B: Plain x-ray of post-nasal space (adenoid hypertrophy).

Figure 2: 8 years female with bilateral OME and adenoid hypertrophy. A: Pure tone audiogram (mixed hearing loss). B: Flat tympanogram.
The patients included in the current study were those with ages ranging from 6-12 years diagnosed as cases of bilateral OME (pure tone hearing threshold average more than 20 dB HL within frequencies 0.5, 1, 2, and 4 KHz with type B tympanogram) and varying degrees of adenoid hypertrophy. Patients excluded from the study were those with current upper respiratory tract infection or ear infection, bleeding tendency diseases, immunocompromised diseases e.g, diabetes mellitus, and congenital diseases e.g Cleft palate, Down syndrome, Kartagener syndrome, or Young syndrome.
Each patient who met the inclusion criteria was given a code number. Odd numbers were given to the 17 patients in group I, while the 16 patients in group II were given double numbers. The 17 patients; 34 ears, in group I were treated with adenoidectomy and endoscopic myringotomy alone, while the 16 patients; 32 ears, in group II were subjected to adenoidectomy and endoscopic myringotomy with ventilation tube insertion (Figure 3).

Figure 3: Ventilation tube insertion in the right ear of 10 years male with bilateral OME (suction shows sticky fluid in the middle ear).
The patients were followed-up by otoscopic examination for 3 months. At the end of the 1st and 3rd postoperative months, the pure tone audiometry was repeated. The means of the pure tone hearing threshold averages of the patients in both groups were compared using Independent samples t-test to define the association between the two means.
Surgical Procedures: General anesthesia was administered via an oral endotracheal tube. Using an otoscope with a camera and display system, a radial incision; myringotimy, was made in the anteroinferior portion of the tympanic membrane using Agnes Myringotom and middle ear fluid was suctioned. Shepard ventilation tube was placed in group II patients only. Adenoidectomy was done by using St. Clair-Thomsen curate while the patient was in the neutral position, and packing was used to ensure hemostasis. In patients who underwent tonsillectomy, a sandbag was placed under the shoulders; so extending the neck, tonsillectomy was done by dissection method and hemostasis was secured by packing and ligations.
Statistical Analysis: Statistical analysis was done by using the statistical package for social sciences version 23. Independent samples t-test was used to define the association between the two means. The Chi-square test was used to define the association between the categorical variables. The confidence level of 95% was set and a P-value <0.05 was considered significant.
Results
The patients included in this study were 33 patients; 66 ears, with ages ranging from 6-12 years (mean= 8.48 years ± SD 2.07). 19 patients (57.6%) were males and 14 patients (42.4%) were females, with a male: female ratio =1.4:1. There was no significant difference between both groups regarding age and gender(P-value > 0.05) as shown in tables 1 and 2 respectively.
| Group | Number & % | Minimum | Maximum | Mean ± SD | P-value | |
|---|---|---|---|---|---|---|
| Age (years) | Group I | 17 (60.6%) | 6 | 12 | 8.11 ± 1.93 | 0.412 |
| Group II | 16 (39.4%) | 6 | 12 | 8.87 ± 2.21 | ||
| Total | 33 (100%) | |||||
Table 1: Distribution of patients according to age (number=33).
| Group | Males | Females | Chi-square test value | P-value | |
|---|---|---|---|---|---|
| Gender | Group I | 10 | 7 | 0.022 | 0.881 |
| Group II | 9 | 7 | |||
| Total | 19 | 14 | |||
Table 2: Distribution of patients according to gender (number=33).
