- Biomedical Research (2010) Volume 21, Issue 2
Acute subdural hematoma with severe traumatic brain edema evacuated by Dural-stabs -A new brain preserving technique
Abdul Rashid Bhat*, Mohammed Afzal Wani, Altaf R. Kirmani,
Department of Neurosurgery, Sher-i-kashmir Institute of Medical Sciences (SKIMS), Srinagar Kashmir, India.
- *Corresponding Author:
- Abdul Rashid Bhat
B-4 Faculty Quarters
Sher-I-Kashmir Institute of Medical Sciences
Srinagar, Kashmir
India 190011.
Tel: +919419081377
E-mail: seven_rashid@rediffmail.com
Accepted date: December 17 2009
Abstract
The Department of Neurosurgery Sher-i-Kashmir Institute of Medical Sciences (SKIMS) Srinagar, a single neurosurgical centre in Kashmir valley, assessed prospectively, under a uniform protocol, 120 patients of severe traumatic brain edema with acute subdural hema-toma by wide decompressive craniectomy with dural-stabs in 60(cases) patients as against conventional dural opening (open dural flap) and removal of acute subdural hematoma in 60(controls) patients during a period of 3 years from Jun. 2006 to Jun. 2009. A free bone flap was elevated and preserved. All patients had GCS (Glassgow Coma Scale) score of 8 and less. The elective ventilation and ICP monitoring was carried out in all patients. Most patients were young and males with a mean age of 30 years in both groups. The overall survival of the dural-stab group (case-study) was 78.3% with good recovery in 43.3% and a mortality of 21.6% (13/60) as compared to 40% survival in open dural flap (control) group with 11.6% good recovery and a mortality of 60% (36/60) . The conventional (open dural flap) procedure to remove the clot proved dangerous in a traumatic “vent-searching” and edematous brain, restricted in a rigid cranial vault. This midway-approach, known in SKIMS as “Dural-Stabs”, between the only decompressive craniectomy and removal of acute subdural clot by open dural flap (conventional) method, proved much effective in increasing survival of pa-tients with low GCS and severe traumatic brain edema with acute subdural hematoma. In conclusion decompressive craniectomy alone is not sufficient and open dural flap is full of risk in such patients. The new innovative and indigenous technique is much favourable to the patient outcome.
Keywords
Acute Subdural Hematoma, Severe Brain Edema, Dural-Stabs, New Technique, Outcome.
Introduction
The concept of wide decompressive craniectomy in svere traumatic brain swelling is based on the principle of Monro-Kellie Doctrine that ‘total intracranial volume is fixed because of rigid and inelastic nature of skull’ which contains brain [1, 2]. Kocher T in 1901and Harvey Cushing in 1905 were the first to describe decompressive craniectomy for the relief of increased intracranial pressure [3, 4]. The decompressive craniectomy is one of the treatment modalities which can be performed in the worsening and low GCS score patients with dilated pupils and resisting maximal decongestant therapy because of acute subdural hematoma, contusions and acute brain swelling [5]. The surgical decompression after severe traumatic brain injury by open dural flaps, removal of contused and infarcted brain, removal of acute subdural and extradural hematomas is an effective practice [6].However in all these procedures the aim is to gain intracranial extraspace by way of decompression to change the constant of “fixed intracranial volume in rigid and inelastic skull” to quickly relieve the raised ICP. The Department of Neurosurgery SKIMS Srinagar, Kashmir prospectively evaluated all the standard procedures against a new modified (dural-stabs) technique and found promising results. The main objective of this study was to evaluate the effect of “duralstabs” in the complete removal of acute subdural hematoma for quick relief of raised intracranial pressure(ICP) and in preventing any further secondary brain damage due to opening of dural flaps where superficial clots and contused brain could be removed with ease but the deeper edematous white matter swelling, which pushes itself and the overlying cortex with vital vasculature out of the cranial cavity causes lacerations to further compound the brain insult.
