Review Article - Otolaryngology Online Journal (2018) Volume 8, Issue 4
Acute Exteriorized Ethmoiditis of the Child: About 23 Cases Diagnosis and Management
- *Corresponding Author:
- Koumalou Emmanuel Bakyono, MD
Ear Nose and Throat Unit at Yalgado ouedraraogo Teaching Hospital
Burkina Faso, 03 BP 7022 Ouaga 03
Tel: +226 7027 18 39
E-mail: leben_manu@yahoo.fr
Received date: August 24, 2018; Accepted date: November 19, 2018; Published date: November 26, 2018
Abstract
Objective: To describe the diagnostic and therapeutic characteristics of acute exteriorized ethmoiditis of the child.
Patients and Methods: This was a retrospective study conducted from January 2006 to December 2015 in the ENT service of the Yalgado Ouedraogo, teaching hospital. All the files of children of under 15 year hospitalized for acute exteriorized ethmoiditis were included.
Result: The study concerned 23 patients, including 17 boys and 06 girls. The average age was 11 years. All the children presented immediate antecedents of nasopharyngitis. The average time for consultation was 14 days. The painful orbital tumefaction was the main reason for consultation. The clinical examination allowed to find an infectious syndrome in 15 cases, associated at a rhinologic syndrome that was isolated in 10 cases. Computing related many sinutis on 17 cases and 2 cases of frontal sino-dural empyema. The exteriorized ethmoiditis was bilateral in 8 cases. According to Chandler's classification, this was mainly stage II in 10 cases, and III in 6 cases. The streptococci were isolated in the most cases. The treatment was only medical in 14 cases. In 9 cases this was an ethmoidectomy associated with the surgical drainage of the collected orbital cellulitis. The antibiotic treatment was in the most cases constituted at the association of ceftriaxone and metronidazole, parenterally over an average duration of 08 days. The evolution was favorable in 20 patients. The sequelae occurred in 03 patients at type of definitive blindness, a decrease of the visual acuity. No deaths were recorded.
Conclusion: The exteriorised acute ethmoiditis is a relatively common complication of rhinopharyngitis in children. It's a real emergency diagnostic and therapeutic. The prevention remains the correct management of acute rhinopharyngitis.
Keywords:
Acute ethmoiditis; Child; Diagnosis; Treatment
Introduction
The Acute ethmoiditis, child acute sinusitis, is relatively common. It is often a complication of the acute nasopharyngitis. A diagnostic problem in the form of early, not exteriorized. It is a medical emergency that has long been a provider of functional and vital complications [1,3]. It is a serious pathology because of the risks of extension of the infection at the oculo-orbital and endocranial level. These complications are daunting. Their gravity lies in the risk of blindness by optic nerve damage, and neurological sequelae. However, the diagnosis of these ethmoidities is always at the stage of complications in our context. The peculiarities of these ethmoidities in our regions have been little discussed in the literature.
The purpose of this work was to describe the diagnostic and therapeutic features of the acute ethmoiditis exteriorized in our context.
Materials and Method
It is a retrospective study conducted on 10 consecutive years, from January 2006 to December 2015 in the ORL department of the University Hospital Center Yalgado Ouedraogo of Ouagadougou. All records of children aged less than 15 years hospitalized for an acute ethmoiditis exteriorized were included. We excluded patients who did not have a CT scan of the facial sinus and patients whose records were incomplete. The other causes of palpebral edema have been excluded. We have identified for each patient at admission age, sex, the entry door, previous treatments in hospitalization, the period of consultation, clinical and paraclinical, signs the results of biological samples and bacteriological, the duration of hospitalization, treatment, and evolution.
Results
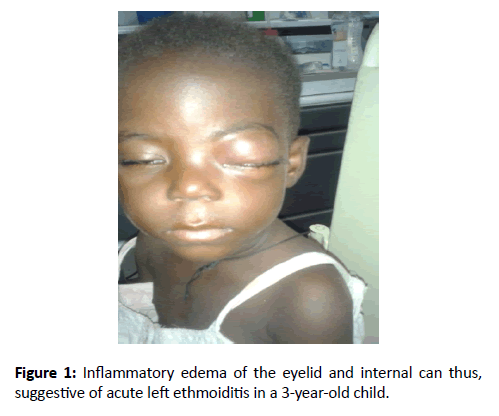
Our study population contains 23 patients, 17 boys and girls 6. The average age was 11 years with extremes ranging from 11 months and 15 years. All children had an immediate history of nasopharyngitis. In 9 cases, patients had prior consultation with a physician generalist and in 7 cases an ophthalmologist. The average consultation time was 14 days (extreme 4 to 30 days). Orbital tumefaction painful was the obvious sign in all patients (Figure 1).