Hearing impairment was the chief complaint in the 33 patients included in this study (100%), other symptoms were nasal obstruction, snoring, and impaired speech as shown in table 3. Table 4 shows the pre-operative otoscopic examination signs.
| Symptoms | Group I | Group II | Chi-square test value | P-value |
|---|---|---|---|---|
| Hearing impairment | 17 (100%) | 16 (100%) | 0.000 | 1 |
| Nasal obstruction/snoring | 14 (82.4%) | 11 (68.8%) | 0.830 | 0.362 |
| Impaired speech | 2 (11.8%) | 4 (25%) | 2.254 | 0.324 |
Table 3: Patient symptoms (number=33).
| Otoscopic signs | Group A (34 ears) | Group B (32 ears) | Chi-square test value | P-value | |
|---|---|---|---|---|---|
| Tympanic membrane color | Red | 28 (82.4%) | 24 (75%) | 0.533 | 0.465 |
| Yellow | 6 (17.6%) | 8 (25%) | 1.348 | 0.246 | |
| Foreshortened handle of malleus | 26 (76.5%) | 28 (87.5%) | 0.626 | 0.429 | |
| Air bubbles | 4 (11.8%) | 6 (18.8%) | 0.607 | 0.436 | |
| Hair sign | 4 (11.8%) | 2 (6.3%) | 0.607 | 0.436 | |
Table 4: Pre-operative otoscopic examination (number=64 ears).
There was no significant difference between group I and group II patients regarding the pre-operative means of pure tone hearing threshold averages within 0.5, 1, 2, and 4 KHz as shown in table 5. Preoperatively, the tympanogram in all patients included in this study were type B; flat tympanogram.
| Pre-operative Pure tone hearing threshold means ± Std. Deviation (dB) | Independent samples t-test | P value | |
|---|---|---|---|
| Group I (34 ears) |
Group II (32 ear) |
||
| 27.3 ± 2.670 | 29.5 ± 2.865 | 0.055 | 0.816 |
Table 5: Pre-operative means of pure tone hearing threshold averages whithin 0.5, 1, 2, and 4 KHz. (number=66 ears).
12 patients in group I were subjected to myringotomy and adenoidectomy and 5 patients underwent myringotomy and adenotonsillectomy. In group II, 13 patients were subjected to myringotomy with ventilation tube insertion and adenoidectomy, and 3 patients underwent myringotomy with ventilation tube insertion and adenotonsillectomy. Statistically, there was no significant difference between group I and group II regarding tonsillectomy performance (Chi-square test=0.510; P-value=0.475. Table 6 shows the distribution of the patients according to the surgical procedures performed.
| Surgical procedures | Group I | Group II |
|---|---|---|
| Myringotomy and adenoidectomy | 12 (70.6%) | - |
| Myringotomy and adenotonsillectomy | 5 (29.4%) | - |
| Myringotomy with ventilation tube and adenoidectomy | - | 13 (81.25%) |
| Myringotomy with ventilation tube and adenotonsillectomy | - | 3 (18.75%) |
| Total | 17 (100%) | 16 (100%) |
Table 6: Types of surgical procedures (number=33).
Regarding the otoscopic findings, statistical analysis showed a significant difference between both groups in 2 otoscopic signs only; red tympanic membrane and foreshortened handle of malleus, as shown in tables 7 and 8.
At the end of the 1st and 3rd post-operative months, there was a significant difference between group I and group II patients in terms of improvement of the means of the pure tone hearing threshold averages within 0.5, 1, 2, and 4 KHz, the improvement was greater in group II patients. The difference in the improvement was more significant at the end of the 3rd post-operative month (P-value<0.005) than the improvement at the end of the 1st post-operative month (P-value< 0.05) as shown in table 9.
Discussion
OME one is of the most frequent diseases causing hearing impairment in children. However, still there is controversy regarding the treatment of OME. In this study, adenoidectomy was performed in all patients. Perhaps, adenoidectomy can open up the nasopharyngeal airway and relieves pressure on the eustachian tube’s nasopharyngeal orifices which allow for better middle ear cleft ventilation. Furthermore, adenoidectomy can remove the possible reservoir of pathogenic bacteria which can play an important role in the development of chronic OME. Emaneini et al. mentioned that adenoid hypertrophy may play an important role in the pathogenesis of OME, it may cause mechanical obstruction of the eustachian tube and can act as a reservoir of pathogenic bacteria [10]. Several studies have demonstrated the role of biofilms in the pathogenesis of OME [11-13]. It was shown that children with OME who were scheduled for adenoidectomy and myringotomy with or without the insertion of a tympanostomy tube had significantly less post-operative time with middle ear effusion than those who were treated with myringotomy or tympanostomy tube alone without an adenoidectomy [14, 15].