Material and Methods
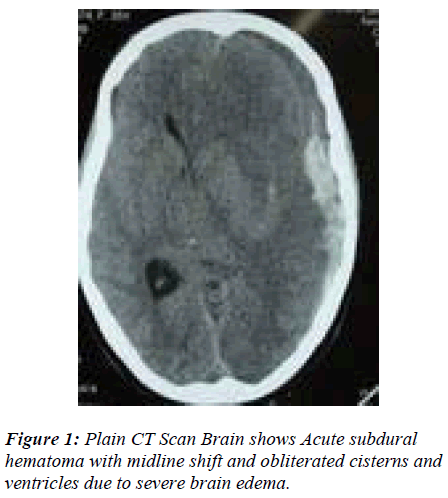
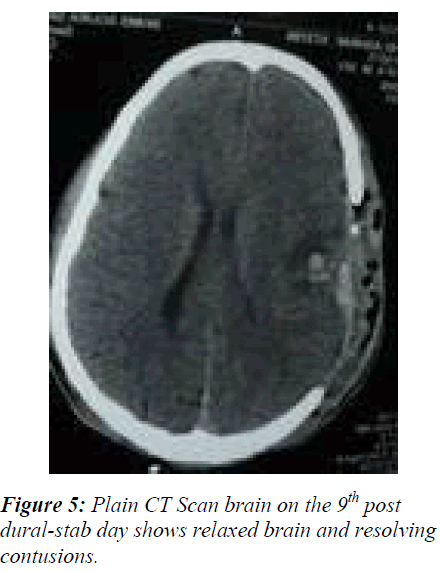
The study to evaluate the efficacy of the ‘dural-stabs’ after wide craniectomy in 60 cases against the conventional open dural flap after wide craniectomy in 60 controls to decompress acute subdural hematomas in low GCS (Glassgow Coma Scale) [7] score 3 - 8 in presence of severe brain edema, took place in the Department of Neurosurgery, SKIMS Kashmir from Jun. 2006 to Jun. 2009. All 120 patients of GCS score 3 – 8 following trauma were received in the accident and emergency room within 30 minutes to 6 hours of trauma. Immediate intubation and resuscitation followed non-contrast CT-scan brain with bone windows. Patients with significant acute subdural hematoma (> 25 ml volume) causing midline shift (> 5mm) and severe brain edema (Fig. 1) due to underlying multiple hemorrhagic and non-hemorrhagic contusions, subarachnoid hemorrhages and diffuse axonal injury were randomly allotted to the duralstabs (cases) and open dural flap (controls) decompressive procedures. Postoperatively all patients were electively ventilated, subjected to ICP monitoring, serial arterial blood gas (ABG) analysis and serial CT-scans to evaluate intracranial extraspace gain (Fig. 5) and whenever indicated such as the worsening of GCS score. The outcome was assessed by applying Glassgow Outcome Scale [8] at the time of discharge and upto 6 months after discharge, however results drawn here are of the time of discharge. Initially bone flaps were implanted in the abdominal fat, now these are stored at -80° C for next 3 months for reimplantation. The data was analysed and evaluated by the statistical methods like student’s T-test. The analysis of Variance was used where-ever applicable.
Technique of Dural-Stabs
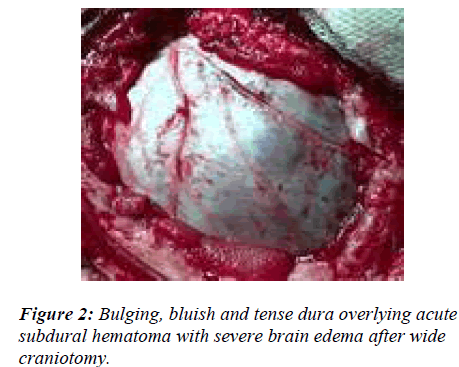
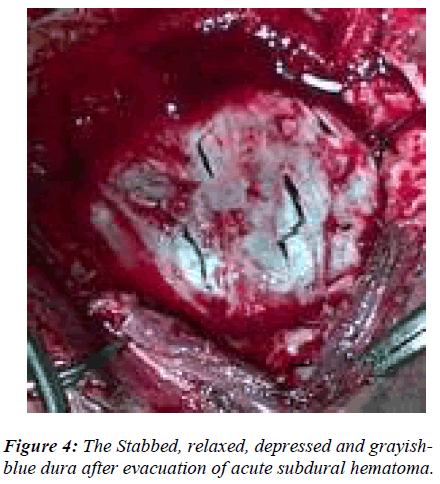