At the time of admission, fifteen (15) patients had an infectious syndrome with a temperature greater than or equal to 38 degrees. They had never received antibiotics as an outpatient. Eight (8) were apyretiques with antibiotic treatment associated with an inflammatory anti either an antipyretic. At physical examination, the ethmoiditis was enacted right in 10 cases left in 5 cases and was bilateral in 8 cases. All the children had ophthalmologic signs (100%), (Table 1).
| Clinical signs | Number | Percentage (%) |
|---|---|---|
| Eyelid edema | 23 | 100 |
| Purulent rhinorrhea | 23 | 100 |
| Chemosis | 19 | 82 |
| Syndrome infectious | 15 | 65.2 |
| Exophtalmy | 18 | 78.3 |
| Complications | 3 | 13 |
Table 1: Distribution of patients based on clinical signs.
At the biological level, C-reactive protein was high and ranged from 20 and 180 mg/L and the sedimentation rate was accelerated in all patients. The average rate of white blood cells was 15400 elements/mm3 with extremes of 12000 and 17000, predominance of polymorphonuclear neutrophils. The bacteriological samples were taken in 9 children. Six (6) results were positive. Isolated germs were distributed as follows: Streptococcus pneumonias 3 cases, Staphylococcus aureus 2 cases, Haemophilus influenzae 1 case. These children had not received antibiotics beforehand. The blood culture performed in 3 patients has been negative. The standard X-rays of the sinuses of the face made in five (05) patients found an ethmoidal homogeneous diffuse opacity.
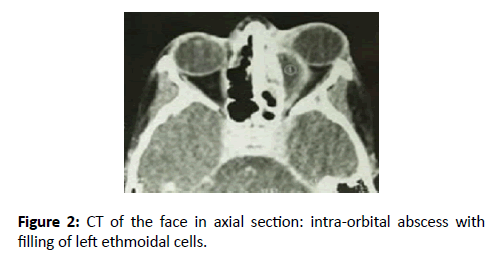
The craniofacial CT (CT) and parenchymal in axial and Coronal section was done in 23 children. Different pictures have been found: images of pansinusite (n=6), isolated ethmoidal opacity (n=5), unilateral ethmoido-maxillary opacity (n=5), opacity ethmoido-fronto-maxilla unilateral (n=3), bilateral ethmoido-frontal opacity (n=2). Opacity ethmoidosphenoido- maxillary bilateral (n=2). He associated oculo-orbital and endocranial complications. The endocranial complications were a frontal subdural empyema (2 cases). The evolutionary characteristics of the patients with oculo-orbital complications of the ethmoiditis are shown in Table 2 according to the classification of Chandler [2].
| Evolutionary characteristics | Number of cases | |
|---|---|---|
| Stade I | Périorbital cellulite | 4 |
| Stade II | Orbital cellulite | 10 |
| Stade III | Orbital abscess sub-periosteum | 6 |
| Stade IV | Intra orbital abscess | 2 |
| Stade V | The cavernous sinus thrombophlebitis | 1 |
Table 2: Evolutionary characteristics of the ethmoiditis according to the classification of Chandler.
All of our patients have received medical treatment based on a probabilistic and parenteral antibiotics in the first poly. The surgical treatment has been associated in 9 cases. The initial antibiotic treatment included the ceftriaxone + metronidazole + gentamycin (8 cases), ceftriaxone + metronidazole (7 cases), amoxicillin + clavulanic acid + metronidazole (6 cases), amoxicillin + clavulanic (1 case), ceftriaxone (1 case). The average length of this antibiotic was 08 days. The surgical treatment consisted of an incision drainage of the orbital suppuration by orbitotomie 9 cases. An ethmoidectomie by external way in 3 cases, drainage of subdural empyema in 2 cases. The length of hospital stay was an average of 10 days. The acute ethmoiditis did it again in 2 children, which led to a readmission to a new parenteral antibiotic treatment. The evolution was favorable in 20 patients. The consequences have been noted in 3 cases: 1 case of unilateral blindness right, 2 cases of down years of visual acuity. No deaths were reported (Figure 2).
Discussion
The acutes ethmoidities are relatively frequent in our context. They occur especially in male children. Our findings corroborate those of literature [1-3], but the fragmentized forms have become exceptional in the west since the advent of antibiotics [1,4].
The ethmoidal cells are first existing sinus cavities and developed in the first few months of life, which explains the frequency of their achievement in children. The ethmoiditis occurs most often during or after of acute rhinopharyngitis in children [3,5,6] with classically two peaks of frequency, 1 to 5 years and 10 to 15 years. Indeed, all the children had a history of rhinopharyngitis in our series.