Since some adverse effects may result from ventilation tube insertion, it is important to know whether myringotomy is equally as effective as ventilation tube insertion in the treatment of children with OME [16]. In the present study, two surgical approaches for the treatment of children with bilateral OME and adenoid hypertrophy were compared. The current study showed that there was a statistically significant difference in the improvement of hearing thresholds between children treated with adenoidectomy and myringotomy with ventilation tube insertion and those who were treated with adenoidectomy and myringotomy alone, the improvement in pure tone hearing threshold average was greater in patients who subjected to adenoidectomy and myringotomy with ventilation tube insertion. The early closure of myringotomy in group I patients in comparison to group II patients who were treated with ventilation tube insertion which kept the middle ear ventilated for a longer period may explain the result. In the current study, the difference in the improvement of the pure tone hearing threshold averages between both groups was more significant at the end of the 3rd post-operative month (P value>0.005) than the difference in the improvement at the end of the 1st post-operative month (P value>0.05). Mandel et al., demonstrated that ventilation tubes ventilate the middle ear for a few months, but myringotomy alone is useless for treating chronic OME since the incision closes within a few days [17, 18]. However, progressive spontaneous resolution might also play a role. When the resolution is indicated by a change from type B to type A/C1 in the tympanogram, 25% of newly discovered OME of unknown prior duration in children resolves by 3 months (peak pressure more than 200 dapa) [19, 20].
According to Technology Assessment in Health Care, there is convincing evidence that ventilation tubes temporarily improve hearing (up to 9 months) [21]. According to Vlastos et al., in children older than 3 years with OME, tympanostomy tube insertion leads to a short-term improvement in hearing threshold compared to simple myringotomy [22]. Rosenfeld et al., advised ventilation tube insertion as an initial surgery because randomized trials had revealed a mean 62% relative decline in effusion prevalence [23] Grommet insertion, according to Rovers et al., improves hearing levels by a mean of 12 dB [24]. Adenoidectomy and ventilation tube insertion, in children with adenoid hypertrophy and recurrent OME, can significantly reduce the recurrent rate and shorten the time of middle ear effusion [25].
Many studies have shown that the improvement in hearing thresholds in children with OME treated with grommet insertion is temporary. According to the study done by Khodaverd et al. myringotomy with or without ventilation tube insertion does not affect the long-term hearing level in the treatment of children with chronic OME [26, 27]. However, restoration of normal hearing in patients with OME can be achieved by insertion of ventilation tubes that are correctly placed and remain patent, but in the long-term, they do not affect the hearing threshold after they fall or are removed [21, 28].
On the other hand, some studies had shown different results. Lous et al., mentioned that the benefits of ventilation tube insertion in children with OME on hearing is small and diminished during the first year [29]. In a study conducted by Gates et al., they concluded that adenoidectomy in conjunction with myringotomy and tympanostomy tube insertion has equivalent efficacy to adenoidectomy plus myringotomy alone in the treatment of OME in 4 years children or older [14]. Tao et al., recommended adenoidectomy plus myringotomy as the first choice surgical treatment of [4-12] years children with adenoid hypertrophy and OME to avoid complications after ventilation tube insertion without increasing the risk of long-term recurrence [30].
In a study conducted by Zhang and Fu on 312 children (556 ears) with OME, they allocated the children in 3 groups, drug treatment group: mild hearing loss; myringotomy group: mild, moderate or severe hearing impairment and rarefied fluid in the tympanic cavity; ventilation tube insertion group: mild, moderate or severe hearing impairment and sticky or jelly fluid in the tympanic cavity. They found that the effective rates were 95.6% in the drug treatment group, 89.6% in the myringotomy group, and 90.9% in the ventilation tube insertion group. Statistical analysis showed no significant difference among the 3 groups, they concluded that the treatment of OME in children should not only be combined with disease course but also combined with different hearing loss and the characteristics of effusion in the tympanic cavity [31].