This is a decompressive procedure for acute subdural hematoma in the presence of severe brain edema and midline shift (Fig. 1) to preserve the anatomical integration of the arachnoid, pia, brain tissue and its vasculature by opening dura less than or equal to a gyral size at one place. The blue, intact and tense dura is completely defined after wide craniectomy (Fig. 2). A no.11 stab knife is used to apply multiple linear dural incisions of about 5 – 8 mms long, in horizontal lines, parallel to vessels and 2 – 2.5 cms apart from each other. The knife tip should not penetrate the dura more than 0.5 to 1.0 mm (Fig. 3). The initial gush of the hematoma is forceful and venous-like but subsequent incisions reduce the gush force. The normal saline is used to wash the dura off the blood and clots continuously. A soft 6F silastic cather is passed through the stab horizontal to, and its eye facing, the dura, to wash and remove any stuck up clots on the surface of brain. The completion of the procedure is indicated by the change in the colour, consistency and the flattening of dura (Fig. 4). Although most of the times the dura continues to be tense even after the drainage of the subdural hematoma, only small blebs of arachnoid covered brain tissue incarcerate and slightly widen the stab openings without any brain lacerations. Since most of the liquefied blood and the clot accumulate in the centre of the craniectomy site causing central dural bulge, the periphery of the craniectomy is preferred as the site for the first few incisions. This is to avoid incisional injury to the peripheral brain, close to the overlying dura, in case the hematoma is drained in the thickest and usually central part of craniec-tomy. However if the dura is torn with tensly pouting brain, the procedure is still ideal but in large tears if the brain is lax and inside the lines of the cranial vault, the open dural flap is carried out. Also in the wake of any bleeding from brain, which usually stops with continuous saline washes, it is mandatory to locate the site of bleed and apply a longer incision rather than a stab to achieve complete hemostasis. The dura can always be cauterized locally for any bleeding. Thus acute subdural hematoma is removed through dural-stabs while at the same time the integrity of the dura, arachnoid, pia, brain and its vasculature, in the presence of the severe ‘vent-searching’ brain edema, is largely preserved. Thus exta-space is gained intracranially by craniectomy