The acute ethmoiditis realize an emergency ENT. We agree with Chandler imposed a diagnosis and early treatment because of the risk of oculo-orbital complications and endocranial that can jeopardize the functional and vital prognosis [7]. The extension of the infection to the orbit is done either by direct contact through the vascular pertuis of the unguis or congenital dehiscences of the extremely thin papery blade in the child, or through the periorbital venous network which allows the passage of septic embolus.
The diagnosis of an acute ethmoiditis externalized is easy, strongly suspected at clinical examination, confirmed by medical imaging.
The consultation period was 14 days. This long period of consultation can be explained by the fact that the first pass is done at the pediatrician or ophthalmologist. Indeed, palpebral edema predominant on the upper eyelid and the inner canthus was the first sign of appeal. It is almost constant and inflammatory. A feverish palpebral edema associated with rhinopharyngeal syndrome is strongly suggestive of the diagnosis. Fever was inconsistent in our series, we agree with some authors [1,7,8]. The reason is often the antipyretic and antibiotic treatment previously administered [9]. The palpebral edema was constant in our series as in Miloundja [1].
The association with palpebral ptosis is usual. The ophthalmoplegia is a sign of severity found in 12 of our patients. The same observation has been made by some authors [5,9]. It can be underestimated because often masked by eyelid edema.
The ORL examination must systematically search a purulent rhinorrhea. It has been present in our series in 78% of our patients.
Paraclinical plan, the standard X-ray still practiced in our regions, shows a nonspecific of the ethmoid unilateral opacity. The orbital ultrasound, simple, harmless and inexpensive would be a great contribution in our practice [10].
The ethmoido-orbital and brain CT is essential. We emphasize strongly with some authors the reliability of this review [11,12]. It allows a diagnosis of certainty and a complete injury report by the study of the whole of the sinus cavities, intra-orbital elements and intracranial structures.
Among the many classifications describing the orbito-palpebral involvement occurring during an acute ethmoiditis exteriorised, that of Chandler [3], defining 5 groups of increasing gravity seems to us right. All stages of severity have been found (Table 2). The stages II and III were the most represented because of the delay in consultation with patients, at the stage of the infection spreading to the intraorbital and endocranial spaces. This delay is linked to several causes including the therapeutic itinerary and low health coverage of regions. This same observation was made by other authors [1,6].
The results scannographiques showed a predominance of pansinusites witnessing once again the importance of the diagnostic delay and supported in the spreading of the infection to the other sinuses, orbit and even the brain.
To biological inflammatory syndrome noted in all cases. The bacteriological investigation was often disappointing during the fragmentized acute ethmoidites. Payments only, easy to make, endonasal and nasopharyngeal, have no value because the correlation with germs endo-sinus is not sigificative. However the levy at the level of the specific supposed Middle meatus is in practice impossible to realize in the child in the Chair, because of the narrowness of nasal. The most interesting collection is that of the abscess sub - periostes or orbital [4,5]. The seeds in question are variable according to the series. The most frequently found in the samples in our series by puncture of abscess under periosteum germs were: Streptococcus pneumoniae, Staphylococcus aureus and Haemophilus influenzae. The same finding was made by some authors [4,13]. In our series, we have isolated no anaerobic. However Brook [13], in his series which counted 26 patients, found 22% of anaerobic. This could be explained in our context, presumably by the unsuitability of sample collection and delivery conditions to the laboratory for this type of research.
The treatment of these infections is surgical. Medical treatment is based on initially probabilistic antibiotic therapy introduced from the admission of the patient and secondarily adapted to the results of the antibiogram [14-16]. The choice of probabilistic antibiotherapy varies from one author to another. Thus, it is not rare in the literature to find a multitude of proposals based on the practice of each authors [8,17-19]. For us, an essential condition to be met by probabilistic antibiotherapy: It must have effective antibiotics at the time on the aerobic and the anaerobic although in our context the highlight of these is not always obvious. We fully agree with the recommendations on rhinosinusitis of the child held in Brussels in September 1996 seeking to prescribe in first intention amoxicillin + clavulanic acid association or cefuroxime axetil [16].
The surgical treatment was indicated in the abscess subperiosteal or orbital. It consisted of a drainage achieved by only external orbitotomie, with incision of the periosteum, or associated with an ethmoidectomie endonasal or through external [15,20,21].
The evolution was favorable in 21 cases. Two patients presented a recurrence. The average drop was 11 months. The evolution despite treatment in our series was marked by the occurrence of formed consequences of unilateral blindness right (1) and lower Visual acuity (2 cases). These after-effects are essentially the corollary of the late consultation of our patients at very advanced stages. The prognosis of the ethmoidites depends on the precocity of diagnosis, the stage evolution percentage-clinic and support. According to Ben Amor [22], the advent of antibiotics decreased considerably the frequency of complications oculo-orbital and their evolutionary risk of blindness including the percentage of occurrence has increased from 10.5% in 1991 to 0.6 percent in 2009. Force, however, is to recognize that in our context this risk is still high because of the diagnostic delay [23].