Conclusion
In this study, we concluded that insertion of a ventilation tube in conjunction with adenoidectomy is statistically significantly superior to adenoidectomy with myringotomy alone in terms of hearing improvement in short-term follow-up in the surgical treatment of OME in 6-12-yearold children.
References
- Emmett SD, Kokesh J, Kaylie D. Chronic ear disease. Med Clin. 2018;102(6):1063-79.
- Coleman A, Cervin A. Probiotics in the treatment of otitis media. The past, the present and the future. Int J Pediatr Otorhinolaryngol. 2019;116:135-40.
- Jalali MM, Rezaie S, Kousha A, et al. Detection of fungal DNA in the middle ear effusion of patients suffering from otitis media with effusion. Iranian J Pub Health. 2008;37(4):109-13.
- Aarhus L, Tambs K, Kvestad E, Engdahl B. Childhood otitis media: a cohort study with 30-year follow-up of hearing (the HUNT study). Ear Hear. 2015;36(3):302.
- Zernotti ME, Pawankar R, Ansotegui I, Badellino H, Croce JS, Hossny E, et al. Otitis media with effusion and atopy: Is there a causal relationship?. World Allergy Organ J. 2017;10:1-9.
- Núñez-Batalla F, Jáudenes-Casaubón C, Sequí-Canet JM, Vivanco-Allende A, Zubicaray-Ugarteche J. Diagnosis and treatment of otitis media with effusion: CODEPEH recommendations. Acta Otorrinolaringol Esp (Engl Ed). 2019;70(1):36-46.
- Daniel M, Imtiaz-Umer S, Fergie N, Birchall JP, Bayston R. Bacterial involvement in otitis media with effusion. Int J Pediatr Otorhinolaryngol. 2012;76(10):1416-22.
- Francis NA, Waldron CA, Cannings-John R, Thomas-Jones E, Winfield T, Shepherd V, et al. Oral steroids for hearing loss associated with otitis media with effusion in children aged 2-8 years: the OSTRICH RCT. Health Technol Assess. 2018;22(61):1.
- Rovers MM, Schilder AG, Zielhuis GA, Rosenfeld RM. Otitis media. Lancet. 2004;363(9407):465-73.
- Emaneini M, Khoramrooz SS, Taherikalani M, Jabalameli F, Aligholi M. Molecular characterization of Staphylococcus aureus isolated from children with adenoid hypertrophy: emergence of new spa types t7685 and t7692. Int J Pediatr Otorhinolaryngol. 2011;75(11):1446-9.
- Hoa M, Syamal M, Schaeffer MA, Sachdeva L, Berk R, Coticchia J. Biofilms and chronic otitis media: an initial exploration into the role of biofilms in the pathogenesis of chronic otitis media. Am J Otolaryngol. 2010;31(4):241-5.
- Saylam G, Tatar EÇ, Tatar I, Özdek A, Korkmaz H. Association of adenoid surface biofilm formation and chronic otitis media with effusion. Arch Otolaryngol Head Neck Surg. 2010;136(6):550-5.
- Emaneini M, Gharibpour F, Khoramrooz SS, Mirsalehian A, Jabalameli F, Darban-Sarokhalil D, et al. Genetic similarity between adenoid tissue and middle ear fluid isolates of Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis from Iranian children with otitis media with effusion. Int J Pediatr Otorhinolaryngol. 2013;77(11):1841-5.
- Gates GA, Avery CA, Prihoda TJ, Cooper Jr JC. Effectiveness of adenoidectomy and tympanostomy tubes in the treatment of chronic otitis media with effusion. N Engl J Med. 1987;317(23):1444-51.