and dural relaxation in addition to removal of acute subdural hemorrhage, changing the fixed coefficient of “total intracranial volume” (Fig. 5). Though solid clot may stick to the brain at the end of the procedure but the liquid and semi-solid blood evacuation leads to the quick relief of the raised intracranial pressure (ICP), much needed to save the patient. Also the stabbed dura has much more tensile strength and stretch capability, in case of any postoperative brain edema and rise in ICP, to provide extra space and negate the pressure effect.
Results
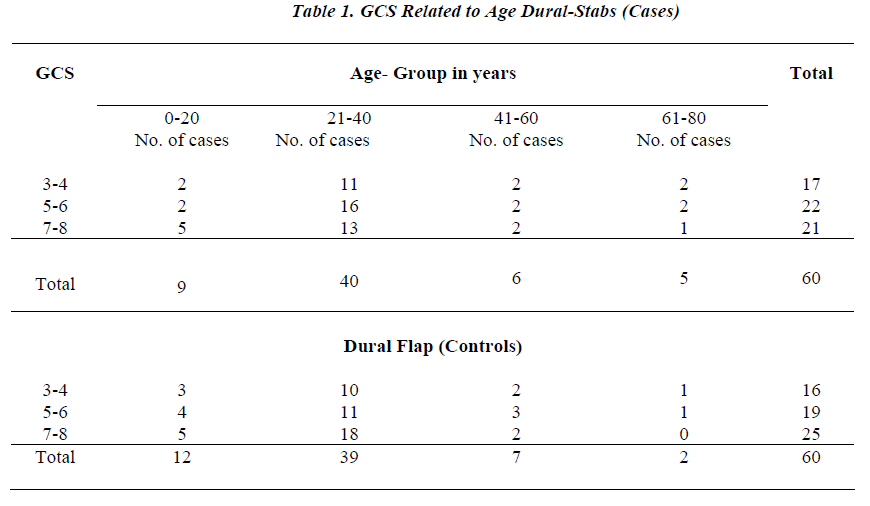
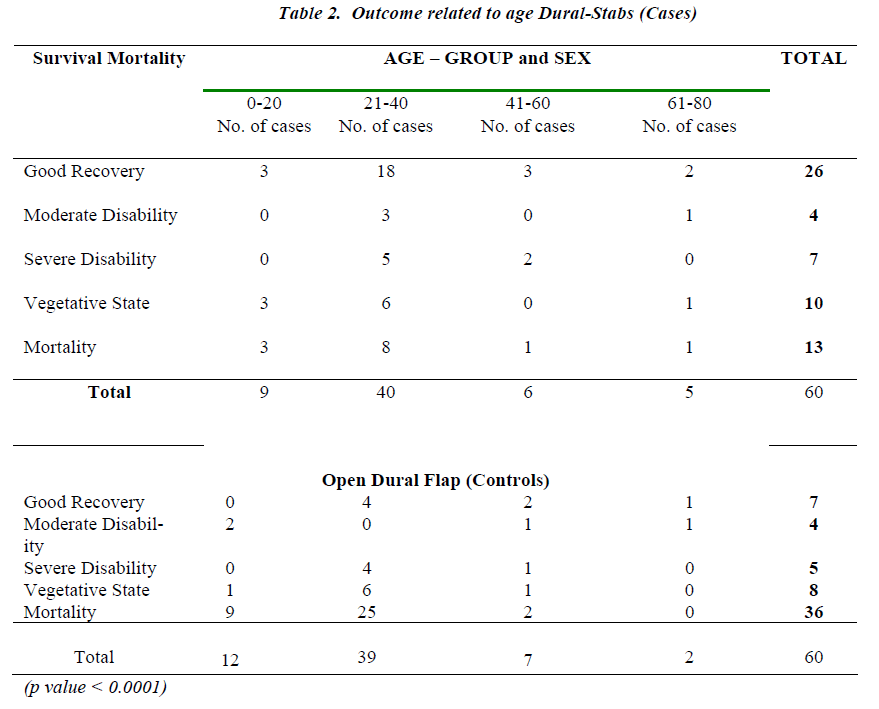
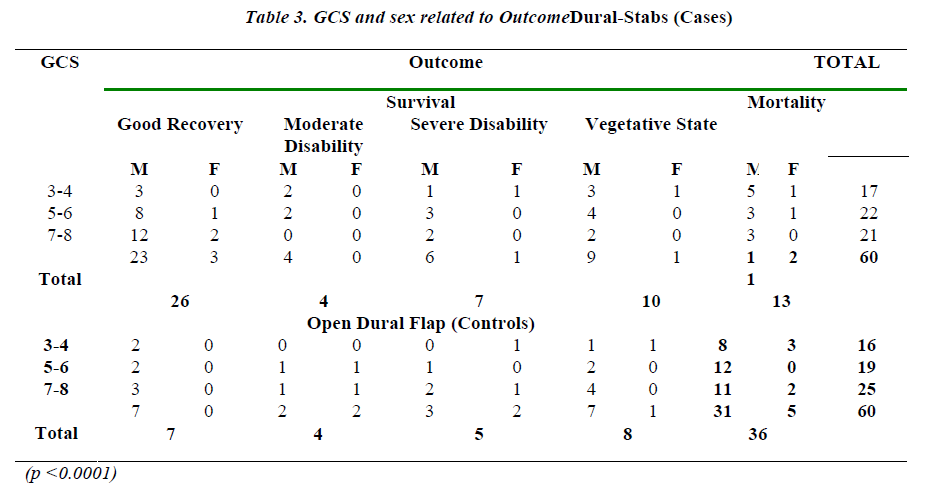
The comparative results of the cases (dural-stabs) and the controls (open dural flap) revealed similar demographic variables in both the groups. But the GCS and the outcome of case study and control groups varied. A total of 14 patients were operated on the posterior fossa, 6 from dural-stabs and 8 from control group. Bilateral decompressive craniectomy was performed in a total of 12 patients, 7 from dural-stabs and 5 from open dural flap group. Most patients reached the emergency room within 4-6 hours of the injury. Both the groups had more than 80% males (Table 1). Most patients (> 65%) were in the age group of 21 – 40 years both from case as well as control groups. Of the dural-stabs group 28.3% (17/60) patients were in the GCS 3-4 group while only 26.6% of the open dural flap group had GCS 3-4. In comparison to only 35% (21/60) patients of GCS 7-8 in the dural-stab group, most of the open dural flap patients, 41.7% (25/60), were in the in GCS 7-8 group. Noteworthy was maximum number of patients, 30% (18/60), of open dural flap (controls) being in the age group of 21-40 yrs with GCS 7-8. However only 21.6% (13/60) patients of dural-stabs had such an age group and GCS . Conversely most, 26.6% (16/60) of the dural-stab group with age 21-40 had GCS of only 5-6 (Table 1). While comparing outcome to the age and sex, the dural-stab (case study group) had an overall and better survival of 78.3% (47/60) and a good-recovery of 43.3% (26/60) especially 30% (18/60) good recovery in the age group 