Conclusion
The exteriorised acute ethmoidite is a relatively common complication of rhinopharyngitis in children. It's a real emergency diagnostic and therapeutic. Its gravity is related to the exterioration orbito-eyepiece and endocranial of infection. The treatment is essentially medical based appropriate antibiotic therapy. The formerly systematic drainage place is currently a topic of discussion. Its prevention based on a proper treatment of the rhinopharyngitis remains the challenge.
References
- Miloundja J, Ategdo S, Mandji Lawson JM, et al. The acute external ethmoidities of the child. About 9 cases. Med Afr Black. 2011;58:149-55.
- Chander JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414-28.
- Oxford LE, Mc Clay J. Complications of acute sinusitis in children. Otolaryngol Head Neck Surg. 2005;133:32-7.
- Francois M. Acute ethmoiditis externalised in children. EMC (Elsevier, Masson, SAS Paris) Otorhinolaryngology. 2008;20-440-A-10.
- Hytonen M, Atula T, Pitkaranta A. Complications of acute sinusitis in children. Acta Otolaryngol Suppl. 2000;543:154-7.
- Ikeda K, Oshima T, Suzuki H, et al. Surgical treatment of subperiostal abscess of the orbit: Sendai’s ten-year experience. Auris Nasus Larynx. 2003;30:259-62.
- BoughamouraL, Hmila F, Ben AliM, et al. Acute externalized ethmoiditis of children, study of 11 observations. J Tun ORL. 2006;16:22-5.
- Ernest S, Bosc JM, Piquout X, et al. Acute ethmoiditis. Retrospective study of 20 years. Bull Soc Ophthalmol. 1991;2:185-6.
- Chobaut JC, Menget A, Badet JM et al. The child's ethmoidities about 20 recent observations. JF ORL. 1993;42:195-200.
- Pinzuit- Ronde V, Elmaleh, Francois M, et al. Interest of the orbital ultrasound in the ethmoidities of the child. J Radiol. 1999;80:569-74.
- Fauchier F, Lescanne E, Sibel JP, et al. Acute infectious swelling of the orbital region in children. Indication of the CT according to the clinic (results of a multicentric study). Rev off soc fr ENT. 1999;52:19-25.
- Hammami B, Masmoudi M, Charfeddine I, et al. Management of orbital and endocranial complications of acute bacterial sinusitis. ENT Department CHU Habib Bourguiba. J Tun ORL. 2014;31:6.
- Brook I. Bacteriology of acute and chronic ethmoid sinusitis. J Clin Microbiol 2005;43:3479-80.
- Barry B. Recent data in ENT infectious disease on the first-line treatment of common ENT infections. Otorhinolaryngol letter and cervicofacial chiropractor. 2000;258.
- Chahed H, Bachraoui R, Kedous S et al. Management of oculo-orbital complications of acute sinusitis, Rabta Hospital, Tunisia. Rev d’ORL et chir Maxillo-fac. 2014;1007:87-9.
- Khaled H, El korbi A, Belhadjrhouma S, et al. Orbital complications of sinusitis: diagnosis and treatment. ENT Department, Fatouma Bourguiba Teaching Hospital Tunisia.
- Clement PA, Bluestone CD, Gordts F, et al. Management of rhinosinusitis in children, consensus meeting, Brussels, Belgium. Arch. Otolaryngol. Head Neck Surg. 1998;124:31-4.
- Sobol SE, Marchaud J, Tewfik TL, et al. Orbital complications of sinusitis in children. J Otolaryngol. 2003;31:131-6.
- Froehlich. Acute child ethomoiditis: diagnosis and management of complications. Cah ORL. 2001;35:271-2.
- Klossek JM. Acute and chronic infectious rhinosinusitis, ENT treatment. 2008;239.
- Souldi H, Bouchareb N, Khassime S, et al. Oculo-orbital complications of acute sinusitis at UHC Ibn Rochd, Casablanca, Morocco. J F ORL. 2013;396: 43-4.
- Ben AM, Khalifa Z, Romdhane N, et al. Orbital complications of sinusitis. ENT and CCF, Habib Thameur Hospital Tunis 1008. Jr fr Opht. 2013;36:488-93.
- McHenry CR, Piotrowski JJ, Petrinic D, et al. Determinants of mortality for necrotizing soft-tissue infections. Ann Surg. 1995;22:558-65.