- Gates GA, Avery CA, Prihoda TJ. Effect of adenoidectomy upon children with chronic otitis media with effusion. Laryngoscope. 1988;98(1):58-63.
- Stenstrom R, Pless IB, Bernard P. Hearing thresholds and tympanic membrane sequelae in children managed medically or surgically for otitis media with effusion. Arch Pediatr Adolesc Med. 2005;159(12):1151-6.
- Mandel EM, Rockette HE, Bluestone CD, Paradise JL, Nozza RJ. Myringotomy with and without tympanostomy tubes for chronic otitis media with effusion. Arch Otolaryngol Head Neck Surg. 1989;115(10):1217-24.
- Mandel EM, Rockette HE, Bluestone CD, Paradise JL, Nozza RJ. Efficacy of myringotomy with and without tympanostomy tubes for chronic otitis media with effusion. Pediatr Infect Dis J. 1992;11(4):270-7.
- Shekelle P, Takata G, Chan LS, Mangione-Smith R, Corley PM, Morphew T, et al. Diagnosis, natural history, and late effects of otitis media with effusion. Evid Rep Technol Assess. 2002;(55):1-5.
- Rosenfeld RM, Kay D. Natural history of untreated otitis media. Laryngoscope. 2003;113(10):1645-57.
- Hellström S, Groth A, Jörgensen F, Pettersson A, Ryding M, Uhlén I, et al. Ventilation tube treatment: a systematic review of the literature. Otolaryngol Head Neck Surg. 2011;145(3):383-95.
- Vlastos IM, Houlakis M, Kandiloros D, Manolopoulos L, Ferekidis E, Yiotakis I. Adenoidectomy plus tympanostomy tube insertion versus adenoidectomy plus myringotomy in children with obstructive sleep apnoea syndrome. J Laryngol Otol. 2011;125(3):274-8.
- Rasheed AM. Adenoidectomy with Myringotomy and Tympanostomy Tube Versus Adenoidectomy with Myringotomy in Treatment of Otitis Media with Effusion in 5-7 Years Old Children. Al-Kindy College Med J. 2016;12(1):83-6.
- Rovers MM, Straatman H, Ingels K, van der Wilt GJ, van den Broek P, Zielhuis GA. The effect of short-term ventilation tubes versus watchful waiting on hearing in young children with persistent otitis media with effusion: a randomized trial. Ear Hear. 2001;22(3):191-9.
- Xu WM, Ye YH. Effect of tympanostomy tube insertion with adenoidectomy for children with recurrent otitis media with effusion. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. J Clin Otorhinolaryngol Head Neck Surg. 2016;30(23):1873-5.
- Khodaverdi M, Jørgensen G, Lange T, Stangerup SE, Drozdziewizc D, Tos M, et al. Hearing 25 years after surgical treatment of otitis media with effusion in early childhood. Int J Pediatr Otorhinolaryngol. 2013;77(2):241-7.
- Rasheed AM. Adenoidectomy with Myringotomy and Tympanostomy Tube Versus Adenoidectomy with Myringotomy in Treatment of Otitis Media with Effusion in 5-7 Years Old Children. Al-Kindy College Med J. 2016;12(1):83-6.
- Browning GG, Rovers MM, Williamson I, Lous J, Burton MJ. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane database of systematic reviews. 2010(10).
- Lous J, Burton MJ, Felding JU, Ovesen T, Rovers MM, Williamson I. Grommets (ventilation tubes) for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst Rev. 2005;(1).
- Tao J, Luo R, Chen Y, Hou C, Qin H. Myringotomy or tympanostomy tube insertion, comparison of surgical treatment of adenoid hypertrophy and otitis media with effusion in children. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zh J Clin Otorhinolaryngol Head Neck Surg. 2020;34(3):207-10.
- Zhang Y, Fu Y. Different treatment methods and efficacy analysis of otitis media with effusion in children with different hearing loss. Lin Chuang er bi yan hou tou Jing wai ke za zhi= J Clin Otorhinolaryngol Head Neck Surg. 2022;36(10):731-5.