21-40 yrs. This proved effective as compared to an overall 40% (24/60) survival and 11.6% (7/60) good recovery in the open dural flap (contrtrol group) while age group of 21-40 yrs also showed a Mere 6.6% (4/60) good recovery. Mortality of 28% (2/7) in females and 20% (11/53) in males of dural-stab group was also lower as compared to the 50% (5/10) deaths in females and 62% (31/50) deaths of males in the open dural flap group. The children and age group 0-20 yrs alone had only 33.3% (3/9) mortality in the dural-stabs as compared to the open dural flap group with 75% (9/12) deaths (Table 2). The GCS and outcome relationship shows that dural-stab group has better survival of 78.3% (47/60) than open dural flap (control group) with 40% (24/60). The dural-stab group depicted higher survival for all GCS groups, GCS 3-4: 18.3% (11/60), 5-6: 30% (18/60), 7-8: 30% (18/60) and an overall good recovery of 43.3% (26/60), most for GCS 7-8: 23.3% (14/60). Comparatively open dural flap group revealed lower survival in all GCS groups, GCS 3-4: 8.3% (5/60), 5-6: 11.6% (7/60), 7-8: 20% (12/60) and an overall good recovery of 11.6% (7/60) with 5% (3/60) in GCS 7-8 group (Table 3). A lower mortality of 21.6% (13/60) with 10% (6/60) in GCS 3-4 among dural-stabs (cases) than patients of open dural flaps (controls) was evident (Table 3). The open dural flap group showed a mortality of 60% (36/60) and it was highiest 21.6% (13/60) in the GCS 7-8 and 18.3% (11/60) in GCS 3-4. At the time of discharge the dural-stabs had favourable outcome (good recovery and moderate disability) in 50% (30/60) and poor outcome in 50% (30/60) patients, while in open dural flap, 18.3% (11/60) had fa-vourable outcome and 81.6% (49/60) poor outcome. This improved over 6 months. There were many cases whose condition, due to the associated injuries, did not allow major brain surgery, the dural-stabs made itself an alternative procedure for such patients. The complications like wound infection, seizures, hygromas, hydrocephalus and cerebral atrophy (in most of the surviving patients in both groups) were not related to the surgical decompression but pimary trauma. These were managed without causing any deaths.
Discussion
Traumatic acute subdural hematoma is one of the most lethal of all head injuries in which primary brain injury is more critical factor than a clot. The outcome depends upon the ability to control ICP rather than removal of subdural clot. Although timing of clot removal within 4 hours of injury has lowered mortality to 30% with functional rate of 65% but ICP control has been a critical factor [9] .The high mortality of acute subdural hematoma is largely explained by its frequent association with primary brain damage consisting of contusions and brain swelling. However the nature and causes of brain swelling after traumatic brain injury are multifactorial and poorly understood. Brain swelling associated with acute subdural he-matoma is caused by secondary insult in addition to parenchymal injury. The authors report outcome of acute subdural hematoma associated with brain swelling as poor even when treated with early surgical evacuation. The mortality rate of such patients was over 75% [10]. At Neurosurgical centre, SKIMS Kashmir, the outcome of such patients with early and open dural flap was similar I.e, poor with 60% mortality. But dural-stabs had favourable outcome of 50% and survival rate of 78.3% with only 21.6% mortality. Brain swelling and the acute subdural hematoma were the most common, i.e 64%, CT-scan findings in a series [11]. Even after operative decompression, the prognosis of acute subdural hematoma is still poor in many cases. This is thought due to coexisting brain damage (Diffuse Axonal Injury, contusions, lacerations) that leads to poor outcome. Thus poor outcome is resultant of the compression of the microcirculation and resulting low CBF which leads to lucid interval i.e, ‘talk and die’ [12]. It was observed at SKIMS, Kashmir that conventional (open dural flap) surgery in controls to remove subdural clot in presence of coexisting injuries and edema , even though early, could not avoid pouting and laceratin of brain and vessels despite substantial amount of decongestion. This lead to poor outcome in 81.6% of the patients in controls (open dural flap). However dural-stabs group had all favourable outcome. Experimental investigators assessed the effect of rapid or delayed surgical evacuation on the physiological consequence and brain edema formation in a rat model of acute subdural hematoma (SDH) coupled with either diffuse brain injury (DBI) or hypoxemia. The SDH was made by an autologous blood injection, while DBI was induced using the impact acceleration model (mild, 450 g/1 m; severe, 450 g/2 m). Physiological parameters measured included intracranial pressure (ICP), mean arterial blood pressure (MABP), cerebral blood flow (CBF), and brain tissue water content. The surgical evacuation showed no beneficial effects on the brain edema formation assessed at 5 h post-injury. The rapid, but not delayed, evacuation significantly reduced both the increased ICP level and brain water content. The additional insult of hypoxemia resulted in a progressive ICP elevation, persistently depressed CBF, and severe brain swelling. Under this situation, the rapid evacuation exacerbated brain edema. These results have clinical implications for the management of severe traumatic SDH, especially its operative indication and timing [13]. The results revealed in the Department of Neurosurgery, SKIMS showed that stabing the dura at intervals decompressed the underlying edematous brain slowly with better results, in comparison to the open dural flap (Table 3). Some authors showed Single burr hole evacuation in the emergency room as a useful treatment for acute subdural hematoma of the posterior cranial fossa because the procedure can be performed easily and rapidly, thus achieving reduction of intracranial pressure [14]. At SKIMS all 6 cases of posterior fossa acute subdural hematoma had multiple dural incisions after wide craniectmy (dural-stabs), avoiding wastage of time in opening dural flaps after craniectomy. A series reports the outcome of acute subdural hematoma, delay from injury to operation was the factor of greatest therapeutic importance. Patients who underwent surgery within the first four hours had a 30 per cent mortality rate, as compared with 90 percent in those who had surgery after four hours (P less than 0.0001) [15]. However at SKIMS most patients were received after 4 hours but mortality rate, though time factor counts, differed with the procedure and was least for dural-stabs (21.6%). Hemispherical brain edema, observed after evacuation of subdural or extradural hematoma, is a well recognized entity. In an autopsy study 17 out of 151 cases had this and it was not contributed to contusions, intracerebral hematoma or infection. The aetiopathogenesis of the lesion is still debated [16]. However there is evidence to suggest that it may be secondary to ischemia caused by the compressive hematoma or vasomotor paralysis [17]. All 120 patients at SKIMS, Kashmir had brain edema, contusions and acute subdural clot. It is reported that at the time of discharge of 49 patients, 72% had poor outcome (severe disability, vegetative state or death) with 59% mortality and 28% had favourable outcome (good recovery, moderate disability). This improved 6 months after trauma, from 72% to 59% (poor outcome) and 28% to 41% (favourable out-come) [5]. In Neurosurgery SKIMS, among the two groups, dural-stab group had 43.3% good recovery as compared to the open dural flap (control) group with only 11.6% . An author reported 33% mortality and 14% vegetative state with only 7% demonstrating good outcome [18]. While at SKIMS Kashmir, open dural flap (cotrols) had 60% mortality and only 18.3% good recovery as against dual-stab group with better outcome (Table 3).
Conclusion
The dural-stabs is the quicker, safer (in any condition), novel decompressive and effective procedure for the removal of acute subdural hematoma and gaining extra-space intracranialy, in the presence of severe tramatic brain edema with good outcome. The residual solid clot dissolves slowly over a period of few days without any further rise in ICP. The techique avoids brain pouting and lacerations at the time of surgery. However this procedure needs further trials in the future to understand its effect on the pathogenesis of brain edema after gaining extra-space intracranially without opening dural flap and to establish it as a routine decompressive technique.
Acknowledgement
Thanks to Rohul, Adam, Saim and Huwa for continuous support and Turab & Hilal for assistance.
References
- Kellie G. On death from cold, and, on congestion of the brain: An account of the appearances observed in the dissection of two of three individuals presumed to have perished in the storm of 3rd November 1821; with some reflections on the pathology of the brain. Trans Med Chir Soc Edinb 1824; 84-169.
- Monro A. Observations on the structure and the function of the nervous system. Edinburgh , Creech and Johnson, 1823, p 5.
- Kocher T. Die Therapie des Hirndruckes, in Holder A (ed): Hirnerschutterung, Hirndruck und chirurgische Eingriffe bei Hirnkrankheiten. Vienna: A Holder, 1901, pp 262-266.
- Cushing H. the establishment of cerebral hernia as a decompressive measure for inaccessible brain tumors with the description of intermuscular methods f making the bone defect in the temporal and occipital regions. Surg Gynecol Obstet 1905; 1: 297-314.
- Munch E, Horn P, Schurer L, Piepgras A, Paul T, Schmiedek P. Management of severe traumatic brain injury by decompressive craniectomy. Neurosurgery 2000; 47: 315-323.
- Chambers I, Treadwell L, Mendelow AD. Secondary brain insults following traumatic brain injury (TBI) in children and their relationship with outcome. British Journal of Neurosurgery 2000; 14(5): 416-423.
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness, a practical scale. Lancet 1974; 2: 81-4.
- Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet 1975; 1: 480-484.
- Wilberger JE, Harris M, Diamond DL. Acute subdural hematoma: morbidity, mortaliy and operative timing. J Neurosurgery 1991; 74 (2): 212-218.
- Sawauchi S, Abe T. The effect of haematoma, brain injury and secondary insult on brain swelling in traumatic acute subdural haemorrhage. Acta Neurochirurgica 2008;150(6):531-536.
- Faleiro RM, Faleiro LC, Caetano E, Gomide I, Pita C, Coelho G, Bras E, Carvalho B, Gusmao SN. Decompressive Craniotomy: prognostic factors and complications in 89 patients. Arq Neuropsquiatr 2008; 66(2b): 369-373.
- Schroder ML, Muizelaar JP, Kuta AJ. Documented reversal of global ischemia immediately after removal of an acute subdural hematoma : Report of two cases. J Neurosurg 1994; 80: 324-327.
- Sawauchi S, Marmarou A, Beaumont A, Signorett S, Fukui S. Acute subdural hematoma associated with diffuse brain injury and hypoxemia in the Rat : effect of surgical evacuation of the hematoma. Journal of Neurorauma 2004; 21 (5):563-573.
- Motohashi O, Kameyama M, Shimosegawa Y, Fujimori K, Sugas K, Onuma T. Single burr hole evacuation for traumatic acute subdural hematoma of the posterior fossa in the emergency room. Journal of Neurotrauma 2002;19(8):993-998.
- Seelig JM, Becker DP, Miller JD, Greenberg RP, Ward JD, Choi SC. Traumatic acute subdural hematoma : major mortality reduction in comatose patients treated within four hours. New England Journal of Medicine1981;304 (25):1511-1518.
- Adams JH, Graham DI, Gennareli TA. Neuropathology of acceleration- induced head injury in the subhuman primate. In : Head Injury : Basic and Clinical Aspects, (Eds.) Grossman RG, Gildenberg PL, Raven Press, 1982, P. 141.
- Yoshino E, Yamaki T, Higuchi T, Horikawa Y, Hirakawa K. Acute brain edema in fatal head injury : analysis by dynamic CT scanning. J Neurosurg 1985; 63:830-839.
- Marshall LF, Gautille T, Klauber MR. The outcome of severe closed head injury. J Neurosurg 1991; 75:28-36.